Digestive system lab
advertisement

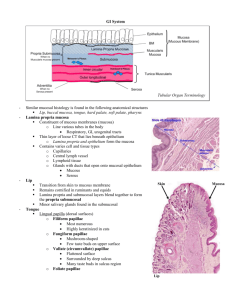
Anatomy and Human Biology 2214 12 October, 2009 Prof. John Campbell DIGESTIVE SYSTEM Objectives: You should be able to recognize the following structures: For all organs of the GI tract mucosa lamina propria muscularis mucosa submucosa muscularis externa myenteric plexus adventitia/serosa Esophagus skeletal and smooth muscle stratified squamous epithelium submucosal glands (if present) Stomach rugae gastric pits surface mucous cells gastric glands chief cells parietal cells Small intestine plicae circularis villi enterocytes brush border goblet cells Brunner's glands crypts of Lieberkühn Paneth cells Large intestine glands tenia coli Ano-rectal junction transitions from simple columnar to stratified squamous to keratinized epithelium hemorrhoidal veins Slide descriptions D-101, Esophagus (H&E): The esophagus is basically just a muscular tube to convey food to the stomach. Its structure follows the same outline as the rest of the gut with a mucosa composed of epithelium, lamina propria and muscularis mucosa, a submucosa, a double-layered muscularis externa and an adventitia. Be warned that the lamina propria is more abbreviated here than in the rest of the alimentary canal and that the muscularis mucosa is made up of bands of smooth muscle instead of a nice continuous sheet. The first thing you should do with this slide is pick out these layers of the mucosa and distinguish them from the submucosa. The esophagus has four distinctive specializations: 1. The epithelium is stratified squamous and non-keratinized instead of simple columnar. 2. Glands are found in the submucosa as well as the lamina propria. They are compound mucous glands and do not appear on all of your sections. 3. Large projections occlude the lumen except when a bolus of food is being swallowed. Look to see if these projections are mucosal or submucosal. 4. The muscularis externa is composed of striated muscle fibers at the top of the esophagus. Proceeding down the esophagus, the striated muscle is replaced increasingly by bundles of smooth muscle. You can compare these two types of muscle side by side since this section is from the middle of the organ. The muscularis mucosa stays as smooth muscle all of the way up the esophagus. Towards the top of the esophagus this muscle layer become disorganized and you will have to look carefully to locate it close to the epithelium. 1 D-103, Stomach, Fundus, monkey (H&E): Again, distinguish the main layers of the wall; mucosa, submucosa, muscularis externa and serosa. These layers in the monkey, seen here, are substantially thinner than they would be in a human. Examine the mucosa. The surface epithelium consists of mucous cap cells, a unique cell type filled with tiny secretory granules of mucus. These cells differ in appearance from typical mucous cells (e.g. goblet cells). They are narrower, their mucus-laden apical ends look clearer and their nuclei are plump and round instead of heterochromatic and pushed out of shape. Also, the mucus that they produce is biochemically distinctive in that it stays slippery at the low pH of the stomach. The gastric epithelium does not form a flat surface but, instead, dips down as a series of gastric pits. Looking down on the surface these pits would look like tiny creases, crisscrossing the surface. They are typically several millimeters long and about a millimeter deep. They increase the stomach surface area. Also, from the bottom of the pits, simple, tubular branched glands (without ducts) extend down into the lamina propria. The gastric glands run pretty much straight down except for the very distal ends, which twist around a bit. Typically, the glands are so jammed together that it is hard to recognize their orientation. Two cell types can be distinguished in the upper parts of the glands. Brightly eosinophilic parietal cells secrete HCl. Mucous neck cells are on their way to becoming mucous cap cells. The cells at the base of the glands, close to the muscularis mucosa, are chief cells. Their basal ends are strongly basophilic, indicative of large quantities of rough endoplasmic reticulum, and therefore, protein synthesis. Stem cells and hormone-secreting cells are scattered along the glands, but require special preparations for their recognition. D-104 Stomach, monkey (PAS stain): This slide shows the rugae of the stomach. These are gross wrinkles that form when the stomach is empty. They allow the stomach to extend greatly after a pig-out meal by stretching the mucosa flat. The rugae are composed of a ridge of submucosa overlain by mucosa: Thus, they are submucosal structures. Rugae are entirely different from the pits, which are mucosal and two orders of magnitude smaller. The slide has been stained with the periodic acid-Schiff reaction to demonstrate carbohydrates (a major component of mucus). It shows that mucous-secreting cells extend from the surface down into the neck of the glands. Mucous neck cells are produced by cell division in the middle of the glands and migrate up the gland to become mucous cap cells. This specialized stain is poor for examining other cellular structures. Don’t do it. D-107 Lower duodenum (H&E). This well preserved example of human lower duodenum has been sectioned longitudinally. The wall is thick, due to ridges called the plicae circulares. Under low power it becomes evident that plicae are thickenings of the submucosa covered with mucosa (epithelium, lamina propria and muscularis mucosa). They are covered on their surface by a multitude of villi. These smaller protrusions of mucosa are composed of only epithelium and lamina propria. The lamina propria is easily distinguished from the underlying submucosa. While the submucosa is rather ordinary-looking areolar tissue, the lamina propria is highly cellular with many lymphocytes. A thin layer of muscularis mucosa separates the two connective tissue layers. Examine the relatively inconspicuous glands (crypts of Lieberkühn) which invade the mucosa between the villi and extend down close to the muscularis mucosa. The Paneth cells at the bottom of the glands contain red secretory granules in their apical cytoplasm. On some slides these granules have been leached out, leaving a foamy-looking apical cytoplasm instead.) The 2 surface epithelium of the villi is tall columnar and dominated by enterocytes with a brush border. Goblet cells and lymphocytes are scattered in between. The cells in the lamina propria include lymphocytes and plasma cells, fibroblasts and smooth muscle cells. Both capillary and lymphatic channels richly supply this region, so that many of the elongate nuclei are endothelial. Turning to the submucosa, follow this layer from the core of the plicae to the tunic beneath the plicae where a rich plexus of large blood vessels and lymphatic channels are visible under low magnification. These reflect the main function of the submucosa. The muscularis externa has two muscle layers. The inner circular layer is seen in transverse section and the outer longitudinal layer is sectioned longitudinally. This smooth muscle is regulated by a well developed plexus of autonomic ganglia. Sections through this myenteric plexus can be seen as pale islands of cells, sandwiched between the two muscle layers. D-105 Pyloric-duodenal junction, human (H&E): Brunner’s glands fill up the lamina propria as well as the submucosa of the initial 10 cm or so, of the duodenum. They are long, compound, branched, and tubulo-alveolar in form; mucous in function. Ducts are sparse and those present are lined with mucous-secreting cells. Spend a moment looking at the glands and thinking about their shape. Can you find a place which shows their tubulo-alveolar morphology? The downside of this slide is that the epithelium over the sphincter has been lost. D-114, Colon. (H&E): The large intestine, the colon, conforms to the essential features of the gastrointestinal tract. the glands. Mucosal glands, still called crypts of Lieberkühn, are present although villi and pliqae are gone. In a section exactly perpendicular to the surface the glands might look like the boundaries between closely packed villi. However, if you look at an area where the knife has cut parallel to the surface you can see that the glands are small, circular tubes with narrow sheets of connective tissue between them. Goblet cells dominate the epithelium of the crypts. The connective tissue of the lamina propria is heavily infiltrated by lymphocytes and plasma cells. Lymph nodules are scattered in the submucosa. The muscularis mucosa is worth examining carefully on this slide. It has two layers, the inner circular and the outer longitudinal. This is the case throughout the GI tract but especially well demonstrated here. A principal specialization of the colon relates to its external longitudinal smooth muscle layer. This is reduced to a thin layer everywhere except for three heavy bands known as tenia coli. These are easily found without magnification as bulges in this full cross-section of the monkey colon. Between them and the inner circular layer of muscle are well developed ganglia of the myenteric plexus. D-115 Anal-rectal junction (H&E): Start at low power with the rectum. On the right hand side of your slide (which will appear on the left through the microscope). Identify the simple columnar epithelium of the rectum. Notice the tubular glands (many in cross section). Find the muscularis mucosa, the submucosa with rich venous plexus (some distended into hemorrhoids), the transversely sectioned the inner circular muscle layer, and the longitudinally sectioned fibers of the outer longitudinal muscle layer. Follow the epithelium to the right (as seen under your microscope). Look for the abrupt transition into non-keratinized stratified squamous epithelium. Farther along, the epithelium becomes keratinized to blend with the skin at the distal portion of the anal canal. Finally, note the loss of orderly layers typical of the GI tract at the anal end. 3 D-101, Esophagus (H&E) D-104 Stomach, monkey (PAS stain) D-103, Stomach, Fundus, monkey (H&E) D-107 Lower duodenum (H&E) D-105 Pyloric-duodenal junction, human (H&E) D-114, Colon. (H&E) D-115 Anal-rectal junction (H&E) 4