Pro6.4-E-05 Cytocentrifuge Technique for Smear Preparation SOP
advertisement

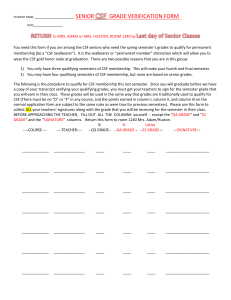
SMILE Johns Hopkins University Baltimore, MD USA CYTOCENTRIFUGE TECHNIQUE FOR SMEAR PREPARATION Author(s), Name & Title Penny S. Stevens MBS, MT (ASCP), CLS (NCA) Document Number Effective Date Sr. International QA/QC Coordinator Pro6.4-E-05 23 Jan 2009 SMILE Comments: This document is provided as an example only. It must be revised to accurately reflect your lab’s specific processes and/or specific protocol requirements. Users are directed to countercheck facts when considering their use in other applications. If you have any questions contact SMILE. Name, Title Signature Date Name, Title Signature Date Approved By SOP Annual Review Version # [0.0] Revision History Name (or location) Revision Date [dd/mm/yy] Description (notes) # of copies Name (or location) # of copies Distributed Copies to 106739189 Version 1.0 Page 1 of 12 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL I acknowledge that I have read, understand and agree to follow this SOP. Name (print) 106739189 Signature Version 1.0 Page 2 of 12 Date CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL I. PRINCIPLE: 1. The cytocentrifuge method is used as a means to concentrate cells within a defined area to enable morphological identification and differential counting. It provides more cells than that which would be present in a wedge smear preparation on the same sample and therefore, provides for greater precision in counting. 2. The principle of all cytocentrifugation techniques is that the cell is denser than the suspending fluid and under an applied force the cell will have greater momentum than the fluid. The cellular movement occurs after passing through the sample chamber. The cells are projected towards the microscope slide with sufficient momentum to cross the exit port formed by placing a filter card between the chamber sample and the glass slide resulting in cell to slide adhesion. II. DEFINITIONS 1. 2. 3. 4. 5. 6. III. CBC - Complete Blood Count CSF - Cerebrospinal Fluid LIS - Laboratory Information System QC - Quality Control RBC - Red Blood Cell WBC - White Blood Cell SPECIMENS: 1. Cerebrospinal Fluid: a. A physician obtains CSF by lumbar puncture and always under aseptic conditions. b. It is a routine practice to collect three (3) sterile tubes of CSF (1-5 ml per tube) for analysis. 2. Tubes should be collected and labeled sequentially by the physician at the time of collection. All tubes must be labeled properly and delivered immediately to the following sections: a. b. c. d. 106739189 Tube #1: To Chemistry for protein and glucose or serology study. Tube #2: To Microbiology for culture and gram stain. Tube #3: To Hematology for cell count and differential If only one tube is collected, perform testing in the following order to preserve specimen and avoid contamination: i. Microbiology - culture and gram stain. Version 1.0 Page 3 of 12 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL ii. Hematology - cell count and differential. iii. Chemistry 3. Cell lysis can begin within one (1) hour of collection so prompt delivery to the laboratory is critical. 4. Specimens must be handled as STAT. If possible, notify laboratory personnel before specimen collection to ensure staff is ready for testing immediately after collection. 5. Always deliver specimens to laboratory personnel by hand - never drop specimens off or leave unattended. 6. Clotted specimens are not satisfactory for testing. a. If the specimen is clotted, the cell count can not be performed. Notify the physician immediately. b. Prepare a Cytocentrifuge smear and review for malignant cells. Do not perform or report a manual differential. c. Document actions taken and all notification in the LIS and on the CSF worksheet. 7. Never run a body fluid through the CBC automated counting instrument. Cell counts are performed manually using a hemocytometer. 8. Hematology specimens are retained for 7 days at 2-8°C in the hematology refrigerator in the container marked "Fluids". If specimens are transferred for additional testing, they will be stored in the transfer departments as required by department procedure. IV. EQUIPMENT & REAGENTS 1. Equipment: a. Cytocentrifuge –Wescor or Thermo Shandon Cytocentrifuge b. Sterile pipettes c. Pre-cleaned etched glass cytospin slides d. Wescor Cytofunnel sample chamber e. Wescor absorbant filter pads, pre-punched f. Shandon Cytofunnel sample chamber with filter g. Shandon Cytoclip h. LIS label 2. Reagents: a. 22% Bovine Albumin Solution (protein concentration) 106739189 Version 1.0 Page 4 of 12 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL b. Diff Quick or Wright’s Stain V. QUALITY CONTROL - NOT APPLICABLE VI. CALIBRATION: Centrifuge speed verifications are performed semi-annually by the medical maintenance department. Document accordingly on the Body Fluid QC and Cytocentrifuge Maintenance Worksheet. Appendix 3 in the CSF Cell Count SOP VII. PROCEDURE: a. Determine the amount of fluid to be used depending on the appearance. Varied amounts may be used. i. Clear fluids: 2 drops of well mixed patient specimen ii. CSF fluid: Add 2 drops 22% Albumin Solution. This is a protein concentration that will aid in cell to slide adhesion and decrease cellular distortion due to the centrifugal force. iii. The cytofunnels are capable of holding 0.1mL to 0.5 mL total volume. b. Cloudy or bloody fluids: Perform a dilution using physiological saline. Albumin solution will not be required. Prepare 2 slides using the same dilution as used during the hemacytometer count and prepare an undiluted slide. Annotate the dilution factors on the slides. c. Label the slides with an LIS label or pencil. NOTE - the labels should be placed on the opposite side of the etched circle. The circle is visible through the glass and should not be on the same side as the patient specimen. d. The cytofunnels are specific to the centrifuge in use. Use only Wescor Cytopro funnels with tan or white absorption pads with the Wescor Cytocentrifuge and Thermo Shandon Cytofunnels with the Thermo Shandon Cytocentrifuge. e. The slides are also specific to the centrifuge in use. Ensure that the funnel opening aligns directly with the etched circle on the cytospin slide and use only Wescor Cytopro cytocentrifuge precleaned etched slides with the Wescor Cytocentrifuge and Shandon cytospin slides with the Thermo Shandon Cytocentrifuge. f. WESCOR CYTOCENTRIFUGE: i. 106739189 Version 1.0 Turn the instrument on. The power switch is located on the back, bottom, right of the instrument. Page 5 of 12 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL ii. Lift the lid and remove the rotor assembly. iii. Remove the sealed rotor assembly lid by pulling up on the silver button. Lift the lid off. iv. Insert the slides with the etched glass facing forward and the printing legible. v. Select the appropriate Cytopro funnel as follows: 1. Tan (slow): Clear colorless CSF or urine samples (thin samples) 2. White (fast): Synovial, sputum and turbid body fluids (thick samples) 3. Tan & White: Other fluids as necessary based on sample cellularity, turbidity and viscosity. vi. Press down on the spring arm and insert the funnel. Add patient sample as indicated previously (under section VII.a-b.) and cap the funnel. vii. Place the lid on the rotor assembly and seal it by pressing the silver button. Insert the assembly into the cytocentrifuge and close the lid. viii. Press [STOP] and select the [CYTOCENT] key. Press the number 1 for program cycle 1 and press [RUN]. All hematology body fluid samples will use cycle 1. This program is set at 1000 RPM for 4 minutes. ix. Set new programs as follows: 1. Select [CYTOCENT] and then enter the number of the program i.e., [1], [2], [3], etc. to be programmed. 2. Select [PROG] and then enter the desired speed, time and acceleration. The acceleration options are 1 = Low, 2 = Medium or 3 = High. x. The display will revert back to the cytocentrifuge main menu automatically once the acceleration has been entered g. THERMO SHANDON CYTOCENTRIFUGE: i. 106739189 Version 1.0 Place the labeled glass slide in the cytospin clip. Place a disposable Shandon cytofunnel sample chamber with attached filter facing the labeled slide. Page 6 of 12 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL ii. Close the cytospin clip. iii. Add patient sample as indicated previously (under section VII.a-b.) and cap the funnel. iv. Press the ON/OFF switch on the front of the instrument to turn power on. v. Make sure that the bench or support surface is solid immovable and flat. vi. If the ‘BAL’ and ‘!’ alarm lights flash lift the front of the instrument about ½ inch from the bench. Place the centrifuge back to normal positions. This will reset the movement detection system. vii. Press [OPEN LID] and at the same time lift the see through safety cover. viii. If it won’t open, the emergency release is located on the upper left side of the upper housing. Remove the cap and insert a pencil into the aperature. 1. Remove the Sealed Head assembly and pull up the center button of the lid until it clicks, and lift off the lid. 2. If the lid sticks, lift the centrifuge and touch the ball bearings located under the assembly. This releases the vacuum. 3. Place the cytoclip with labeled slide into the sealed head assembly. Make sure to balance the cytoclip in the centrifuge. 4. Close the sealed head by pushing the center button to secure. Carefully place assembly into centrifuge and close lid. 5. The [LID LOCK] alarm light will indicate that the safety cover is not closed correctly. Press [OPEN LID] and carefully close again. 6. Select the desired program by pressing [LOAD]. a. 1-BODY FLUIDS, 1000 rpm, 10 min. b. 2-CSF, 800 rpm, 6 min. 5-Platelet Smear 2000 rpm, 10 min. c. Press [ENTER] and [START]. 106739189 Version 1.0 Page 7 of 12 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL 7. In order to create a loaded program, select [LOAD], choose a number 1-9 using the numeric keys, press [ENTER]. a. Select [SET TIME], choose a time from 1 to 99 minutes, press [ENTER]. b. Select [SET SPEED], choose a speed between 200 and 2000, press [ENTER]. c. Select [SAVE], choose the number that was just loaded, press [ENTER]. The information will be retained in memory for future use. 8. Press the [OPEN LID] key and remove the sealed head assembly. Open the sealed head assembly by pulling the center button. Remove cytospin clips and funnels. 9. To unload the cytofunnel from the cytoclip: Hold the clip firmly. Push the spring against the slide to release it from the hooks. Allow the cytofunnel to pop out of the clip. h. Dispose of all used cytofunnels. Do not reuse. i. VIII. Dry slides horizontally before staining with wrights or Diff Quick stain CALCULATIONS: a. Differential results are reported as percentages not total number of cells counted. If cell count is performed using anything other than 100 cells, convert the cells to percentage as follows: i. [(number of cell type counted)/(total number of cells counted)] x 100 ii. If 50 total cells are counted: 15 Lymphocytes and 35 Neutrophils: 1. 15 lymphocytes/50 total cells x 100 = 30% lymphocytes 2. 35 Neutrophils/50 total cells x 100 = 70% neutrophils 3. Your calculations must total 100% when added. b. Insert the following comment: “X number of total cells counted during differential cell count and converted to percentage.” IX. REPORTING RESULTS a. Refer to the CSF Cell Count Procedure for additional information. b. Record all results, color, clarity, manual cell count, and differential results on the Body Fluid Worksheet (appendix 2 of the CSF Cell Count SOP) during testing. Do not record any results on scrap paper. 106739189 Version 1.0 Page 8 of 12 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL c. Any notes or comments should also be added to the worksheet. (i.e., specimen dilution, stained or unstained count, precipitate presence, etc.) d. All results, cell count data and differential, will be reported in the LIS and results released to the physician within the one hour of receipt in the laboratory. e. After the manual differential is completed a pathology review must be ordered for the specimen in the LIS. f. The results from microbiology and chemistry must also be printed from the LIS and attached to the hematology results. All section results must be available for the pathologist at the time of their review. g. Enter all pathologist comments in the LIS and reported to the physician. Upon completion, the finalized CSF worksheet will be maintained in the PATHOLOGY REVIEW book for one month. 2. INTERPRETATION OF RESULTS: a. CSF is normally clear, colorless, and hypocellular. Any turbidity or color presence is abnormal. i. To differentiate hemorrhage: a traumatic tap from subarachnoid 1. Traumatic tap - staining of the (3) tubes of CSF is uneven, being greatest in the first tube, and least in the last tube. After centrifugation, the supernatant is colorless and the specimen tends to clot. 2. Subarachnoid hemorrhage - the blood is evenly mixed, the supernatant becomes yellowish within a few hours after the hemorrhage, and the fluid will not clot. ii. Pink color - indicates RBC lysis and hemoglobin release. It can be seen 4 to 10 hours after a subarachnoid hemorrhage. iii. Yellow or xanthochromic - indicates pathologic bleeding resulting from hemoglobin breakdown to bilirubin in the subarachnoid space. Xanthochromia persists for 2 to 3 weeks after hemorrhage. It is also caused by a very high protein concentration in the CSF or by liver disease. 106739189 Version 1.0 Page 9 of 12 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL iv. Brown - indicates the presence of methemoglobin, which forms after a subdural or intracerebral hematoma. b. The CSF normally contains small numbers of lymphocytes and monocytes. c. Ventricular lining cells, ependymal cells or choroid plexus cells may occasionally be seen in normal or abnormal CSF. d. Additional cell types that may be found in normal CSF include bone marrow cells, chondrocytes (cartilage cells), squamous epithelial cells, fibrous tissue, and adipose tissue. e. Abnormal cells that may be seen in CSF are plasma cells, monocytes (together with neutrophils and lymphocytes), lipophages (foamy macrophages), and malignant cells. f. Others terms used to describe monocytes are "reticulomonocytes", "histiocytes", and "macrophages". 3. CORRELATION OF RESULTS a. Compare the cytospin manual differential and total cell count results. They should correlate as follows: Hemocytometer WBC Cell Count Cytocentrifuge Expected Total Cell Recovery 0 1-15 6-10 11-20 > 20 0 - 40 20 - 100 60 - 150 150 - 250 >250 i. If they do not correlate: 1. Verify the cytospin was prepared using the same dilution as the hemocytometer cell count. 2. Verify calculations 3. Repeat the hemocytometer cell count. 4. Prepare a new cytospin specimen and repeat the manual differential cell count. 106739189 Version 1.0 Page 10 of 12 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL b. Other section correlation - Before results are released, compare results with microbiology and chemistry. If discrepancies are detected between results, testing must be repeated if sample volume permits. c. If the problem can not be resolved, notify the attending physician and document all actions taken on the Body Fluid Worksheet appendix 2 in the CSF Cell Count Procedure and in the LIS. X. REFERENCE RANGES: Leukocyte Percent Differential: Adults: Lymphocytes…………… 60% ± 20% Monocytes……………… 30% ± 15% Neutrophils ……….…….. 2% ± 4% Neonates: Lymphocytes…………… 20% ±15% Monocytes………….……70% ± 20% Neutrophils ……………….4% ± 4% XI. PROCEDURAL NOTES: 1. Specimens must be well mixed. Failure to mix the specimen can cause erroneous results. 2. Leukocytes may begin to lyse within one (1) hour after collection. Testing must be performed promptly. 3. Differential cell counts cannot be performed on clotted CSF specimens. Notify the physician immediately. If the physician requests that the fluid be tested despite the clot, add the following comment in the LIS and on the CSF worksheet: Clotted Specimen - results are questionable. Testing performed at Dr. [Name]’s request. 4. Variable cellular distortion may be seen with the cytocentrifuge method. a. The cells near the center of the circle are often smaller, have less cytoplasm, and denser nuclear chromatin than those in the periphery. 106739189 Version 1.0 Page 11 of 12 CEREBROSPINAL FLUID (CSF) CELL COUNT AND DIFFERENTIAL b. Considerable nuclear distortion such as clefting or lobulation may be seen c. Other artifacts frequently encountered are peripheral localization of nuclear lobes in polymorphonuclear leukocytes, peripheral cytoplasmic vacuolation, localization of cytoplasmic granules, and holes in the nuclei. d. Benign cells, such as mesothelial cells and lymphocytes, often clump together. 5. When CSF or serous fluid is received from patients with diagnosed or suspected leukemia or any other malignancy, prepare 6 extra Cytospin slides for possible histological testing. Label the slides in pencil and do not stain. XII. APPENDICES- Refer to the CSF Cell count procedure for the following appendices: 1. Body Fluid Worksheet 2. Body Fluid Quality Control Worksheet XIII. REFERENCES: 1. CSF Cell Count Procedure 2. King-Strasinger, Susan; Urinalysis and Body Fluids; Fourth Edition; F.A. Davis Book Publisher; 2001; Pages 150 to 164. 3. Kjeldsberg, Carl; Body Fluids; American Society of Clinical Pathologist Book Publisher; 1993; Pages 71 to 75 and 321 to 323. 4. Wescor Cytocentrifuge Methods Manual, M2365-4 Rev 4; Logan, UT; 2003 5. Shandon Cytospin 3, Cell Preparation System, Life Sciences International Europe, 3/1997 106739189 Version 1.0 Page 12 of 12