Management of Gastric Residual Volumes: Evidence Based Practice
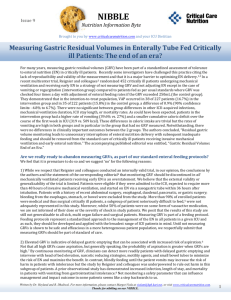
advertisement

Management of Gastric Residual Volumes: Evidence Based Practice By: Lauren Doty, BSN, RN, Alexandria Pipa, BSN, RN, & Nicole Viglietta, BSN, RN Medical Intensive Care Unit Introduction Current Policy at HMC Early enteral feeding for mechanically “Aspiration Precautions” ventilated patients is associated with positive policy number: A-5 A 5 CPMN: effects on gut mucosa integrity, immune *If receiving enteral nutrition: function, infection rates, glycemic control and aspirate stomach contents before overall survival. Not unlike other therapies, enteral nutrition has its risks. The most feared feedings or as ordered. For and talked about complication of enteral continuous tube feedings, if feeding is aspiration. Current practice utilizes gastric g residual exceeds 250 ml,, gastric residual volumes (GRVs) as the main hold feeding and notify physician. marker for risk of aspiration. This practice is neither standardized nor is it universal, with Literature cutoffs ranging from 150ml to 500ml volumes. Because of the positive effects of enteral feeding support, and unsure relationship of GRVs to aspiration, stopping enteral feedings when the GRVs reach an arbitrarily low set cutoff could be harming patients rather than benefiting them. The purpose of this literature review and critique of available studies is to determine the optimal GRV cutoff volume. STUDY Level IC Level IIA PICO Question “For mechanically ventilated adult ICU patients receiving continuous enteral feedings (p), does holding the t b ffeeds tube d ffor GRVs GRV greater t than th 250ml (I), reduce the incidence of aspiration (o) as compared to not holding the tube feeds until residual volumes are greater than 500 ml (c)?” Don’t stop feedings for RV <400-500. Abrupt cessation only with overt regurgitation --Specific statistical findings from the studies reviewed were discussed --No discussion of methods for article selection or leveling criteria A limiti of 500 ml is not associated with adverse effects and can be recommended as a normal limit for GRV --Sample includes 329 patients from 28 ICUs --Blind statistical analysis with significance defined as P <0.05 --No standardization of tube feeding rates or methods for measuring GRV No apparent relationship between residual volume and aspiration was found --Well defined methods --Extensive literature review comparing findings to that of other studies. --Small sample size of only 40 patients. McClave, Snider (2002) REGANE study Pneumonia Chest xx-ray ray --Grade G d B recommendation: only one level I study referenced A id holding Avoid h ldi ffeedings di ffor RV <500 without signs and symptoms of intolerance. North American Summit on Aspiration McClave et al. (2005) Level IIB A non-restricted search of Cinahl, Pro Q Quest, t Ovid, O id Pub P b Med, M d and dC Cochrane h databases was conducted using combinations of the following terms: *gastric residual volumes Implications *enteral nutrition *tube feed residual Practice *aspiration Implementation of an evidence based protocol designed to accept GRVs up Review to 500 ml, with attention being added STRENGTHS WEAKNESSES to the importance of assessing for g of intolerance. signs --Extensive E t i lit. lit review. i --Well defined methodology with specific leveling criteria M Cl McClave ett al.l (2009) SCCM and ASPEN. Level IA Montejo et al. (2010) Normal Chest xx-ray ray FINDINGS Methods Conclusions According to the best evidence available, not withholding feeds until GRVs are > 500 ml does not increase the risk of aspiration as compared to holding tube feeds for residuals >250 ml ml. Patients aspirate with all levels of residual volumes. Attention must therefore shift away from GRV as an important marker of aspiration, to the need for careful assessments for other signs of gastric intolerance, and to the implementation of further methods to reduce aspiration. Research Investigation into the following terms to determine their usefulness in the management of enteral feedings: refractometry testing *refractometry *use of prokinetic agents *use of narcotic antagonists infused through the feeding tube References McClave, S.A., Lukan, J.K., Stefater, J.A., Lowen, C.C., Looney, S.W., Matheson, P.J., . . . Spain, D.A. (2005). Poor validity of residual volumes as a marker for risk of aspiration in critically ill patients. Critical Care Medicine, 33(2), 449-450. doi:10.1097/01.CCM.0000153413.46627.3A. McClave, S. A., Martindale, R. G., Vanek, V.W., McCarthy, M., Roberts, P., Taylor, B., . . . Cresci, G. (2009). Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition ((A.S.P.E.N). ) Journal of Parenteral and Enteral Nutrition, 33(3), 277-316. doi:10.1177/0148607109335234 \ McClave, S.A., Snider, H.L. (2002). Clinical use of gastric residual volumes as a marker for patients on enteral tube feeding. Journal of Parenteral and Enteral Nutrition, 26(6), S43-S50. doi:10.1177/014860710202600607 Montejo, J.C., Minambres, E., Bordeje, L.., Mesejo, A., Acosta, J., Heras, A., . . . Manzanedo, R. (2010). Gastric residual volume during enteral nutrition in ICU patients: the REGANE study. Intensive care med, 36(8), 1386-1393. doi:10.1007/s00134-010-1856-y.