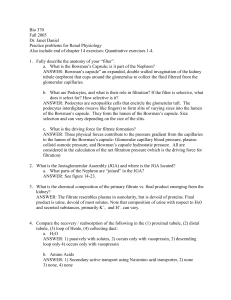
Urinary System and Renal Physiology Functions of the Urinary System 1) Regulate plasma ionic composition (Na+, K+, etc) 2) Regulate plasma volume 3) Regulate plasma osmolarity (solute concentration) 4) Regulate plasma pH 5) Remove metabolic waste products and foreign substances from plasma 6) Hormone secretion a) Erythropoietin- increase red blood cell production b) Renin- role in aldosterone production (Na+ balance)— more later Blood Supply to Kidneys ➢Kidneys are primarily a blood (plasma) filter 1) Receive 20% of cardiac output at rest a) Very large flow of blood b) Less than 1% of body weight c) Utilize 16% of ATP usage by body -- ATP used for active transport – Blood supply via renal arteries Microscopic Anatomy of the Kidney Uriniferous Tubules = functional units ✓ About 1 million per kidney Uriniferous tubules consist of: 1) Nephrons- each with 2 main parts a) Renal corpuscle i. ii. Glomerulus Glomerular (Bowman’s) Capsule b) Renal tubule- long tube divided into several specialized regions 2) Collecting Ducts Renal Corpuscle of Nephron 1) Glomerulus = twisted ball of blood capillaries a) Where plasma is filtered from blood and enters into tubule system b) Blood enters glomerulus from afferent arterioles, some of the plasma is filtered, rest of blood leaves glomerulus through efferent arterioles c) Efferent arterioles then form another capillary network which surrounds the tubular portion of nephron = peritubular capillaries 2) Glomerular (Bowman’s) capsule = inflow end of renal tubule a) Where filtered plasma enters into tubule Renal Corpuscle Peritubular Capillaries Renal Tubules of Nephron 1) Proximal Convoluted Tubule 2) Loop of Henle a) Descending limb b) Thin ascending limb c) Thick ascending limb 3) Distal Convoluted Tubule 4) Collecting Duct Anatomy of a Nephron Figure 19.3 Four Basic Processes in the Formation of Urine 1) Glomerular filtration – filtration of plasma from glomerulus into Bowman’s capsule 2) Reabsorption – movement of substances from tubules back into blood (peritubular capillaries) 3) Secretion – movement of substances from peritubular capillaries directly into tubules 4) Excretion – from tubules out of body Basic Renal Processes Figure 19.7 1) Primary function of the kidneys is to filter blood 2) Filtrate has a similar composition to plasma minus the plasma proteins 3) Initially, composition of ions and small molecules same as plasma (changes as filtrate passes through renal tubules) 4) Only about 20% of plasma passing through each kidney is filtered a) However, still results in large volume filtered each day Glomerular Filtration (GFR) Rate of filtration is known as Glomerular Filtration Rate = GFR GFR = 125 mL/min or 180 liters/day Regulation of GFR 1) 180 liters fluid filtered/day a) Only 1.5 liters urine excreted/day (<1%) b) >99% of filtered fluid is reabsorbed 2) Small increase in GFR → large increase volume fluid filtered and excreted 3) Because of this, GFR is highly regulated ➢GFR is primarily dependent on 2 factors: 1. Blood pressure in glomerular capillaries a) Forces plasma out of capillaries into Bowman’s space b) Primary force affecting GFR 2. Osmotic force of plasma (due to plasma proteins) a) Water tends to remain in capillaries unless forced out b) Decreasing osmotic force increases GFR Glomerular Blood Pressure (BP) is Primary Force Producing Filtration 1) Increase BP 2) Decrease BP increase in filtration decrease in filtration • Glomerular BP affected by blood flow through afferent arterioles 1) Dilate afferent arteriole– increases blood flow into glomerulus increases BP in glomerular capillaries 2) Constrict afferent arteriole– decrease blood flow into glomerulus decrease BP 1) Afferent arterioles (and to lesser extent, efferent arterioles) are controlled by both 1) local messenger molecules within the kidney and 2) by the sympathetic nervous system ✓ Tubuloglomerular Feedback (local control) a) If there is a decrease in fluid in kidney tubules, vasodilating molecules are released by tubule cells; dilate afferent arterioles increases BP in glomerulus and increases GFR (more fluid filtered) b) If increased fluid in tubules, vasoconstricting molecules are released which constrict afferent arterioles and decreases GFR (less filtered) ➢ Maintains a relatively constant GFR and fluid level in tubules Sympathetic Control of GFR 1) Decreases in BP can decrease GFR a) Baroreceptor reflex increases sympathetic stimulation of afferent arterioles b) Causes vasocontriction c) Reduces blood flow into glomerular capillaries which decreases GFR (less filtered) d) Conserves fluid in plasma to increase blood volume and increase BP -- Example: blood loss due to hemorrhage Reabsorption Movement of substances from renal tubules into peritubular capillaries (substances returned to the blood) 1) Most occurs in proximal convoluted tubule 2) Some in distal convoluted tubule 3) Barrier for reabsorption a) Epithelial cells of renal tubules b) Endothelial cells of capillary (minimal) Reabsorption Barrier Figure 19.13 Solute and Water Reabsorption Dependent on transport proteins and membrane permeability to water Figure 19.14c Rates of Reabsorption of Water and Select Solutes (Don’t memorize values from Table 19.1) lymphocyte Table 19.1 Reabsorption in Proximal Convoluted Tubule (PCT) Molecules reabsorbed include (but not limited to): 1) Glucose Normally, 100% reabsorbed from tubule in PCT 2) Amino acids 3) Sodium 4) Calcium 5) Urea (from protein degradation) 6) Water: approx 65% of filtered water is reabsorbed in PCT ✓ Water is reabsorbed due to osmotic gradient produced by the reabsorption of other solutes Example: Reabsorption of Glucose and Amino Acids 1) Glucose and amino acids are co-transported with sodium (secondary active transporters) into PCT cells 2) These transporters can be saturated so that above a certain filtrate concentration, no further re-absorption occurs remainder lost in urine 3) Rate of transport when carrier proteins are saturated = transport maximum or Tmax Example: Glucose Reabsorption 1) Normal plasma glucose = 100 mg/100 ml plasma 2) Freely filtered at glomerulus, so concentration in filtrate is same as plasma concentration 3) Normally 100% actively reabsorbed in proximal convoluted tubule 4) Normally, zero glucose in urine 5) Tmax for glucose = 375 mg/100 ml filtrate (normal plasma glucose is well below the Tmax ) Diabetes mellitus 1) During diabetes mellitus, plasma glucose can be as high as 600 mg/100 ml plasma 2) Glucose concentration now exceeds Tmax 3) In this case, an amount of glucose = 225 mg/100 ml (600 mg/100 ml – 375 mg/100 ml) will remain in PCT and be excreted in urine a) Makes the urine sweet: mellitus = “sweet” Descending Loop of Henle 1) Mostly involved in water reabsorption 2) 15% of filtered water reabsorbed 3) Little solute reabsorption a) Concentrates the fluid in tubule Ascending Loop of Henle 1) Mostly involved with sodium and chloride reabsorption; no (little) water reabsorption 2) Thin portion of loop: passive sodium channels on tubule cells (depends on concentration gradient) 3) Thick portion: secondary active transporter for sodium, potassium, and chloride a) Known as the NK2C transporter (transports 1 Na+, 1 K+, and 2 Clfrom filtrate into the tubule cells Na+ pumped out of cell and reabsorbed into peritubular capillaries (blood) Na+ Impermeable to water Distal Convoluted Tubule (DCT) ➢ Involved with regulated sodium reabsorption: ✓Dependent on the hormone Aldosterone 1) Aldosterone secreted by cells in adrenal gland cortex 2) Part of RAAS system a) Renin, Angiotensin, Aldosterone System 3) Renin = hormone secreted by kidney in response to low plasma sodium or low plasma/extracellular fluid volume Renin-Angiotensin-Aldosterone System *In kidney; in walls of afferent arterioles = granular cells To kidney ACE = Angiotensin Converting Enzyme Figure 20.15 ✓ Aldosterone increases reabsorption of sodium from Distal Convoluted Tubule (DCT) 1) Aldosterone increases the number of sodium channels and Na+/K+ ATPase transporters (pumps) • Able to transport more sodium from tubule and return it to peritubular capillaries Na+ channels Collecting Duct 1) Some reabsorption of sodium (dependent on aldosterone) 2) Mostly involved with water reabsorption 3) Water reabsorption in collecting duct dependent on the hormone anti-diuretic hormone (ADH, vasopressin) 4) ADH inserts water channels (aquaporins) into membrane of collecting duct cells 1) Allows water to move from tubule into cells and then back into peritubular capillaries 2) Without ADH, water cannot pass through the membrane of these cells 1) ADH produced in hypothalamus (released from posterior pituitary gland) 2) ADH secreted in response to low extracellular fluid (ECF) volume and/or increased ECF osmolarity 3) Allows water reabsorption to increase plasma/ECF fluid volume (i.e. conserve body water) 4) Without ADH, water remains in tubules and is excreted in urine (lost from body)- more later Nephron Secretion 1) Solute moves from peritubular capillaries into tubules 2) Barriers same as for reabsorption 3) Transport mechanisms same but opposite direction – Secreted Substances: a) Potassium b) Hydrogen ions (helps regulate pH) c) Penicillin • Highly efficient- penicillin has short half life in plasma Formation of Concentrated vs. Dilute Urine ➢Kidneys regulate volume of water in body 1) Increased volume of extracellular fluid excrete large volume of dilute urine 2) Decreased volume excrete small volume of concentrated urine to conserve body water Osmosis Water diffuses down concentration gradient 1) Water moves from low [solute] to high [solute] 2) Water reabsorption follows solute reabsorption Water Reabsorption 1) Proximal tubules a) 70% filtered water is reabsorbed b) Not regulated 2) Desending Loop of Henle a) 15% filtered water is reabsorbed b) Not regulated 3) Distal tubules and Collecting ducts a) Most remaining water is reabsorbed b) Regulated by ADH Medullary Osmotic Gradient for Water Reabsorption 1) Gradient critical for water reabsorption 2) Osmolarity of body fluids = 300 mOsm 3) Osmolarity of interstitial fluid of renal medulla varies with depth a) Lower osmolarity near cortex b) Greater osmolarity deep in medulla Osmotic Gradients – cont. 1) Fluid in distal tubule - 100 mOsm 2) interstitial fluid of medulla – gradient up to 1400 mOsm ➢Large osmotic gradient in interstitial fluid favors reabsorption of water from tubule by osmosis Osmotic Gradients of Late Distal Tubule and Collecting Ducts If epithelium impermeable to water, then no reabsorption occurs If permeable, water will move by osmosis and be reabsorbed back into blood Figure 20.9a Water Reabsorption in Distal Tubules and Collecting Ducts 1) Dependent on epithelium permeability to water 2) Water permeability dependent on water channels a) Aquaporin-2: present in apical membrane only when ADH present in blood Permeable Membrane in Presence of ADH 1) ADH stimulates insertion of water channels (aquaporin-2) into apical membrane. a) Water can permeate membrane and be reabsorbed by osmosis 2) Excrete small volume of concentrated urine 3) Max osmolarity urine = 1400 mOsm Figure 20.9b Without ADH, 1) No water reabsorption; water remains in tubule 2) Excrete large volume of dilute urine 3) Reduces total body volume