GASTROINTESTINAL SYSTEM 11
advertisement

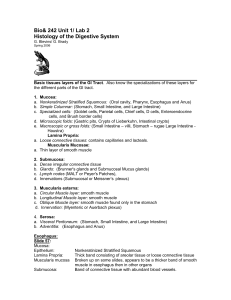
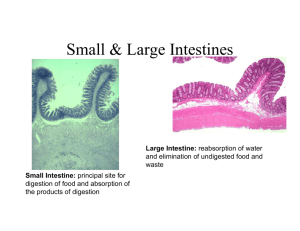
GASTROINTESTINAL SYSTEM II. Small Intestine, Large Intestine, Appendix, Anal Canal. Barry R. J. Rittman, Ph.D. Reading: Gartner and Hiatt Chapter 14, p277; BRS Cell biology and histology, Chapter 16. (Junqueira and Carneiro Chapter 15, p281) Learning Objectives: Name the cell types found in the epithelium of small and large intestines and their functions. Describe villous structure with regard to epithelium, lymphatics and blood supply. List the features and functions of Peyer's patches. List functions of the small intestinal epithelium. Correlate unique structural features throughout the small and large intestines with their functional significance for that zone. Describe how the appendix can be distinguished histologically from the colon. List unique features of the rectum and anal canal not found elsewhere in the GI tract. Key Words: Villi, microvilli, crypts, Paneth cells, absorptive cells, Payer’s patches, Brunner's glands, Auerbach's and Meissner's plexus. THE SMALL INTESTINE. GENERAL FEATURES. A tube approximately 5-7 meters long. Ridges of mucosa plus associated submucosa. Villi, are small (up to 1.5 mm long) epithelium-covered, finger like projections of the Plicae circulares (valves of Kerckring) are permanent folds created by great rolling mounds of submucosa. Plica circulares and villi significantly increase the luminal surface area. Small intestine continues digestion of chyme from stomach using enzymes associated with the glycocalyx, pancreatic enzymes and liver bile and absorbs the resulting nutrients. Lubrication and peristalsis to facilitate moving of contents. There are three portions duodenum, jejunum and ileum – all have the same basic histologic appearance (with minor differences) but some differences in function. The 4 basic layers are shown above Tunica Mucosa - General Architecture Typical GI tract pattern of epithelium, lamina propria and muscularis mucosa. Finger-like villi extend into the lumen and pocket-like crypts of Lieberkϋhn extend from the surface down into the lamina propria. Both are lined by a continuous layer of simple columnar cells. A central lacteal in the lamina propria of each villus drains into lymphatic vessels in the submucosa as seen in the diagram below. Lacteals are very important for draining chylomicrons that are absorbed by the epithelium. After a high fat meal, the splanchnic lymphatic bed will turn white due to the appearance of large amounts of these small fatty globules. A dense capillary plexus is immediately under the epithelium so that absorbed molecules have only very short distances to travel through the lamina propria to be taken up into the vasculature. Capillaries arise from one or two arterioles in the center of each villus and these in turn arise from sub mucosal arteries. Capillaries drain into one or two central venules that flow into submucosal veins. INTESTINAL MUCOSA. Epithelium-The epithelium is always simple columnar. Enterocytes (intestinal Absorptive Cells): Columnar cells plus their underlying basement membrane, form an unbroken sheet separating the lamina propria from the luminal contents. Under normal conditions tight junctions exclude bacteria and their toxins. To further increase the surface absorptive area, each enterocyte is covered with numerous microvilli. The layer of microvilli can be seen with light microscopy as a striated border (= brush border). The Glycocalyx covering the microvilli is a cell coat where enzymes for terminal digestion are located (e.g. maltase, α – dextrinase, sucrase, lactase, trehalase, aminopeptidases and enterokinases). Enterocytes a significance in the adult, in the newborn this activity is very pronounced and permits absorption of valuable antibodies obtained from mother's colostrum and milk in the first week following birth. Carbohydrates. Digested to monosaccharides and transported to portal blood. Proteins. Digested to amino acid, dipeptides and tripeptides. Some further digestion may occur in enterocytes and then amino acids transported to portal blood. Triacylglycerols. Emulsified by bile salts and digested to fatty acids and monoacylglycerols. Long chain fatty acids packaged as chylomicrons that enter lacteals and then on to lymph. Short and medium chain fatty acids enter enterocytes directly and delivered to portal blood. Water soluble vitamin B12 absorbed in ileum and requires gastric intrinsic factor. Ca2+ requires vitamin D for absorption. Fe2+ or heme Fe2+ enters the hepatocyte. Free Fe2+ released into blood. Goblet Cells Goblet-shaped mucus producing cells interspersed among the enterocytes covering the villi. The narrow base of the goblet cell contains the nucleus, while the swollen apical portion is packed full of mucus granules that are released by exocytosis. These cells provide lubrication throughout the small intestine. The further down the GI tract the greater the number of goblet cells to meet the need for increased lubrication of the luminal contents. Goblet cells appear to be clear in hematoxylin and eosin slides but in this picture the mucus is shown with the periodic acid Schiff reaction and goblet cells appear a deep red. Intestinal Glands (Crypts of Lieberkühn) • Stem Cells. Replace enterocytes and goblet cells every 3-5 days. Paneth cells Stain a characteristic orange-red with H&E stain are always located at the base of the crypts. Their color is due to the presence of numerous cytoplasmic granules filled with lysosome, an antibacterial substance. They increase in number down the small intestine, possibly to keep pace with the increasing bacterial concentration. Paneth cells secrete: Lysozyme-Bactericide. Tumor necrosis factor – α (TNF-α). Proinflammatory factor. Defensins- Increase permeability of bacteria and parasites by forming ion channels. Enteroendocrine Cells. Secrete variety of factors: Cholecystokinin. Secreted in response to small peptides, amino acids and fatty acids in the gut lumen. Stimulates secretion from pancreatic acinar cells and release of bile from gall bladder. Secretin (from S cells). In response to H+ and fatty acids in gut lumen. Stimulates release of HCO3 from pancreas and biliary tract of liver. Gastric Inhibitory peptide (from K cells). Released in response to glucose, amino acids and fatty acids in the gut lumen. Stimulates insulin secretion from pancreatic islets. Glucagon like peptide (L cells). Released in response to glucose, amino acids and fatty acids in the gut lumen. Stimulates insulin secretion and inhibits glucagon secretion. Lamina propria and Gut Associated Lymphoid Tissue (GALT). Large amounts of foreign, toxic and antigenic material close to the lamina propria are separated only be a layer of fairly porous cells and a very thin basement membrane. The intestines are considered to be in a controlled state of inflammation at all times with the mucosa constantly attacking intruders. Large numbers of cells of the immune system are found here, this an atypical characteristic of most lamina propria in other sites. The lamina propria is highly cellular loose connective tissue, containing cells derived both from mesenchymal cells as well as migrating cells of the immune system. Lymphocytes are critical for immunologic defense. They will be found not only in the lamina propria, but also migrating through the epithelium where they are known as infra-epithelial lymphocytes. Lymphocytes will also be seen in solitary lymph nodules of the lamina propria. While isolated lymph follicles are randomly distributed throughout the alimentary canal mucosa the ileum always contains a specialized collection of lymph nodules known as Peyer's patches. These are aggregates of 5-300 nodules arranged in an oval shape and unlike lymph nodes are not encapsulated. Up to 300 Peyer's patches can be found in the ileum at puberty, declining to as few as 30 in the elderly. Like other lymphatic follicles, they may have germinal centers and mantles comprised primarily of B lymphocytes, with a peripheral, ill-defined T cell zone. Plasma cells are important for production of secretory immunoglobulin A (slgA), an antibody that links with the enterocytes and is transported to the apex of the cell for release where it prevents attachment of bacteria. slgA is an extremely important mucosal surface defense weapon. The epithelium covering the dome of each follicle consists of enterocytes and specialized cells known as M cells (membranous epithelial cells). M cells are antigen presenting cells that appear to be capable of selectively taking up only certain groups of macromolecules, antigens and specific groups of bacteria, which can then be presented to the underlying lymphocytes. The Peyer’s patches in the ileum makes it a powerful immunologic organ for sampling and detecting foreign material in the environment and alerting the immune system. On the negative side, M cells may also be ports of entry for select pathogens. Special Features of specific regions of the Small Intestine. The mucosal features described above may be found the length of the small intestine but there are a few features that are limited in their distribution within this part of the alimentary tract. Brünner’s Glands (BG) Found only in the initial part of the duodenum adjacent to the stomach and merge into the mucosal pyloric glands of that organ. They are localized by definition in the submucosa, but are often extend into the lamina propria. Brünner’s glands secrete alkaline mucus to help neutralize the acidic contents of the stomach via ducts that empty into the bases of the crypts. JEJUNUM ILEUM with Peyer’s Patch Summary: Please refer to the images above. Proximal-distal modifications in function occur in the small intestine, which are reflected in its structure. Proximally, where the bolus of food digestion and absorption takes place, the wall is thicker due to a thicker mucosa and taller villi with a large absorptive capacity. Moving distally where absorption slows down, mucosal mass and villous height decreases. There is an initial capacity to neutralize stomach acid due to the secretion of Brünner’s glands in the duodenum. As intestinal contents continue to move and becoming more concentrated, goblet cell numbers increase for lubrication purposes. At the distal end of the small intestine where food absorption is less critical, immunologic surveillance is facilitated by the presence of Peyer's patches. Hepato-pancreatic secretions are dumped into the most proximal part of the intestine at the papilla of Vater to aid in digestion. After journeying through the intestine, bile salts and complexes of intrinsic factor/vitamin B12 are unique in that they can only be absorbed at the ileum to enter the splanchnic circulation. Upon passing throughout the liver, the blood is cleared of the bile salts, which then return via bile to the duodenum. This is known as the enterohepatic circulation. Histologic Identifiers:- Dodenum - villi plus Brünner’s glands; Ileum – villi plus Peyer’s patches; Jejunum - villi but absence of both Brünner’s glands and Peyer’s patches. THE LARGE INTESTINE (COLON). GENERAL FEATURES. A large diameter tube and absorbs about four fifths of the water, Na+ and Cl- from the fluid presented to it from the ileum, concentrating and solidifying it. Consists of: Mucosa with glands, no villi. Submucosa (includes Meissner’s plexus) Muscularis externa. Smooth muscle arranged as inner circular layer and three outer longitudinal layers known as taenia coli. Contraction of taenia coli muscle forms sacculations known as haustra. Auerbach’s plexus between the two muscle layers. Serosa. Intestinal Mucosa. Surface epithelium consists of numerous surface columnar absorptive cells and scattered goblet cells. Crypts are still present. and these are lined with many more goblet cells than absorptive cells. With appropriate stains enteroendocrine cells are detected in the crypts. Paneth cells are rarely found at the base of a crypt and are not considered a significant part of the cell population. Undifferentiated stem cells are present within the bases of the crypts and migrate upward to form the other four cell types. The epithelium functions to absorb water Na+ and Cl- from the stools and solidify them, Aldosterone increases numbers of Na+ channels. Large amounts of mucus released to lubricate the wall, and probably also to enhance the barrier function of the thin epithelium against the large numbers of bacteria here. Sedatives, anesthetics and steroids also absorbed Intestinal Glands. Surface absorptive cells. Goblet cells. Stem cells. Replace surface absorptive cells and goblet cells every 5-6 days. Enteroendocrine cells. APPENDIX. GENERAL FEATURES. Small blind ended tube with intestinal glands. Mucosa with simple columnar epithelium, absorptive cells, and short crypts filled mostly with goblet cells and occasional enteroendocrine cells. No M cells. Submucosa contains numbers of lymphatic nodules (not Peyer’s patches). Deposits of adipose tissue often found. Serosa. RECTUM. After the sigmoid colon the rectum descends for--and has a similar histology to the colon's but lacks taenia coil. The lower 1-2" pierces the pelvic floor and is characterized arising from its mucosal aspect by the appearance of longitudinal folds known as anal columns or rectal columns of Morgagni. These columns terminate a half inch or so from the anal orifice. The bases of the columns are connected by anal valves. The mucosal lining epithelium of the rectum, down to the valves, is simple columnar epithelium with the crypts occupied mostly by goblet cells, and changes to stratified squamous. ANAL CANAL. This is the terminal few centimeters of the alimentary canal. GENERAL FEATURES. This has a mucosa, submucosa, muscularis and adventitia. The anal canal is divided into upper and lower anal canals by the pectinate line. Upper anal canal. Mucosa has longitudinal folds the anal columns of Morgagni. Anal columns are connected at their bases by transverse fold of mucosa to form the anal valves. Pectinate line is at the lower extent of the columns. Behind the anal valves are the anal sinuses into which the anal glands open. Upper anal canal is lined by a simple columnar epithelium derived from endoderm. Lower anal canal. Below the anal valves, the epithelium is stratified squamous and the muscularis mucosa disappears. At the anal opening there is skin with its typical keratinizing stratified squamous epithelium complete with hairs. Submucosa The submucosa of the anal canal contains tortuous veins that may dilate to form hemorrhoids, and sebaceous glands. Sweat glands are present and include not only the type typically found on all skin surfaces. but also the specialized apocrine sweat glands also found in the axillae that become functional at puberty. Tunica Muscularis The smooth inner circular laver forms the internal anal sphincter (autonomic control). The outer longitudinal one is smooth initially then becomes skeletal after it passes over this sphincter to form the external anal sphincter (voluntary control). Anal rectal junction Note the change from a simple columnar epithelium to the right of the arrow to a stratified squamous epithelium on the left of the arrow. Clinical Considerations. Hirschsprung’s disease (megacolon). Failure of neural crest cells to migrate to parts of the digestive tract especially the distal portions. There is a loss of peristalsis and a backup of feces. Might be possible to correct this surgically depending on the extent. Polyps. Some polyps can become malignant. Familial adenomatous polyposis coli is an example where large number of polyps cover the surface of the mucosa and interfere with its normal functioning. Anal canal. Upper anal canal. Venous drainage to superior rectal vein to the portal vein Varicosities are known as internal hemorrhoids Tumors will drain to deep lymphatic nodes. Sensory innervation for stretch sensation, no pain sensation. Lower anal canal. Venous drainage to inferior rectal vein to the inferior vena cava. Varicosities known as external hemorrhoids. Tumors drain to superficial lymphatic nodes. Sensory innervation for pain, temperature and touch. ___________________________________________________________________________ DIGESTIVE SYSTEM II LABORATORY. You need to be able to: identify the four major tunics of the wall and their components, as described in lecture; Be sure to identify structures in bold as they often appear on tests. You should hold the slide against a white background and determine inner from outer surfaces because the tunica mucosa always looks like a thick dark band due to its cellularity and basophilia, while the outer layers are eosinophilic. SMALL INTESTINE. When examining sections of small intestine villi will appear as long finger like processes, circular profiles or images intermediate between these two due to different angles at which the individual villi are sectioned. Circular outlines of villi appear in the lamina propria and appear to be completely surrounded by the lamina propria. These are villi that are cut in cross section but which are still connected to the lumen of the intestine. Duodenum/Pyloric Stomach. Slide 70 - Returning to this slide where you looked at pyloric stomach, search along the mucosa until you begin to spot clear goblet cells in the epithelium. The mucus to these cells does not pick up H&E stain and will appear to be clear. Once you see these, you are looking at duodenum. Villi if present are a better indication of the area, but unfortunately these have been lost due to post-mortem and processing changes in some of your slides. The epithelium is frequently lifted off of the lamina propria, leaving an artifactual space. The most prominent feature of the duodenum at this point is the presence of mucosal Brünner's glands packing the lamina propria and submucosa so completely that it is very difficult to find the muscularis mucosa. Further distally, the villi tend to be preserved. Look at the enterocytes, interrupted by goblet cells. Look for crypts with bright eosinophilic Paneth cells at their bases. You won't be able to distinguish stem cells or enteroendocrine cells. Be sure you can distinguish circular profiles belonging to crypts versus those belonging to mucous glands. Observe the cellularity of the lamina propria and the loose relatively acellular connective tissue of the submucosa. Try to find multipolar neurons representing Meissner's plexus ganglia. The initial part of the duodenum has a serosa, although further along this mesothelial lining will be lost. The connective tissue here looks abnormal, with loose red blood cells indicating hemorrhage, and too many neutrophils indicating an abnormal inflammatory process was going on. Jejunum: Slide 5 - Although there is some artifactual separation of the various layers, the villi are present for the most part. Specifically, look for the striated border as a thin pink band along the surfaces of the epithelial cells. Understand the composition of this border. Central lacteals are almost never found in the human samples due to post-mortem collapse but may be presented as a demo using another species that's easier to preserve. Look for the rich subepithelial capillary plexus of the villi and in the centers for slips of smooth muscle running up the cores. Don't forget to look for Auerbach's and Meissner's plexuses. Ileum; Slide 6 - In addition to the usual features, you will see the lamina propria and part of the submucosa packed with nodules belonging to a Peyer's patch. Unfortunately, the epithelium is ripped off of most of the domes of the follicles and is floating in space, but if you look around you can see they are covered by a simple columnar epithelium and are devoid of villi. Do not try to identify M cells in these sections. In the submucosa there are some large, thin-walled lymphatic vessels filled with lymphocytes. There is also a well-preserved serosa. LARGE INTESTINE Colon: Slide 71 - The tunics are all well preserved here. Tunica mucosa: No villi of course. Vote that the surface cells are primarily absorptive cells, while goblet cells fill the crypts. Be certain you understand that all the circular profiles filled with goblet cells are really angled cuts through the long, tube-like crypts. Note the absence of Paneth cells in these crypts compared to the small intestine and enabling you to distinguish them even without seeing villi in the field. This is an excellent place to see a "textbook" example of loose cellular connective tissue to the lamina propria. There are lots of plasma cells here too. Tunica submucosa: Here's a great example of loose relatively acellular connective tissue. There are also a few lymph nodules in this laver. Look for Meissner's plexus and ganglion cells. Tunica muscularis: Observe the thickening of the outer longitudinal layer as one of the taenia coil and how thin the laver is elsewhere instead of being uniform in thickness. Tunica adventitia is found on the outside. Appendix- Slide 61 - In some of your slides the staining of the sections has faded. Please check with your neighbors to see if they have well stained sections. You may have a longitudinal as well as a cross section on this slide - the latter is easier to use. The lumen of the appendix always looks angular and sort of folded. Special features are: Mitotic figures in the crypts as elsewhere to the intestines, verifies for you that they are always the site of epithelial cell renewal. The density of the lymphatic nodules throughout the lamina propria and into the mucosa obscures the muscularis mucosa - it is not detectable here. Look for adipose tissue in the submucosa - a characteristic of this organ. Absence of taenia coli.