Pro6.4-E-04 CSF SOP
advertisement

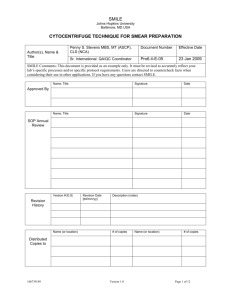
SMILE Johns Hopkins University Baltimore, MD USA CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL Author(s), Name & Title Penny S. Stevens MBS, MT (ASCP), CLS (NCA) Document Number Effective Date Sr. International QA/QC Coordinator Pro64-E-04 23 Jan 2009 SMILE Comments: This document is provided as an example only. It must be revised to accurately reflect your lab’s specific processes and/or specific protocol requirements. Users are directed to countercheck facts when considering their use in other applications. If you have any questions contact SMILE. Name, Title Signature Date Name, Title Signature Date Approved By SOP Annual Review Version # [0.0] Revision History Name (or location) Revision Date [dd/mm/yy] Description (notes) # of copies Name (or location) # of copies Distributed Copies to 533572427 Version 1.0 Page 1 of 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL I acknowledge that I have read, understand and agree to follow this SOP. Name (print) 533572427 Signature Version 1.0 Date Page 2 of 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL I. PRINCIPLE: 1. Cerebrospinal Fluid, also called CSF, is the product of the secretory activity of the choroid plexus. It is the third major fluid of the body and supplies nutrients to the nervous tissue, removes metabolic waste, and protects the brain and spinal cord from trauma. 2. CSF examination is requested when the physician suspects: a. b. c. d. II. DEFINITIONS 1. 2. 3. 4. 5. 6. III. Meningitis, encephalitis, syphilis, or abscess infections. Multiple Sclerosis, Leukemia, and Demylelinating diseases Hemorrhage Brain or spinal cord tumors CBC - Complete Blood Count CSF - Cerebrospinal Fluid LIS - Laboratory Information System QC - Quality Control RBC - Red Blood Cell WBC - White Blood Cell SPECIMENS: 1. Cerebrospinal Fluid: a. A physician obtains CSF by lumbar puncture and always under aseptic conditions. b. It is a routine practice to collect three (3) sterile tubes of CSF (1-5 ml per tube) for analysis. 2. Tubes should be collected and labeled sequentially by the physician at the time of collection. All tubes must be labeled properly and delivered immediately to the following sections: a. b. c. d. 533572427 Tube #1: To Chemistry for protein and glucose or serology study. Tube #2: To Microbiology for culture and gram stain. Tube #3: To Hematology for cell count and differential If only one tube is collected, perform testing in the following order to preserve specimen and avoid contamination: i. Microbiology - culture and gram stain. ii. Hematology - cell count and differential. iii. Chemistry Version 1.0 Page 3 of 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL 3. Cell lysis can begin within one (1) hour of collection so prompt delivery to the laboratory is critical. 4. Specimens must be handled as STAT. If possible, notify laboratory personnel before specimen collection to ensure staff is ready for testing immediately after collection. 5. Always deliver specimens to laboratory personnel by hand - never drop specimens off or leave unattended. 6. Clotted specimens are not satisfactory for testing. a. If the specimen is clotted, the cell count can not be performed. Notify the physician immediately. b. Prepare a Cytocentrifuge smear and review for malignant cells. Do not perform or report a manual differential. c. Document actions taken and all notification in the LIS and on the CSF worksheet. 7. Never run a body fluid through the CBC automated counting instrument. Cell counts are performed manually using a hemocytometer. 8. Hematology specimens are retained for 7 days at 2-8°C in the hematology refrigerator in the container marked "Fluids". If specimens are transferred for additional testing, they will be stored in the transfer departments as required by department procedure. IV. EQUIPMENT & REAGENTS 1. Equipment: a. b. c. d. e. f. g. h. i. j. k. 533572427 Neubauer Hemocytometer Neubauer Hemocytometer specific coverslip Capillary pipettes Petri dish containing moist gauze Microscope Gauze Sterile pipettes Microscope slides with etched circles Sterile, disposable cuvettes Shandon Cytospin Cytocentrifuge Test tubes Version 1.0 Page 4 of 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL 2. Reagents: a. Quality Control Material - Level I and II b. Methylene Blue - Maintained in flammable cabinet in Hematology. Store at room temp. c. Diff Quick Stain d. Saline V. QUALITY CONTROL: 1. Two levels of quality control will be tested at least once each day that a CSF Cell Count is performed. 2. Both levels of QC will be performed on the first shift during which patient testing is ordered. If day shift performed a cell count, the next shift to perform patient testing must repeat and record results for quality control level II. 3. The quality controls come ready to use. No further preparation is necessary. 4. When a new vial of control is opened, label with the date and initials of tech placing reagent in use. 5. Store the controls tightly capped at 2-8°C when not in use. Stored at this temperature, the controls are stable until expiration date. After opening, the controls are stable for six months when refrigerated. 6. Discard the controls if there is any evidence of microbial contamination. The level 2 control may appear slightly turbid after mixing. 7. Procedure for cell count controls: a. Remove CSF Controls from the refrigerator, and allow the controls to remain at room temperature for 15 minutes before mixing. b. Mix the controls thoroughly by inverting the vials several times and by squeezing the bulb in the cap at least 10 times but AVOID FOAMING to minimize cell lysis. c. Using the glass dropper provided, charge both sides of the hemocytometer chamber. Do not over or under fill. d. Immediately recap the controls and return them to the refrigerator. 533572427 Version 1.0 Page 5 of 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL e. Count all nine squares in the hemocytometer chamber. All RBC and WBC counts will be performed as stated in the procedure and calculation sections. Controls must be processed as undiluted and unstained CSF. f. Perform the controls in the same manner as patient samples. Record all results on the CSF Quality Control Worksheet (appendix 2) and in the LIS. g. The controls must be within the expected ranges posted on the Body Fluid Quality Control Worksheet. (appendix 3) h. If all results are within limits, proceed with patient testing. i. Procedure for out of range control: i. Review all reagents for expiration dates. ii. Repeat the procedure with a new vial of control(s). iii. If results are still outside of the expected ranges, notify the Hematology supervisor immediately. Corrective action must be taken before reporting patient results. iv. Out of range controls will be recorded in the Quality Control log and the hematology corrective actions log along with the corrective action taken. VI. CALIBRATION: NOT APPLICABLE VII. PROCEDURE: 1. MACROSCOPIC EXAMINATION: a. Immediately after the samples have been received, complete the CSF Worksheet with the total volume of fluid. b. Evaluate for color: Gently invert CSF tube #3 and hold both the uncentrifuged sample and the Hematology water standard against a white background. Report the color as follows: i. ii. iii. iv. Colorless - clear fluid identical to water Pink Xanthochromic - yellow color Brown c. Evaluate for clarity: Gently invert tube #3 and hold this uncentrifuged sample together with the water standard against the 12-font print standard. Report appearance as follow: 533572427 Version 1.0 Page 6 of 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL i. Clear - crystal clear fluid identical to water. ii. Hazy - turbidity present but print standard can be read easily through the tube. iii. Cloudy - print standard cannot be read through the tube. 2. MICROSCOPIC EXAMINATION: a. UNSTAINED CELL COUNT i. Prepare the hemocytometer - clean the coverslip and counting area with distilled water and follow with an alcohol wipe. Allow it to dry thoroughly. ii. Prepare the humidity chamber 1. Place 1-2 layers of gauze on the bottom of a Petri dish. It must provide a level resting area or the fluid in the hemocytometer will pool resulting in an inaccurate count. 2. Wet the gauze slightly with distilled water. 3. Place two wooden sticks or straws on top of the gauze. This will provide a resting area for the hemocytometer and keep it above the wet gauze which makes removal easier. 4. Put the hemocytometer on top of the sticks (or straws) in the Petri dish and place the clean, dry coverslip on the hemocytometer. iii. Mix the specimen and estimate (based on turbidity) if the specimen can be counted diluted or undiluted. iv. If the specimen is clear, colorless, or there is a very small volume of CSF, the specimen should not be diluted. Charge the hemocytometer and count all nine squares on both sides. 533572427 Version 1.0 Page 7 of 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL v. To charge the hemocytometer: 1. Draw up well mixed specimen using a rubber capillary tube bulb and capillary tube or a 15 µL pipette. 2. Place the end of the capillary tube against the hemocytometer and charge both sides with the fluid. Very little pressure is needed - the hemocytometer should fill by capillary action. Be careful not over or underfill and do not bump the coverslip or the count will be inaccurate. 3. Cover the petri dish with the lid and let the chamber sit undisturbed for five (5) minutes before counting. vi. If the cells are too numerous to count, the fluid must be diluted according to the number of cells present. See below for dilution steps. NOTE: The most accurate count is achieved by counting as many squares as possible (all 9 on both sides of the hemocytometer). Unmaneageable counts result in inaccurate results - do not attempt to perform an unmanageable count. If the cell count yields more than 100 cells per 9 squares (one side of the hemocytometer), perform a dilution. vii. Cells in the hemocytometer appear as follows: 1. RBC’s have a distinct outline with halos and clear centers. If crenated, they have many fine-pointed projections. 2. WBC’s are granular. 3. Tissue cells are usually large granular cells with irregular outlines. They should not be included in either the RBC or the WBC counts. 533572427 Version 1.0 Page 8 of 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL viii. Count the stained WBCs on both sides of the chamber (all eighteen squares - nine on each side). Record results on the Body Fluid Worksheet - appendix 2. ix. Count the RBC’s on both sides of the chamber (all eighteen square). Record results on the CSF Worksheet. x. Proceed with calculations. 3. STAINED CELL COUNTa. Staining is optional and may be used at the discretion of testing personnel. In this procedure, Methylene Blue is used to stain WBC’s. This helps differentiate them from RBC’s and can improve count accuracy. b. There is no dilutional effect with this procedure. c. Methylene Blue is stored in the hematology flammable chemical cabinet. Dispense a small working solution into a 1 mL specimen cup. d. Place a rubber capillary tube bulb on a clean capillary tube. Depress the bulb and hold. Place the other end of the capillary tube in the methylene blue and release the bulb drawing the stain up and fill the capillary tube at least 1/2 full. e. Depress the bulb again and dispense all of the stain onto a disposable gauze pad. Discard the gauze. The capillary tube should be coated but not filled with stain. f. With a sterile pipette, transfer a small portion of well mixed uncentrifuged CSF sample into a 1-mL specimen cup to prevent contamination in the original patient specimen tube. 533572427 Version 1.0 Page 9 of 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL g. Using the stain coated capillary tube, draw up the CSF sample to at least 3/4 full. Carefully mix the capillary tube by gently depressing and releasing the capillary tube bulb. Allow the tube to sit undisturbed for approximately two (2) minutes. h. Alternatively, use a calibrated 15 µL pipette and sterile tip. Draw methylene blue into the pipette and then discard all of the fluid. A small residue will remain in the pipette tip, which is a sufficient volume for staining. Proceed with specimen collection from the patient aliquot. i. Using a clean hemocytometer, charge both sides of the chamber with the stain coated specimen and allow the chamber to sit in a moist petri dish for five (5) minutes. j. Count the stained WBCs on both sides of the chamber (all eighteen squares). Record results on the Body Fluid Worksheet - appendix 2. k. Count the RBC’s on both sides of the chamber (all eighteen square). Record results on the Body Fluid Worksheet - appendix 2. l. Proceed with calculations. m. NOTE: If there is a 10% or greater difference between the counts from each chamber of the hemocytometer, the difference must be investigated for both unstained and stained cell counts. 4. DILUTIONS: a. Obtain 2 mL’s of 0.85% fresh uncontaminated saline from the blood bank department. b. Charge a hemocytometer with undiluted specimen and review microscopically to estimate the best dilution. Remember the ideal cell count is less than 100 cells per 9 squares (one side). c. If the specimen is excessively bloody or turbid, it may be necessary to perform counts on WBC’s and RBC’s using different dilutions. d. Dilutions must be prepared in sterile specimen tubes and labeled accordingly. The most commonly used dilutions are prepared as follows: i. 1:10 - 0.1 mL sample to 0.9 mL of Saline. ii. 1:100 - 0.1 mL of the 1:10 dilution to 0.9 mL of Saline. 533572427 Version 1.0 Page 10 of 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL NOTE: If a different dilution is needed and you are uncertain of what specimen volume to use, contact the Hematology supervisor. Use only calibrated pipettes to perform dilutions. e. Perform the cell count using either the unstained or stained procedures listed above. f. Record the dilution and all results on the CSF worksheet. 5. SMEAR PREPARATION AND DIFFERENTIAL COUNT: a. Prepare a smear by a cytocentrifuge technique for the differential count (cytospin). Refer to the Shandon or Wescor Cytocentrifuge SOP’s for step by step instruction. b. Prepare at least two (2) cytospin slides REGARDLESS OF THE WBC COUNT OBTAINED. c. A differential cell count must be performed if 1 or more WBC/mm3 are found during the cell count.. d. The Supervisor and the Pathologist must review the cytocentrifuge slide and the CSF Worksheet during the next regular duty shift. e. Enter all differential results on the Body Fluid Worksheet - appendix 2 and in the LIS. VIII. CALCULATIONS: 1. Standard formula: (Number of cells counted) x (dilution factor) (Number of squares counted) x (volume of 1 square) = cells/uL 2. QC and Undiluted Specimens: Note: The following calculations assume a counting area of 9 large squares at 0.1 μL volume per square. See the CSF worksheet and appendix 1 for a diagram of square volumes and alternate counting options. Total WBC Count (side 1 count) + (side 2 count) = Average WBC counted 2 Average WBC counted = Total WBC Count (WBC/mm3) 0.9 Total RBC Count 533572427 (side 1 count) + (side 2 count) = Average RBC counted 2 Average RBC counted = Total RBC Count (WBC/mm3) Version 1.0 Page 11 of 0.9 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL 3. Diluted Specimens: Total WBC Count (Side 1 count) + (Side 2 count) = Average WBC counted 2 (Average WBC counted) x (Dilution Factor) = Total WBC Count (WBC/mm3) 0.9 Total RBC Count (Side 1 count) + (Side 2 count) = Average RBC counted 2 (Average WBC counted) x (Dilution Factor) = Total RBC Count (RBC/mm3) 0.9 4. Calculation Examples: a. Undiluted: WBC Side 1 Count = 22 WBC Side 2 Count = 26 Example Total WBC Count 22 + 26 = 24; 2 RBC Side 1 Count = 72 RBC Side 2 Count = 78 Example Total RBC Count 24 = 27 cells/mm3 0.9 72 + 78 = 75; 2 75 = 83 cells/mm3 0.9 b. Diluted 1:10: WBC Side 1 Count = 99 WBC Side 2 Count = 93 RBC Side 1 Count = 31 RBC Side 2 Count = 39 Example Total WBC Count Example Total RBC Count 99 + 93 = 96; 96 x 10 = 1067 cells/mm3 2 0.9 533572427 Version 1.0 31 + 39 = 35; 2 35 x 10 = 389 cells/mm3 0.9 Page 12 of 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL IX. INTERPRETATIONS AND REPORTING RESULTS: 1. REPORTING RESULTS a. Record all results, color, clarity, manual cell count, and differential results on the Body Fluid Worksheet - appendix 2 during testing. Do not record any results on scrap paper. b. Any notes or comments should also be added to the worksheet. (i.e., specimen dilution, stained or unstained count, precipitate presence, etc.) c. All results, cell count data and differential, will be reported in the LIS and results released to the physician within the one hour of receipt in the laboratory. d. After the manual differential is completed a pathology review must be ordered for the specimen in the LIS. e. The results from microbiology and chemistry must also be printed from the LIS and attached to the hematology results. All section results must be available for the pathologist at the time of their review. f. Enter all pathologist comments in the LIS and reported to the physician. Upon completion, the finalized CSF worksheet will be maintained in the PATHOLOGY REVIEW book for one month. 2. INTERPRETATION OF RESULTS: a. CSF is normally clear, colorless, and hypocellular. Any turbidity or color presence is abnormal. i. To differentiate hemorrhage: a traumatic tap from subarachnoid 1. Traumatic tap - staining of the (3) tubes of CSF is uneven, being greatest in the first tube, and least in the last tube. After centrifugation, the supernatant is colorless and the specimen tends to clot. 2. Subarachnoid hemorrhage - the blood is evenly mixed, the supernatant becomes yellowish within a few hours after the hemorrhage, and the fluid will not clot. 533572427 Version 1.0 Page 13 of 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL ii. Pink color - indicates RBC lysis and hemoglobin release. It can be seen 4 to 10 hours after a subarachnoid hemorrhage. iii. Yellow or xanthochromic - indicates pathologic bleeding resulting from hemoglobin breakdown to bilirubin in the subarachnoid space. Xanthochromia persists for 2 to 3 weeks after hemorrhage. It is also caused by a very high protein concentration in the CSF or by liver disease. iv. Brown - indicates the presence of methemoglobin, which forms after a subdural or intracerebral hematoma. b. The CSF normally contains small numbers of lymphocytes and monocytes. c. Ventricular lining cells, ependymal cells or choroid plexus cells may occasionally be seen in normal or abnormal CSF. d. Additional cell types that may be found in normal CSF include bone marrow cells, chondrocytes (cartilage cells), squamous epithelial cells, fibrous tissue, and adipose tissue. e. Abnormal cells that may be seen in CSF are plasma cells, monocytes (together with neutrophils and lymphocytes), lipophages (foamy macrophages), and malignant cells. f. Others terms used to describe monocytes are "reticulomonocytes", "histiocytes", and "macrophages". 3. CORRELATION OF RESULTS a. Compare the cytospin manual differential and total cell count results. They should correlate as follows: 533572427 Hemocytometer WBC Cell Count Cytocentrifuge Expected Total Cell Recovery 0 1-15 6-10 11-20 > 20 0 - 40 20 - 100 60 - 150 150 - 250 >250 Version 1.0 Page 14 of 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL i. If they do not correlate: 1. Verify the cytospin was prepared using the same dilution as the hemocytometer cell count. 2. Verify calculations 3. Repeat the hemocytometer cell count. 4. Prepare a new cytospin specimen and repeat the manual differential cell count. b. Other section correlation - Before results are released, compare results with microbiology and chemistry. If discrepancies are detected between results, testing must be repeated if sample volume permits. c. If the problem can not be resolved, notify the attending physician and document all actions taken on the Body Fluid Worksheet appendix 2 and in the LIS. X. REFERENCE RANGES: RBC Total Cell Count All Ages: 0 mm³ WBC Total Cell Count: Adults: < 1 year old: 1-4 years old: 5-15 years old: 0-5 mm³ 1-30 mm³ 0-20/mm³ 0-10/mm³ 1. A great increase of WBCs occurs in acute pyogenic meningitis, the majority of cells being polymorphonuclear. 2. A slight to moderate increase of polys occurs in meningitis accompanying brain abscess. This also occurs in the early stages of tuberculosis, syphilitic meningitis, and poliomyelitis. After which the mononuclear cells are predominant. 3. The cell count is usually normal in multiple sclerosis, epilepsy, brain tumor, and cerebral arteriosclerosis. 533572427 Version 1.0 Page 15 of 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL Leukocyte Percent Differential: Adults: Lymphocytes…………… 60% ± 20% Monocytes……………… 30% ± 15% Neutrophils ……….…….. 2% ± 4% Neonates: Lymphocytes…………… 20% ±15% Monocytes………….……70% ± 20% Neutrophils ……………….4% ± 4% XI. PROCEDURAL NOTES: 1. Specimens must be well mixed. Failure to mix the specimen can cause erroneous results. 2. Leukocytes may begin to lyse within one (1) hour after collection. Cell counts must be performed promptly. 3. Cell counts cannot be performed on clotted CSF specimens. Notify the physician immediately. If the physician requests that the fluid be tested despite the clot, add the following comment in the LIS and on the CSF worksheet: Clotted Specimen - results are questionable. Testing performed at Dr. [Name]’s request. XII. APPENDICES: 1. Hemocytometer counting areas 2. Body Fluid Worksheet 3. Body Fluid Quality Control Worksheet XIII. REFERENCES: 1. Manufacturer’s Package Insert; Spinal Fluid Cell Controls; Quantimetrix Corporation; 2001. 2. King-Strasinger, Susan; Urinalysis and Body Fluids; Fourth Edition; F.A. Davis Book Publisher; 2001; Pages 150 to 164. 3. Kjeldsberg, Carl; Body Fluids; American Society of Clinical Pathologist Book Publisher; 1993; Pages 71 to 75 and 321 to 323. 533572427 Version 1.0 Page 16 of 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL Appendix 1 HEMOCYTOMETER COUNTING AREAS FIGURE 1 Represents one-side of a hemocytometer chamber. Tech must count both sides. W = White Blood Cell counting areas and R = Red Blood Cell counting areas. 533572427 Version 1.0 Page 17 of 18 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL SOP VALIDATION SOP NAME: CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL Clear and specific title and principle: Comments: yes / no All necessary supplies, equipment, and materials are listed: Comments: yes / no SOP is sufficiently detailed to be understood but not overly complex: Comments: SOP text adequately describes process/procedure: Comments: SOP accomplishes purpose: Comments: yes / no yes / no Reviewed by: (Name & Title) Signature: __________________ 533572427 yes / no Date: __________________ Version 1.0 Page 18 of 18