Renal tubular reabsorption - College of Veterinary Medicine
advertisement

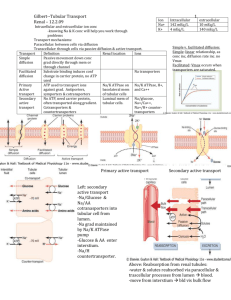
Renal tubular reabsorption Stephen P. DiBartola Department of Veterinary Clinical Sciences College of Veterinary Medicine Ohio State University Columbus OH 43210 What do the kidneys do? The glomeruli “non-discriminantly” filter the blood, and the tubules take back what the body needs leaving the rest as waste to be excreted. Some wastes also can be actively added to the tubular fluid. Renal tubular reabsorption • Excretion refers to the removal of solutes and water from the body in urine • Reabsorption (movement from tubular fluid to peritubular blood) and secretion (movement from peritubular blood to tubular fluid) refer to direction of movement of solutes and water across the renal tubular epithelium Renal tubular reabsorption • The luminal cell membranes are those that face the tubular lumen (“urine” side) • The basolateral cell membranes are those are in contact with the lateral intercellular spaces and peritubular interstitium (“blood” side) Renal tubular reabsorption • The transmembrane potential difference is the electrical potential difference between the inside and outside of the cell • The transepithelial potential difference is the electrical potential difference between the tubular lumen and the peritubular interstitium Renal tubular reabsorption • The term transcellular refers to movement of solutes and water through cells • The term paracellular refers to movement of solutes and water between cells • Epithelial cell junctions can be “leaky” (proximal tubule) or “tight” (distal convoluted tubule, collecting duct) Terminology Transepithelial versus transmembrane potential difference Luminal versus basolateral membranes Transcellular versus paracellular transport Renal tubular reabsorption • Leaky epithelia (proximal) • Tight epithelial (distal) • Small transepithelial concentration difference • Small TEPD • High water permeability • Large transepithelial concentration difference • Large TEPD • Low water permeability Nephro-man says … Just think of it as a six-pack Luminal surface Epithelial tight junctions Basolateral surface Renal tubular reabsorption That renal tubular reabsorption must occur is intuitively obvious because … The fluid filtered into Bowman’s space is an ultrafiltrate of plasma containing many vital small molecular weight solutes (e.g., glucose, amino acids, bicarbonate) but these solutes do not normally appear in urine Renal tubular reabsorption • Solute reaborption in the proximal tubule is isosmotic (water follows solute osmotically and tubular fluid osmolality remains similar to that of plasma) • 65% of water and solute reabsorption occurs in the proximal tubule • 90% of bicarbonate • 99% of glucose & amino acids • Proximal tubules: coarse adjustment • Distal tubules: fine adjustment Cl- goes up because Na+ is reabsorbed with glucose, amino acids, Pi and HCO3Unchanged due to isosmotic reabsorption Glucose, amino acids, Pi and HCO3- go down due to reabsorption with Na+ Secondary active co-transport (glucose, amino acids, phosphate) LUMINAL Glucose, Pi amino acids Na+ HCO3- Na+ + H+ H2CO3 BASOLATERAL 2 K+ 3 Na+ K+ Types of transport processes • • • • • • Passive transport (simple diffusion) Facilitated diffusion Primary active transport Secondary active transport Pinocytosis Solvent drag Passive transport (simple diffusion): Definition • Movement of a substance across a membrane as a result of random molecular motion Passive transport (simple diffusion): Characteristics • No metabolic energy required • Rate of transfer dependent on electrochemical gradient across membrane and membrane permeability characteristics • Rate of transfer linearly related to concentration of diffusion substance (no Vmax) Facilitated diffusion: Definition • Movement of a substance across a membrane down its electrochemical gradient after binding with a specific carrier protein in the membrane Facilitated diffusion: Characteristics • Saturable (has a Vmax) • Structural specificity and affinity of carrier for substance transported • Transfer may occur in either direction across membrane • Does not directly require metabolic energy Facilitated diffusion: Examples • Glucose, amino acids: Basolateral membranes of proximal tubules • Sodium: luminal membranes of proximal tubules Primary active transport: Definition • Movement of a substance across a membrane in combination with a carrier protein but against an electrochemical gradient Primary active transport: Characteristics • Directly requires metabolic energy (i.e. hydrolysis of ATP) • Saturable (has a Vmax) • Structural specificity and affinity of the carrier for the substance transported Primary active transport: Examples • • • • Na+-K+ ATPase H+ ATPase H+-K+ ATPase Ca+2 ATPase Secondary active transport: Definition • Two substances interact with one specific carrier in the cell membrane and both substances are translocated across the membrane • Co-transport Transported substances move in the same direction across the membrane • Counter-transport Transported substances move in opposite directions across the membrane Secondary active transport: Characteristics • “Uphill” transport of one substance is linked to “downhill” transport of another substance • Carrier must be occupied by both substances (or be unoccupied) to be mobile in the membrane • Saturable (has a Vmax) • Demonstrates specificity and affinity of carrier for substance transported • “Uphill” transport occurs without direct input of metabolic energy Secondary active transport: Examples • Glucose, amino acids, or phosphate with sodium in luminal membranes of proximal tubules • Sodium and hydrogen ions in luminal membranes of proximal tubules Secondary active transport • The metabolic energy for secondary active transport of Na+ at the luminal membrane in the proximal tubule comes from Na+-K+ ATPase which transports Na+ out of the cell across the basolateral membrane and maintains a favorable electrochemical gradient for the entry of Na+ at the luminal membrane Secondary active co-transport (glucose, amino acids, phosphate) LUMINAL Glucose, Pi amino acids Na+ HCO3- Na+ + H+ H2CO3 BASOLATERAL 2 K+ 3 Na+ K+ Pinocytosis • Definition: Uptake by cells of particles too large to diffuse through the cell membrane • Example: Reabsorption of filtered proteins in the proximal tubules Solvent drag: Definition • A solvent such as water moving across an epithelium by osmosis can drag dissolved solutes with it Morphologic features of proximal tubular cells • Large surface area for reabsorption of water and solutes (brush border, lateral cellular interdigitations) • Large numbers of mitochondria to provide ATP • Leaky epithelial junctions Routes of transport across proximal tubular epithelium • Paracellular • 1% of surface area • 5-10% of water transfer • Passive diffusion or solvent drag only • Requires favorable electrochemical gradient • Passive diffusion of ions and large nonpolar solutes • Transcellular • 99% of surface area • 90-95% of water transfer • Passive or active transport • All active transport occurs by this route Intrasegmental axial heterogeneity of proximal tubule • P1: sodium, water, bicarbonate, amino acids, glucose, and phosphate reabsorbed • P2: sodium, water and chloride reabsorbed • P3: Organic acids and bases transported Secondary active transport • Glucose, Amino acids • Tmax high and constant (kidney not a regulator of plasma glucose and amino acid concentrations) • Phosphate • Tmax low and altered by PTH (kidney is a regulator of plasma phosphtate concentration) Secondary active transport: Glucose Secondary active transport: Phosphate Na+-K+ ATPase • In renal tubular cells found only in basolateral membrane • When ATP is hydrolyzed, 2 K+ ions are pumped into the cell and 3 Na+ ions are pumped out • Maintains favorable electrochemical gradient for Na+ entry at luminal membrane • Maintains cell membrane potential difference and intracellular osmolality Pinocytosis • Endocytosis: Filtered proteins adsorbed to sites on luminal membranes that are internalized to form endosomes. Fusion with lysosomes forms endolysosomes in which digestion of proteins occurs • Hydrolysis of filtered proteins to constituent amino acids by enzymes in brush border of proximal tubular cells Urea: Passive diffusion • Urea is passively reabsorbed in the proximal tubule • More urea is reabsorbed at low tubular flow rates than at high tubular flow rates • Contributes to BUN increasing out of proportion to creatinine in dehydrated patients even before GFR decreases Calcium homeostasis • 99% of Ca+2 in bone, < 1% intracellular, 0.1% extracellular • Much homeostasis achieved by altering GI absorption via calcitriol • Only 60% of plasma Ca+2 (ionized and complexed) is available for glomerular filtration Renal handling of Ca+2 • Filtered by glomeruli and reabsorbed by tubules • 99% of filtered Ca+2 is reabsorbed (exception: horse) • Proximal tubule: 60-65% • Loop of Henle: 25-30% • Distal tubule & collecting duct: 4-9% Renal reabsorption of Ca+2 • Proximal tubule, medullary thick ascending loop of Henle: passive and paracellular (favorable electrochemical gradient) • Distal nephron: active and transcellular • Ca+2 diffuses down electrochemical gradient at luminal membrane • Transported across basolateral membrane by Na+-Ca+2 antiporter and Ca+2 ATPase Factors affecting renal Ca+2 reabsorption • Proximal tubule: Ca+2 reabsorption parallels Na+ and water reabsorption • Increased by volume depletion • Decreased by volume expansion Factors affecting renal Ca+2 reabsorption • Increased serum Pi stimulates PTH release (via decreased serum Ca+2) • PTH increases Ca+2 reabsorption and decreases Pi reabsorption in kidney • Allows retention of Ca+2 but excretion of Pi mobilized from bone by PTH and absorbed from gut via calcitriol Factors affecting renal Ca+2 reabsorption • Metabolic acidosis stimulates Ca+2 reabsorption in distal tubules • Metabolic alkalosis inhibits Ca+2 reabsorption in distal tubules Renal handling of phosphate • Filtered by glomeruli and reabsorbed by tubules but not secreted • 75-95% of the filtered load of Pi is reabsorbed in the proximal tubule by co-transport with Na+ Renal handling of phosphate • Pi-rich meal will increase serum Pi and filtered load with consequent increase in urinary Pi excretion • Increased serum Pi will increase PTH (via decreased serum Ca+2) which will decrease Tmax for Pi reabsorption in proximal tubule and increase urinary Pi excretion