Chapter 9 notes
advertisement

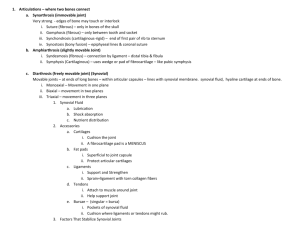
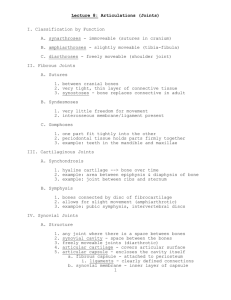
1 Chapter 9: Articulations (Joints) •Point of contact between •Joints structure determines how it functions •The closer the fit at the point of contact the stronger the joint. •Joints are the weakest points of the skeleton JOINTS CLASSIFIED BY: FUNCTIONAL: (table 9-1) •Synarthroses – immovable joints •Amphiarthroses – slightly immovable joints •Diarthroses – freely immovable joints STRUCTURAL: (table 9-2) •Bony fusion: No joint cavity •Fibrous: No joint cavity •Cartilaginous: No joint cavity •Synovial: Has joint cavity Synarthroses: Bones are held tightly together by fibrous connective tissue 1. Suture: a) Synostoses (considered a 4th type) 2. Synchondroses: Held together by hyaline cartilage, temporary: permanent: 3. Gomphoses Amphiarthroses: Bones united by cartilage 1. Syndesmoses: bones connected by a ligament 2. Symphyses: hyaline cartilage fused with fibrocartilaginous pad that separates or unites the bones (i.e. pubic symphysis, intervertebral discs) Diarthroses: Freely movable joints 2 -presence of a fluid filled joint (synovial) cavity which has 5 Features: 1.) ARTICULAR CARTILAGE: Thin layer of hyaline that covers articular surface on bone. 2.) SYNOVIAL CAVITY: Feature unique to synovial joints 3.) ARTICULAR CAPSULE: Double-layered membrane that surrounds and encloses the joint. -Outer layer is -Fibers joined to -Inner layer is 4.) SYNOVIAL FLUID: Thick fluid produced by synovial membrane. *Provides *Lubricates joint surfaces *Normally only enough fluid is secreted to form thin film *Fluid dissipates evenly to 5.) REINFORCING LIGAMENTS: - intrinsic - extra/intrcapsular Other items usually present Fatty pads and Menisci (improve the fit) * Capsule and ligaments are richly supplied with Bursae: -tendon sheath *Found where tendons cross joints 3 STABILITY OF SYNOVIAL JOINTS: 1. Shape of articular surface 2. Number and position of ligaments 3. Muscle tone ANGULAR MOVEMENTS: Increase or decrease the angle between two adjoining bones Origin – Insertion – * movements relative to FLEXION: *DORSIFLEXION *PLANTAR FLEXION - EXTENSION: *HYPEREXTENSION - ABDUCTION: ADDUCTION: CIRCUMDUCTION: ROTATION: Special Movements: PRONATION: SUPINATION: Palms up ELEVATION: DEPRESSION: PROTRACTION: Movement in anterior direction (for scapula protraction is synonymous with abduction) 4 RETRACTION: Movement in posterior direction (for scapula retraction is synonymous with adduction) INVERSION: Sole turns EVERSION: Sole turns OPPOSITION: Thumb touches tips of other fingers TYPES OF SYNOVIAL JOINTS: Nonaxial Joints: no axis 1. gliding (plane) joints - between Uniaxial Joints: 1 axis, 1 plane 2. Hinge joints 3. Pivot joints Biaxial Joints: movement in 2 planes, 2 axes 4. Condyloid Joints (ellipsoidal): one articular surface concave and the other convex. 5. Saddle: Triaxial Joints: movement in 3 planes 6. Spheroid (ball & socket): 5 HOMEOSTATIC IMBALANCES Sprain: Strain: Cartilage damage: Dislocation: Subluxation: Bursitis: Tendinitis: Arthritis: 1. osteoarthritis: most common -"wear and tear" arthritis -chronic inflammation causes articular cartilage to degenerate 2. rheumatoid arthritis: autoimmune disease affects small joints: inflammation of synovial membrane which causes abnormal tissue (pannus) to develop over the cartilage Gout: more common in males 6 Intervertebral Articulation - superior and inferiorior articular surfaces create gliding joints for little movement flexion, extension, lateral flexion, rotation Intervetebral discs – pads of fibrocartilage that separate and cushion vertebrae - S1 – L5 to C2 – C3 - annulus fibrosus – tough outer layer of fibrocartilage; connected directly to the the disc bodies of neighboring vertebrae - nucleus pulposus – soft, elastic, gelatinous core; gives resiliency and absorbs shock - Ligaments o o o o o Ant/Post longitudinal ligament Ligamentum flavum – laminae Interspinous ligament Supraspinous ligament – C7 to Sacrum Ligamentum nuchae – C7 to base of skull Shoulder joint (glenohumeral joint) - ball-and-socket diarthrosis joint Glenoid labrum – fibrocartilagenous lip around the glenoid cavity which deepens the socket Stability of this joint are mostly provided by the surrounding musculature and a few ligaments - glenohumeral coracohumeral coracoacromial coracoclavicular acromioclavicular – supports the superior surface of the shoulder Rotator cuff – tendons of these muscles create the stability of the GH joint - supraspinatus - infraspinatus - teres minor - subscapularis Inferior aspect of the capsule is poorly reinforced - dislocations Bursa in the shoulder can become easily inflamed 7 Elbow Joint - hinge joint; flexion/extension of elbow and pronation/supination of the forearm - humeroulnar joint – largest and strongest of this joint; trochlea of the humerus and trochlear notch of the ulna - humeroradial joint – capitulum of the humerus and the head of the radius Stable joint because: 1. the bony surfaces of the humerus and ulna interlock 2. the articular capsule is very thick 3. the capsule is reinforced with strong ligaments - radial collateral ligament – lateral epicondyle and annular ligament annular ligament – binds the head of the radius to the ulna ulnar collateral ligament – medial epicondyle to the coronoid process and olecranon process Hip Joint (coxal joint) - sturdy ball-and-socket joint; permits flex/ext, abd/adduction, circumduction and rotation Acetabular labrum – a thick fibrocartilage rim that deepens the acetabulum Articular capsule is comprised of four broad ligaments: (attach to the intertrochanteric line) - iliofemoral pubofermoral regional thickenings of the capsule ischiofemoral transverse acetabular ligament – creates the inferior border of the capsule Ligamentum teres (ligament of the femoral head) – originates along the transverse acetabular ligament and attached to the femoral head to the fovea capitis (pit) Knee Joint - hinge joint; permits flexion/extension and little rotation Thin articular capsule that is supported by ligaments and tendons Medial and Lateral menisci: 1. act as cushions; shock absorbers 2. conform to the shape of the surface of the femur 3. provide some lateral stability to the joint 8 Stabilizing ligaments: - Tendons of quadriceps muscles converge at the patella. From the level of the patella to the tibia, the patellar ligament (center) and patellar retinaculae (lat/med to patellar lig.) attach to the anterior surface of the tibia - Two popliteal ligaments posteriorly extend from femur to tibia - The anterior and posterior (site of origin on the tibia) cruciate ligaments inside the joint capsule stabilize the joint from sliding anteriorly and posteriorly - Tibial collateral ligament and the fibular collateral ligament support the joint medially and laterally in extension “Locking” the knee will allow a person to stand for prolonged periods of time with out using surrounding musculature Review table 9-3 on page 271 and 9-4 on page 275