text for cal module on the alimentary system
advertisement

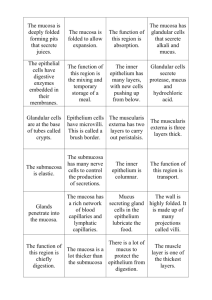
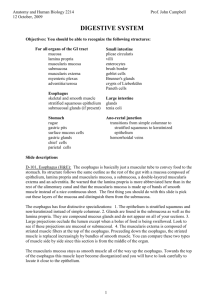
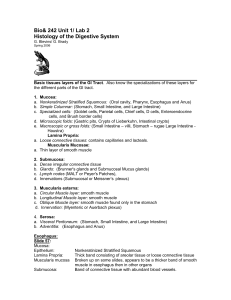
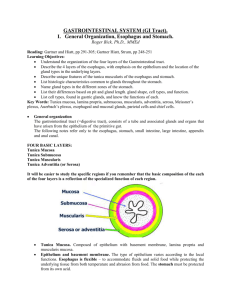
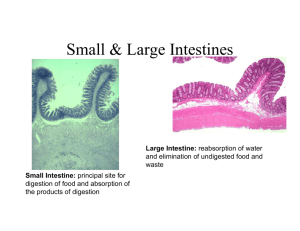
IA MVST HISTOLOGY TEXT FOR CAL MODULE ON THE ALIMENTARY SYSTEM (This program will focus on the mammalian Alimentary System) INTRODUCTION The basic structure of the gastrointestinal tract consists of four tissue layers: 1. The mucosa, comprising: i. an epithelium, which varies throughout the gastrointestinal (GI) tract to meet the function of the specific segment of the GI tract. ii. the lamina propria, a highly cellular underlying supporting tissue containing a rich vascular and lymphatic supply. Numerous cells of the immune system, particularly lymphocytes and plasma cells, are found in this layer. iii. the muscularis mucosae, a relatively thin layer of smooth muscle that provides movement to the mucosa and delimits the boundary between mucosa and submucosa. 2. The submucosa, a dense layer of supporting tissue containing large blood vessels and lymphatics. Lying in the submucosa is Meissner’s nerve plexus, composed of ganglion cells and nerve fibres. 3. The muscularis propria, consisting of two layers of muscle, an inner circular layer and an outer longitudinal layer. The coordinated rythmic contraction of these muscle layers results in peristaltic movements down the GI tract. The muscularis propria also contains a network of nerve fibres and ganglion cells both of which constitute the myenteric nerve plexus of Auerbach. 4. The adventitia, a layer of loose supporting tissue containing the larger blood vessels and nerves. Inside the abdominal cavity, the adventitia is called the serosa and is lined by simple squamous epithelium. OESOPHAGUS The general structure of the oesophagus follows that found in other parts of the GI tract. The four different layers are indicated in this LM. The mucosa is lined by stratified squamous epithelium. The muscularis mucosae is thicker than in other parts of the GI tract. The submucosa contains many blood vessels and scattered mucus-secreting glands (not shown). The latter, together with mucous glands from the mucosa, help to lubricate the epithelial surface. The muscularis propria consists of two muscle layers: outer longitudinal and inner circular layers. Skeletal muscle predominates in the upper part of the oesophagus as this is involved in swallowing, under voluntary control. In the lower regions of the oesophagus, the muscularis propria consists of smooth muscle. Stratified squamous epithelium - Oesophagus The oesophagus has a stratified squamous epithelium. Stratified epithelium consists of two or more cell layers. It is classified on the basis of the shape of the cells in the surface layers. Stratified squamous epithelium has cuboidal cells in the basal layer. As the cells move to the surface they become scale-like, squamous in shape. The main function of stratified squamous epithelium is protection. Animals with a coarse diet, may have the epithelium keratinised. Muscularis propria - Upper portion of oesophagus Since the first part of swallowing is under voluntary control, fasciculi of skeletal muscle are present in the upper portion of the oesophagus. STOMACH Histologically, the stomach is divided into three regions: the cardia, adjacent to the oesophagus; the body and fundus; and the pyloric region, leading to the duodenum. In the stomach, the food is mixed with digestive juices and churned into a soft mix called chyme. Cross-section of stomach wall – Body of stomach The mucosa of the stomach is composed of a glandular epithelium. The glands of the body and fundus of the stomach secrete pepsin, HCl and mucus. The glands of both the cardia and pyloric region secrete mostly mucus. The mucosa of the body (and fundus) of the stomach is made of narrow, straight tubular glands that open into a gastric pit and extend downwards towards the muscularis mucosa. Gastric pits are depressions of the surface of the stomach that extend for a short distance into the mucosa. The main cell types found in the gastric glands of the body and fundus of the stomach are: 1. Mucus-secreting cells. 2. Parietal cells, also called acid-secreting or oxyntic cells, and 3. Peptic cells, also called chief, zymogen or pepsin-secreting cells. Gastric mucosa – Body of stomach Upper portion of a gastric gland: The epithelium of the surface of the stomach and the gastric pits consist of a single layer of mucus-secreting columnar cells (mucus is stained magenta in this preparation). Mucus protects the mucosa from pepsin and acid damage. Parietal, or oxyntic cells are most abundant in the upper portions of the glands. Parietal cells have a large central nucleus. Their cytoplasm appears light pink in the class micrograph. Their appearance is said to resemble that of a 'fried egg'. Parietal cells secrete HCl and intrinsic factor (the latter required for the absorption of vitamin B12. Mid portion of a gastric gland: Peptic or chief cells are most numerous in the lower portions of the glands. Peptic cells have a basophilic cytoplasm, reflecting the abundance of rER and ribosomes, and basally located nuclei. Peptic cells secrete pepsinogens, the precursors of pepsins. Neck mucous cells are found scattered amongst parietal and peptic cells. Endocrine cells are also found scattered in the glands but their identification requires special tissue fixation techniques. Mid-lower portion of a gastric gland: A highly vascular, loose supporting tissue from the lamina propria supports the gastric glands and pits. ---------------------------------------------------------------------------------------------EM of a mucus-secreting cell - Stomach The cytoplasm is packed with granules containing mucin (a glycoprotein), rough ER, a prominent Golgi apparatus and some mitochondria. The nucleus is basally located. EM of both peptic cell and endocrine cell - Stomach Peptic cells secrete pepsinogens, the inactive precursors of pepsins. The cytoplasm has an extensive rough ER, a prominent Golgi apparatus and scattered mitochondria. Zymogen granules containing enzymes are distributed in the apical part of the cell. The nucleus is basally located and has a prominent nucleolus. An endocrine cell is shown at the base of the epithelium between two peptic cells. This particular endocrine cell does not reach the lumen of the gland. It contains numerous small, electron-dense secretory granules, the content of which is released into the extracellular space and may reach the capillaries by diffusion. EM of parietal or oxyntic cell - Stomach Parietal cells secrete hydrochloric acid and intrinsic factor. Parietal cells are characterised by deep branching intracellular canaliculi, extensions of the luminal surface of the plasma membrane. Numerous microvilli project from the surface of the canaliculi towards their lumen. The cytoplasm contains a large number of tubulo-vesicular structures that upon cell activation seem to fuse with the luminal plasma membrane and its extensions, increasing the surface area. It is at this membrane that HCl is produced into the canaliculi. Numerous mitochondria provide the energy required for the ion transport processes involved in hydrochloric acid production. ------------------------------------------------------------------------------Gastroduodenal junction (pyloro-duodenal junction) The transition from stomach to duodenum is marked mainly by changes in the mucosa and submucosa. The glandular arrangement of the gastric mucosa changes to a villous form in the duodenum. The villous arrangement is maintained throughout the rest of the small intestine. The submucosa of the duodenum contains mucus-secreting glands, called Brunner’s glands. These are not found in the submucosa of either the stomach or elsewhere in the small intestine. SMALL INTESTINE Chyme (a thick mix of food with digestive juices) from the stomach is emptied into the small intestine where digestion is completed and the products of digestion are absorbed. The small intestine comprises the duodenum, jejunum and ileum. These three segments share the same basic structure of the rest of the gastrointestinal tract (mucosa, submucosa, muscularis propria and serosa or adventitia) but have some distinctive features. The mucosa of the small intestine shows numerous finger-like projections called villi. Between the bases of the villi there are small pits, known as the crypts of Lieberkuhn. Both villi and crypts are covered by a simple columnar epithelium. The luminal side of the epithelial cells has numerous microvilli. Villi and microvilli greatly increase the surface area for absorption. The epithelial cells of the small intestine have a life span of 2 – 5 days and are continuously replaced by new cells resulting from mitotic divisions of stem cells from the crypts. Enteroendocrine cells are found in the small intestine, more commonly in the basal part of the crypts of Lieberkuhn. In some mammals, Paneth cells, which contain secretory granules with bactericidal properties, are also found in this location. Duodenum The mucosa of the duodenum has a characteristic villous appearance. Villi provide an increased surface area for the absorption of water, electrolytes and nutrients. Some digestion occurs on the surface itself. The submucosa contains numerous mucus-secreting Brunner’s glands. The muscularis propria consists of an inner circular layer and an outer longitudinal layer, as in the rest of the gastrointestinal tract. Duodenal mucosa – duodenal villi Intestinal villi are finger-like extensions of the surface into the lumen of the duodenum. Lying between the villi are the crypts of Lieberkuhn, which extend down to the muscularis mucosae. Both the villi and the crypts are covered by the same type of columnar cells called enterocytes. Interspersed are mucus-secreting goblet cells (stained blue in this LM). Enterocytes participate in both absorption and secretion. In the crypts, enterocytes secrete water and electrolytes. In the villi, they absorb water, electrolytes and the digestion products. Brunner’s glands - Duodenum Brunner’s glands in the submucosa are a distinctive feature of the duodenum. Brunner’s glands are acinotubular glands that secrete an alkaline mucus. This protects the duodenal mucosa by neutralising the acidic chyme received from the stomach. The excretory ducts of Brunner’s glands open into the crypts of Lieberkuhn, at the bases of the villi. Duodenal villus The villous core consists of loose connective tissue that extends from the lamina propria. It contains a rich vascular and lymphatic supply, and numerous cells, particularly cells of the immune system. Thin strands of smooth muscle extend from the muscularis mucosae. Contraction of the muscle helps to drain the lymph and provides movement to the villi so that their contact with the luminal content is enhanced. Duodenal epithelium Simple columnar epithelium with a brush border (microvilli) lines the luminal surface of the small intestine. Mucus-secreting epithelial cells, known as goblet cells (G), are found scattered amongst the columnar absorptive cells (A) of the intestinal epithelium. Lymphocytes (L) are often seen amongst the epithelial cells. Lymphocytes play a role in the immune defence system. EM of duodenal epithelium Under EM, the brush border of the intestinal epithelium appears to be made of microvilli which greatly increase the membrane area. Microvilli are found in the luminal (or apical) surface of cells specialised in absorption. Myenteric plexus of Auerbach - Muscularis propria – Small intestine Ganglion cells sre found between the two muscle layers of the muscularis propria. These ganglion cells are part of the myenteric plexus of Auerbach, which extends all the way down the intestinal wall. Note the large size of the nerve cell bodies and their prominent nuclei. The myenteric plexus controls mainly gastrointestinal movements. Submucosal or Meissner’s plexus The submucosal or Meissner's plexus is found in the submucosa of the entire length of the gastrointestinal tract and the oesophagus. Large ganglion cells are found in the submucosal plexus. The submucosal plexus controls gastrointestinal secretion and absorption, and the contractile activity of the muscularis mucosae. __________________________________________________________________________ ILEUM The ileum has the same basic structure as the jejunum and the duodenum. However, only the duodenum contains Brunner’s glands in the submucosa. The surface of the ileum is convered by villi, finger-like projections of the mucosa. A characteristic feature of the ileum is the presence of lymphoid aggregations, called Peyer’s patches, in the lamina propria and in the submucosa. Peyer’s patches contain cells of the immune system which protect the mucosa against pathogenic organisms. LARGE INTESTINE The main functions of the colon are the absorption of water and electrolytes from the intestinal content and the secretion of mucus to facilitate the passage of fAeces. The colonic mucosa has no villi. It is composed of colonic crypts that are simple tubular glands arranged parallel to each other and which extend down to the muscularis mucosae. In the base of the crypts, new cells are formed to replace those exfoliating continuously from the surface. Absorptive cells with a brush border and goblet cells enable the colon to perform its functions. Numerous bacteria are present in the colon. These can ferment material passing into the colon, such as dietary fibre. The production of short-chain fatty acids from fibre can provide a source of energy to the body (especially significant in ruminants) and to the colonic epithelium. The colonic bacteria also metabolize sloughed epithelial cells and secretions (i.e. bile acids). Additionally, bacteria synthesize vitamin K, which is absorbed in the colon and is an important source in humans.