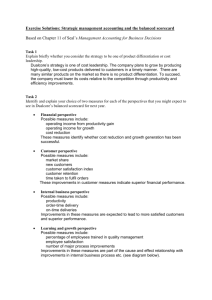
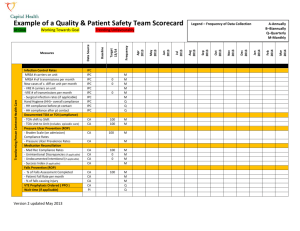
Q&PS Team Scorecard Template for Ambulatory Care
advertisement

Chart Audit 100% M Do not use abbreviation % of most recent physician order/ progress not without “Do Not Use” abbreviation used Chart Audit 100% M Patient Experience Survey PI >90 % A % of patients responding positively to decision making survey questions PI 10% A Transforming Person Centered Health Care Citizen Engagement & Accountability Performance Excellence/CDHA M M Pg. O Mar 2014 % of two client identifiers checked before intervention or service provided - Patient Fall Rate per month Two client identifier Feb 2014 M Jan 2014 100% Dec 2013 Chart Audit PSRS Nov 2013 M Oct 2013 100% Sep 2013 Chart Audit Aug 2013 M Chart Audit Jul 2013 100% 100% 100% ICP HH audit Jun 2013 Frequency Q Q Q Infection Control Rates (if applicable) Hand Hygiene overall compliance HH compliance before patient contact HH compliance after patient contact Documented Transfer of Information (compliance to standard process for area)) Episodic Care To community based care End of Service Medication Reconciliation - Med Rec Compliance Rates (if applicable) Falls Prevention (ROP) - % of Falls Observation Completed May 2013 Target 13/14 80% 75% 80% Measures A-Annually B–Biannually Q–Quarterly M-Monthly Trending Unfavourably Apr 2013 Working Towards Goal ELOS (days) At Goal Legend – Frequency of Data Collection Quality & Patient Safety Team Scorecard Data Source Example of a Sustainability Innovating Health & Learning Transformational Leadership Patient/Family/Client Complaints/Compliments (date reviewed by team) Patient, Family or Client Engagement PSRS Absenteeism (illness) FTEs HSM % of employees and physicians responding positively to leadership survey questions % of staff, management and physician responding positively to accountability survey questions % of staff completing front line leadership program # Inter-professional learning opportunities % staff completed required annual competencies % staff completed required annual patient safety education % staff completed required hand hygiene education % staff completed required hand O&HS education No show rates Cancellations Wait list times Performance Excellence/CDHA M YES M Q PI 20% q2 years PI 10% q2 years LMS A HSM Q LMS 100 A LMS 100 A LMS 100 A LMS 100 A Q Q Q Pg. O Mar 2014 Feb 2014 Jan 2014 Dec 2013 Nov 2013 Oct 2013 Sep 2013 Aug 2013 Jul 2013 Jun 2013 May 2013 Apr 2013 Frequency Target 13/14 ELOS (days) Data Source Measures Guidelines for Scorecard The scorecard is to be used in conjunction with action template. The purpose of the scorecard is to: o align operational related team goals with Capital Health’s 2013 milestones and 2016 strategic goals o track trends for improvement in your care/service area o track and trend compliance to best practice, patient safety and accreditation Required Organizational Practices (ROPs) o track and trend adverse events prevalence and or incidence of ie falls, pressure ulcers, medication reconciliations; infection control measures; etc. The scorecard is to be populated monthly, quarterly or annually depending on the indicator and availability of data. The co-leads or those delegated by the co-lead are accountable for populating the scorecard. The scorecard should be regularly discussed at the Q& PS team members. Actions need to be taken to investigated and address concerning trends in indicators. To be used as evidence for development of a quality improvement action plan and quality initiatives. Instructions for Scorecard 1. Prior to use, please review Capital Health’s 2013 milestones, 2016 Strategic goals, patient safety indicators, Accreditation ROPs and your program goals 2. Consider areas and opportunities of interest for quality improvement 3. Referring to the Data Navigation Guide for details of where and how to obtain data 4. Populate the Scorecard on a monthly, quarterly or annual basis depending of the frequency of data collection for each indicator 5. Track trends 6. Implement strategies for improvement based on evidence using the Action Template Data Source Legend IPC- Infection & Prevention Control CA- Chart Audit PI- Performance Indicators PSRS- Patient Safety Reporting system HSM- Health Services Manager LMS- Learning Management System Performance Excellence/CDHA Pg. O Performance Excellence/CDHA Pg. O