Gastro23-AccessoryOrgans
advertisement

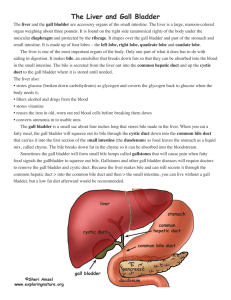
Checked by Dr. Roque GI #23 Fri, 02/21/03, 1pm Dr. Roque Jennifer Uxer for Kelly Thurmon Page 1 of 5 HA: Accessory Organs Liver, Gall Bladder, Pancreas, and Spleen I. Spleen isn’t part of the digestive system, but is associated with the other organs. It’s actually a part of the lymphatic system. I like to think of it as the cemetery of red blood cells. Diseases resulting in increased destruction of rbc can lead to splenomegaly, or enlargement of the spleen. Liver A. Surfaces [N270] 1. Diaphragmatic surface Associated with the diaphragm Mainly found on the right hypochondriac side but does extend to the left Smooth 2. Visceral surface Faces posteriorly and inferiorly Bare Area of the Liver: an area of the liver that’s not covered with peritoneum Contains H-shaped fissures and gall bladder bed. LEARN THE HSHAPED structures! Refer to the power points and Netter for pictures. 1. Horizontal fissure (left to right): Porta hepatis-”doorway” for passage of blood vessels, bile ducts, nerves, and lymphatics to enter and exit the liver. It’s basically a depression. 2. 2 vertical arms: Gall bladder is located here. 3. Superior to gall bladder is the inferior vena cava. 4. Opposite the gall bladder: Another fissure contains the falciform ligament and a fetal structure, the Ligamentum teres hepatis (round lig. of liver)-obliterated umbilical v. It is found in the umbilical cord during development. 5. Superior to ligamentum teres hepatic: Ligamentum venosum— obliterated ductus venosus; a fibrous cord that’s difficult to dissect This is synonymous to the ductus arteriosus in the heart which shunts blood from the pulmonary artery to the aorta because the lungs are not functional. The ductus venosus shunts blood from the portal v. to the inferior vena cava because the liver is non-functional for digestive functions. In the mother, blood goes from the umbilical vein (Ligamentum teres hepatis) → portal vein → ligamentum venosum → inferior vena cava → heart. This sequence prevents most of the blood from passing through the liver in the fetus. 75% of the blood to the liver in the adult is derived from the portal vein. Blood travels through the parenchyma of the liver to the inferior vena cava which takes it to the right atrium. Checked by Dr. Roque GI #23 Fri, 02/21/03, 1pm Dr. Roque Jennifer Uxer for Kelly Thurmon Page 2 of 5 B. Lobes [N270, N272]—BE ABLE TO ID ALL THE STRUCTURES Lobes are important especially in liver transplanation. Entire liver-organ transplants are difficult to do because of few donors, so part of it, a lobe, can be replaced. Classified by how they look and by their functions. The H-shaped structure allows for further subdivision of the lobes 1. Classical lobes—divided by falciform ligament: Right lobe-to the right of the falciform ligament right lobe—to the right of the gall bladder, quadrate lobe—adjacent to the gall bladder and quadrangular in shape, caudate lobe—more posterior lobe and associated with the inferior vena cava Left lobe—to the left of the falciform ligament 2. Functional lobes—based on blood supply and bile drainage; if you take a part out of the functional right lobe or the left lobe, it won’t be a problem because the remaining part is functionally the same. Right lobe—right lobe, caudate process (of caudate lobe) which connects the caudate lobe to the right lobe. Right hepatic artery and vein and the right bile duct also serve the caudate process. Left lobe—left lobe, quadrate lobe, caudate lobe (except the caudate process) C. Ligaments of the Liver [N270] These help support the liver. 1. Falciform ligament—contains ligamentum teres hepatis and paraumbilical veins on free border 2. Coronary ligaments—put your finger on the liver’s surface and push it over the top to the back as far as possible. The coronary ligament stops it. These lie between the diaphragm and the liver and form the posterior boundary of the subphrenic recesses. There are 2 subphrenic recesses: one on the right and one of the left, separated by the falciform ligament. 3. Right and left triangular ligaments 4. Lesser omentum D. Biliary Drainage [N276, N278]—VERY IMPORTANT!!! 1. Hepatic ducts—right and left drain the functional right and left liver lobes, respectively 2. Common hepatic duct—right + left hepatic ducts 3. Common bile duct—common hepatic duct + cystic duct (duct of the gall bladder) 4. Hepatopancreatic ampulla (ampulla of Vater)—common bile duct + main pancreatic duct; opens into major duodenal papilla of duodenum (2nd part) They join within the wall of the second part of the duodenum. This is an important landmark. It demarcates the boundary of the foregut and midgut derivatives. Bile is made in the liver and must be moved to the gall bladder for concentration and storage. A group of sphincters prevents bile from flowing Checked by Dr. Roque II. III. GI #23 Fri, 02/21/03, 1pm Dr. Roque Jennifer Uxer for Kelly Thurmon Page 3 of 5 directly into the duodenum at any time, instead it gets stored in the gall bladder. These are collectively the Sphincter of the hepatopancreatic ampulla (sphincter of Oddi). This includes the bile duct sphincter, pancreatic sphincter, and sphincter ampulla. Fat is present in the duodenum → hormones secreted → gall bladder contracts → sphincters relax → bile flows from gall bladder into duodenum Dissecting this and the blood vessels is difficult. Always start at the hepatoduodenal ligament (lesser omentum, connects liver to duodenal bulb, location of epiploic foramen & lesser sac). There are 3 structures here: common bile duct (always to the right), hepatic artery proper (always to the left), and hepatic portal vein (always behind/posterior). They are the anterior part of the epiploic foramen. The inferior vena cava is in the posterior wall of the epiploic foramen. Gall Bladder and Cystic Duct [N276] 1. Fundus—tip of 9th costal cartilages and linea semilunaris. It’s related to the transverse colon. 2. Body—contacts visceral surface of the liver and 1st part of duodenum 3. Neck—may contain sacculation (Hartmann’s pouch); mucosa is thrown into folds (spiral valve of Heister). Connects to the cystic duct. 4. Cystic duct—mucosa forms spiral fold There is an infundibulum, but it’s believed to be a post-mortem development. If a gall bladder stone (cholelethiasis) perforates posteriorly, it can penetrate different organs. If it perforates in the fundus, it goes into the transverse colon. There’s no obstruction because the colon’s big. If it perforates in the body, the stone can get into the duodenum where the diameter’s smaller and can cause an obstruction, especially in the ileocecal valve or duodenal-jejunal flexure. Pancreas Looks like a small gun pointing to the left and slightlyly up. The handle is below the level of the barrel and the barrel points to the spleen. The trigger is formed by the superior and inferior mesenteric arteries and veins. A. Parts 1. Head—common bile duct posteriorly; superior mesenteric vessels anteriorly; contains uncinate process 2. Neck 3. Body—omental tuberosity marks the location of the celiac trunk The neck and body are found in the transpyloric plane at L1. 4. Tail—contacts hilum of the spleen—found at T12 and shouldn’t be seen at L1 B. Ducts 1. Major pancreatic duct (of Wirsung)—opens into major duodenal papilla with the common bile duct; contains pancreatic sphincter 2. Minor (accessory) duct (of Santorini)—may open into minor duodenal papilla. C. Exocrine & Endocrine Checked by Dr. Roque GI #23 Fri, 02/21/03, 1pm Dr. Roque Jennifer Uxer for Kelly Thurmon Page 4 of 5 Exocrine because it has a set of ducts Endocrine because it secretes hormones—insulin and glucagon, among others. Islets of Langerhans make insulin, which is deficient in diabetes. IV. Spleen—cemetery of RBCs Lymphatic organ Enlarged—splenomegaly—in many diseases, especially those that cause blood problems (i.e. malaria) Also enlarged in portal hypertension Related to left 9th, 10th, 11rth ribs; 10th rib lies along axis of spleen. If there’s a stab wound/penetrating injury in the left hypochondria, the spleen can be injured. It’s also frequently injured in car accidents involving fractured ribs, which lacerate the spleen, and cause profuse bleeding into the abdominal cavity. Completely peritonealized Rests on left colic flexure and phrenicocolic ligament Attached to left kidney via lienorenal ligament Attached to left border of stomach via gastrosplenic ligament Tail of pancreas abuts the hilum of the spleen. The stomach is also related to the spleen. The kidney is behind it, and the transverse colon is below it. Don’t worry about the ligaments of the spleen. Blood Supply, Lymphatics and Innervation of the GIT Embryology Must understand embryology to understand the blood supply and innervations. 3 parts in development 1. Foregut: esophagus, stomach, part of duodenum. Ends at level of major duodenal papilla—the place the common bile duct enters—is the junction of the foregut and midgut. Supplied by the celiac artery and its branches. (Structures include liver, pancreas, gall bladder, stomach, and part of the duodenum) 2. Midgut: junction between the midgut and the hindgut is the junction of the proximal 2/3 and the distal 1/3 of the transverse colon. Supplied by the superior mesenteric artery branches. (Structures include duodenum distal to major duodenal papilla, part of the pancreas, ileum, jejunum, ascending and transverse colon, cecum, and appendix) 3. Hindgut: Supplied by the inferior mesenteric artery. Structures include transverse colon, rectum, sigmoid colon, and descending colon. Aortic branches Aorta has 3 main branches—We’ll have to ID the main branches of each. 1. Celiac (very short)—3 branches (foregut) C1. Common hepatic artery (to the left)—2 branches CHA1. Gastroduodenal artery (down)—behind the duodenal bulb (reason a posterior erosion of the duodenal bulb hits the gastroduodenal artery); has 2 branches Checked by Dr. Roque GI #23 Fri, 02/21/03, 1pm Dr. Roque Jennifer Uxer for Kelly Thurmon Page 5 of 5 GA1. Right gastroepiploic artery—supplies greater curvature of the stomach GA2. Superior pancreatical duodenal artery CHA2. Hepatic artery proper (up)—3 branches—supplies liver, gall bladder, and stomach. HAP1. Right Hepatic artery—mainly supplies liver; has 1 branch RHA1. Cystic artery—supplies gall bladder HAP2. Left Hepatic artery—mainly supplies liver HAP3. Right gastric artery—supplies stomach C2. Left gastric artery (travels up) C3. Splenic artery (down & to the right)—travels behind the pancreas to get to the spleen, eroded in gastric ulcer, SA1. Gives off Short Gastric branches that supply the fundus of the stomach SA2. Left gastro-epiploic artery SA3. Gives of branches to supply the pancreas—pancreatic arteries 2. Superior mesenteric 3. Inferior mesenteric Blood supply to stomach Stomach has a greater and lesser curvature Lesser curvature—continuous vessel: left (from the superior direction) and right gastric (inferior direction) artery anastomose to form a continuous blood vessel in the lesser omentum Greater curvature—continuous vessel: left (superior) and right (inferior) gastroepiploic arteries anastomose to form a continuous blood vessel Fundus is supplied by the short gastric arteries from the splenic artery All the branches give off branches to supply the stomach. So, if you lose 1 blood supply, other branches from the celiac artery will supply that area.