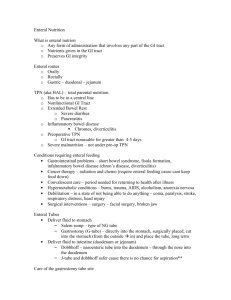
Nutrition Support
advertisement

Enteral and Parenteral Nutrition Presented By: Mr. Sultan Alenazi 1 •Definitions . •Conditions that require nutrition support. •Enteral nutrition access. •Enteral nutrition compositions. •Administration of EN. •Enteral nutrition complications. •Parenteral nutrition access. •Parenteral nutrition solutions. •Administration of PN. •Complications of PN. •Calculations of EN. •Assignment. •Bonus. 2 Nutrition support: is the delivery of formulated enteral and parenteral nutrients to appropriate patients for the purpose of maintaining or restoring nutritional status. Enteral nutrition: the provision of nutrients into the gastrointestinal tract through a tube or catheter when oral intake is inadequate. Also it may include the use of formula as oral supplements or meal replacement. 3 Parenteral nutrition: The provision of nutrients bloodstream intravenously. directly into the 4 The following criteria can be applied to select appropriate patient for nutrition support: Enteral nutrition Parenteral nutrition Should be used in Pt. who have at least Who do not have sufficient 2-3 ft of functional gastrointestinal tract. gastrointestinal function to be able to restore or maintain optimal nutritional status. Who are or will become malnourished. Who are or will become malnourished. In whom oral intake is inadequate to restore or maintain optimal nutritional status. 5 Recommended route of feeding Enteral feeding Condition Typical disorder Impaired nutrient ingestion Neurologic disorders. HIV / AIDS. Facial trauma. Oral or esophageal trauma. Congenital anomalies. Respiratory failure. Cystic fibrosis, Traumatic brain injury. Inadequate oral intake Hyperemesis of pregnancy. Hypermetabolic states such as burns. Comatose states. Anorexia in congestive heart failure, cancer, COPD,ED. Congenital heart disease. Impaired intake after orofacial surgery or injury. Spinal cord injury. Impaired digestion, absorption, metabolism Severe gastroparesis. Inborn errors of metabolism. Crohn’s disease. Short bowel syndrome with minimal resection. Severe wasting or depressed growth. Cystic fibrosis. Failure to thrive. Cancer. Sepsis. Cerebral palsy. Myasthenia gravis. 6 Recommended route of feeding Parenteral nutrition Condition Typical disorder Gastrointestinal incompetency Short bowel syndrome with major resection. Severe acute pancreatitis. Severe inflammatory bowel disease. Small bowel ischemia. Intestinal atresia. Severe liver failure. Major gastrointestinal surgery. Critical illness with poor enteral tolerance or accessibility. Multiorgan system failure. Major trauma or burns. Bone marrow transplant. Acute respiratory failure with ventilator dependency and gastrointestinal malfunction. Severe wasting in renal failure with dialysis. Small bowel transplant, immediate postoperatively. 7 Enteral access: •Nasogastric route. •Nasoduodenal or Nasojejunal route. •Percutaneous Endoscopic Gastrostomy or Jejunostomy. (PEG or PEJ). 8 •For short-term enteral nutrition of 3-4 weeks. •Nasogastric tube passed through the nose into the stomach is appropriate. •Patients with normal gastrointestinal function and gag reflex tolerate this method, which takes advantage of normal digestive, hormonal and bacterial processes in the stomach. 9 •For short-term enteral nutrition of 3-4 weeks in patients with gastric motility disorders, esophageal reflux, or persistent nausea and vomiting. •Nasogastric tube placed postpylorically ( into the small intestine) are appropriate. •The tube passed through the nose and esophagus and inserted into the stomach. The tip of the tube migrates into the small bowel via peristaltic activity. 10 •For patients requiring tube feeding for more than 3 to 4 weeks. •Placing tube directly into the stomach through the abdominal wall by using an endoscope and this tube is endoscopically guided into the stomach (PEG) or the jejunum (PEJ) and then brought out through the abdominal wall to provide the access route for enteral feeding. 11 •A wide variety of enteral feeding products are commercially available. •Formulas are classified in a variety of ways, usually based on protein or overall macronutrients composition. •General purpose formulas are tolerated by most patients and most of these formulas provide 1 kcal / ml. 12 •General formulas that provide 1.5 to 2 kcal / ml are used when it necessary to restrict fluid for patients with cardiopulmonary, renal, and hepatic failure. •High nitrogen formulas are used for patients with increased protein requirements such as those with burns, fistulas, sepsis or trauma. •Disease specific formulas for patients with renal, hepatic or cardiopulmonary disease, metabolic stress, immunosuppression, or glucose intolerance. 13 General purpose / intact (polymeric) Defined / hydrolyzed (monomeric) Semielemental * Use in patients with normal digestion and absorption. * Contain intact protein. * Instituted at full strength ; low viscosity; 300-500 mOsm / kg. * Provide 1-2 kcal / ml. * Lactose free. * 30-40 gm protein / L. • Use in patients with GI compromise. (hydrolyzed nutrients to improve digestion). • Osmolality depends on hydrolysis. • Provide 1-2 kcal / ml. • Lactose free. • 30-45 gm protein / L. Also known as chemically defined, peptide based and elemental formula. • use in patients with limited GI function. • contains free amino acids, minimal fat and minimal residue. • hyperosmolar and low viscosity. • provide 1 kcal / ml. •40 gm protein / L. Also known as free amino acid formula. 14 Disease specific Redehydration Modular •Designed for specific organ dysfunction or metabolic disorder. • May not nutritionally complete. • Most are hyperosmolar. • For patient requiring an optimal ratio of simple carbohydrate to electrolytes for the purpose of maximizing fluid and electrolyte absorption and rehydration. • Formula providing protein, fat or carbohydrate as single nutrients to alter the nutrient composition of commercial formulas or food. 15 The three common methods of tube feeding administration are : 1. Bolus feeding: infusion of up to 5oo ml of enteral formula into the stomach over 5 to 20 minutes usually by large-bore syringe . 2. Intermittent drip feeding: administered of enteral feeding at specified times throughout the day; generally in smaller volume and at a slower rate than a bolus feeding but in large volume and faster rate than continuous feeding. 16 3. Continuous drip feeding: administered of enteral formula into the gastrointestinal tract via pump, usually over 8 to 24 hours of day. 17 Access problems: • Pressure necrosis / ulceration / stenosis. • Tube displacement / migration. • Tube obstruction. • leakage from ostomy / stoma site. Administration problems: • Regurgitation. • Aspiration. • Microbial contamination. 18 Gastrointestinal complications: • Nausea / vomiting. • Distention / cramping. • Delayed gastric emptying. • Constipation. • High gastric residuals. • Diarrhea. Metabolic complications: •Refeeding syndrome. • Drug-nutrient interactions. • Glucose intolerance / hyperglycemia / hypoglycemia. • Dehydration / overhydration. • Hypernatremia / hyponatremia. •Hyperkalemia / hypokalemia. •Hyperphosphatemia / hypophosphatemia . • Micronutrients deficiencies. 19 Parenteral access: • Peripheral access. • Central access. 20 •Peripheral access refers to catheter tip placement in a small vein typically in the arm. • PPN is short-term therapy with minimal impact on nutritional status than TPN. • PPN can be used as a supplemental feeding or in transitional phase to enteral or oral feeding. 21 • PPN veins can’t tolerated concentrated solutions; therefore, diluted larger-volume infusions are often necessary to meet nutritional requirements. • Nutrient solutions not exceeding 800 to 900 mOsm per kg of solvent can be infused through a peripheral intravenous catheter. 22 • Central access refers to catheter tip placement in a large, high blood flow vein such as the superior vena cava. 23 Protein: * Standard solutions: are composed of both essential and nonessential crystalline amino acids. * Specialized solutions: with adjusted amino acid content for patient with hypermetabolism or renal or liver disease. -The concentration of A.A. in these solutions ranges from 3% to 15%. Thus, 10% solution of A.A. supplies 100 gm of protein / L . -The caloric content of A.A. solutions is approximately 4 kcal / gm protein provided. 24 • CHO supplied as dextrose monohydrate in concentration from 5% to 70%. • Dextrose monohydrate yields 3.4 calories / gm. • Maximal rates of CHO administration should not exceed 5 mg / kg / min. 25 • Lipid emulsions composed of aqueous suspensions of soybean or safflower oil with egg yolk phospholipid as the emulsifier. The three carbon molecule, glycerol, which is water soluble, is added to the emulsion to provide osmolarity. •Lipid emulsions are available in 10% and 20% concentrations. • A 10% emulsion provides 1.1 kcal / ml. • A 20% emulsion provides 2 kcal / ml. • Maximal dosage of lipid should not exceed 2 gm / kg of body weight daily. 26 • The recommendations of vitamins and trace element are lower than the DRIs, because parenterally administered of these elements do not go through the digestive and absorptive processes. • Parenteral solutions also represent a significant portion of total daily fluid and electrolyte intake. • The choice of the salt form of electrolytes (chloride, acetate) has an impact on acid-base balance. • Iron is not normally part of parenteral infusions, when needed it is given separately. 27 • Maximum volumes of TPN rarely exceed 3 L daily, with typical prescriptions of 1.5 to 3 L daily. • Patient with cardiopulmonary, renal and hepatic failure needs carefully monitoring. 28 Continuous infusion (hourly): Parenteral solutions are usually initiated below the goal infusion rate and then increased incrementally over 2 0r 3 day period to attain the goal infusion rate. Cyclic infusion (cyclic total parenteral nutrition): Administration of TPN solution for 12 to 18 consecutive hours, usually at night, followed by 6 to 12 hour period of no infusion. 29 Mechanical complications: 1- Pneumothorax. 2- Hemothorax. 3- Hydrothorax. 4- Tension pneumothorax. 5- Subcutaneous emphysema. 6- Branchial plexus injury. 7- Subclavian artery injury. 8- subclavian hematoma. 9- Central vein thrombophlebitis. 10- Arteriovenous fistula. 11- Thoracic duct injury. 12- Hydromediastinum. 13- Air embolism. 14- Catheter fragment embolism. 15- Catheter misplacement. 16- Cardiac perforation. 17- Endocarditis. 30 1- Catheter entrance site: * Contamination during insertion. * Long-term catheter placement. 2- Catheter seeding from bloodborne or distant infection. 3- Solutions contaminations. 31 1- Dehydration from osmotic diuresis. 2-Hyperosmolar, nonketonic, hyperglycemia and hypoglycemia. 3- Hypomagnesemia. 4- Hypocalcemia and hypercalcemia. 5- Hypophosphatemia and hyperphosphatemia. 6- Hyperchloremic metabolic acidosis. 7- Uremia. 8- Hyperammonemia. 10- Electrolyte imbalance. 11- Trace mineral deficiencies. 12- Essential fatty acid deficiency. 13- Hyperlipidemia. 32 1- Cholestasis. 2- Hepatic abnormalities. 3- Gastrointestinal villous atrophy. 33 34 You have male patient old 45 years diagnosed as hypertensive, his Wt. is 65 kg and Ht. is 160 cm. Write complete SOAP note with food menu? You have female patient old 35 years diagnosed as dysphagia, her Wt. 45 kg and Ht. is 150 cm. She needs enteral feeding. With calculating kcal & protein from formula, also flushing water needed : 1- Calculate continues feeding rate ? 2- Calculate bolus feeding rate?( Q6 hrs., Q4 hrs., Q3 hrs. and Q8 hrs.) 3- If patient needs Beneprotein or Benefiber. Calculate how much grams of both that pt. needs? * Types of formula are Ensure & Jevity. 35 Define the following diseases and conditions: •Refeeding syndrome. •Dehydration and Overhydration. •Hypernatremia and Hyponatremia. •Hyperkalemia and Hypokalemia. •Osmolality and Osmolarity. •Cholestasis. •Cystic fibrosis. •Macronutrients and Micronutrients. •Cerebral palsy. •Sepsis. •Fistula. 36