Chapter 16 Notes
advertisement

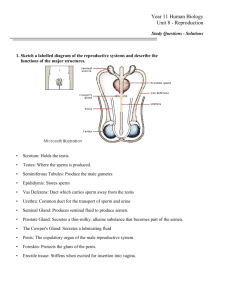
Ch 16 Reproductive System The reproductive system is a unique system-in fact that it isn’t functional until puberty. -Both male and female reproductive systems have primary sex organs or gonads -testes in males -ovaries in females -The function of the gonads is to produce gametes -sperm in males -ova or eggs in ovaries -Gonads also produce sex hormones which influence growth and development. -Accessory reproductive organs -Generally glands which nourish sperm in males or nourish a fetus in embryos Male Reproductive System The primary reproductive structures of the male- the testes-endocrine function -produce testosterone -exocrine function -sperm production -accessory gland secretion Testes -plum size -4 cm long 2.5 cm wide -covered by a connective tissue called tunica albuginea which also separates testes into lobules -each lobule contains seminiferous tubules which are sperm producing factories where spermatogenesis takes place -the interstitial cells surrounding the seminifeous tubules are the site of Testosterone production -after sperm are created, they move into the rete testes to then empty into the epididymus -the epididymus is the beginning of the duct system -epididymus-highly coiled tube (6m) on the exterior superior part of the testis -temporary storage site for immature sperm -sperm mature and gain the ability to swim while in the epididymus approximately 20 days -when sexually excited, contractions expel sperm into the ductus deferens -ductus deferens transports the sperm to the urethra for expulsion from the body -the ductus deferens runs from the testis up over the bladder and joins with the accessory glands at the prostate to form the ejaculatory duct and empties into the urethra *** -The urethra carries the sperm and accessory secretions out of the body during ejaculation -the urethra is divided into the -prostatic urethra -membranous urethra -spongy (penile) urethra Semen- Semen is actually made up of a collection of fluids which cleanse, nourish, activate and dilute the sperm. - Semen is slightly alkaline with a pH of 7.2-7.6 - It neutralizes the acidic vagina, contains an antibacterial agent and the hormone relaxin. - The amount of semen is usually 2-5 ml and contains 50150 million sperm/mL. - As sexual excitement increases, the bulbourethral gland releases its secretion which cleanses the urethra and acts as a lubricant. - As sperm leave the epididymis, they join with the secretions from the seminal vesicle (60%) at the ejaculatory duct then prostate secretions are added in as the semen is now ready for expulsion. External Genitalia - The testes are contained within the scrotum, which aids in providing proper temperature for the sperm production. o The scrotum expands and contracts to maintain a temperature 3°c lower than body temperature. - The penis is designed to deliver the sperm into the female reproductive tract. o It is divided into the shaft (made of erectile tissue) the glans penis (enlarged tip) and the prepuce also called foreskin. The foreskin is usually removed shortly after birth called circumcision. Production of Gametes - males Spermatogenesis - females Oogenesis Spermatogenesis- begins at puberty - Sperm production is initiated by a hormone called FSHfollicle stimulating hormone released from the anterior pituitary gland. - sperm are formed from stem cells called Spermatogonia within the seminiferous tubules - When spermatogonia divide they produce 2 cell types. o Daughter cell A- remains in tubule to maintain stem cell population o Daughter cell B- pushed out to lumen to become primary spermatocyte and go through meiosis. - After meiosis 4 haploid spermatids are produced. - 64-72 days later the spermatids have a tail and a helmet like acrosome which aids in egg penetration. Hormone Production and Secondary Sex Characteristics Testosterone Production- also begins at puberty - Stimulated by LH- (leutenizing hormone) from the anterior pituitary gland. - Testosterone causes the male secondary sex characteristics to emerge. o Enlarged larynx o Increase hair growth o Enlargement of skeletal muscles o Increased heaviness of skeleton Oogenesis- begins in female fetus, produces primary oocytes within the oogonia(stem cells) - Primary oocytes push into the ovary connective tissue-are surrounded by layer of cells and wait until puberty - At puberty FSH stimulates a few primary oocytes to go through meiosis to produce a secondary oocyte and a polar body. - The secondary oocyte ripens into a mature vesicular follicle stage and erupts from the ovary after about 14 days. - This is ovulation and is in response to a release of LH. - When/if a sperm penetrates the oocyte the cell will undergo a second meiotic division to produce a polar body and an ovum. - The ovum nucleus will then unite with the sperm to form a zygote. Hormone Production and Secondary Sex Characteristics - Estrogen production stimulated by the anterior pituitary gland; begins at puberty. - Estrogen also helps maintain low blood cholesterol and high calcium absorption. - Progesterone production is stimulated by the corpus luteum after ovulation each month. Secondary Sex Characteristics - estrogens not progesterone contributes to the changes that cause the secondary sex characteristics. o Enlargement of accessory organs o Breast development o Hair growth o Increased fat deposits o Widening of pelvis o Onset of mensus Female Reproductive Anatomy - Ovaries (gonads) produce haploid gametes - Within the ovaries one egg is released each month growing from a primary follicle until it ruptures from the ovary as a secondary oocyte during a process called ovulation. - The remaining ruptured follicle (scar tissue) is called the corpus luteum and it releases progesterone to help regulate the menstrual cycle. - The egg is pulled through the waving fimbrae into the uterine (fallopian) tubes. - Moving from ovary to uterus takes 3-4 days.- fertilization usually takes place in the fallopian tubes. - The uterus about the size and shape of a pear is the site where the fertilized egg is nourished and grows. - The uterus is divided into 3 regions; the top known as the fundus, the body which is the hollow chamber and the cervix the bottom most outlet to the vagina. - The uterus also has 3 layers; the inner endometrium is the site of implantation- this layer is vascular soft and shed monthly during mensus if fertilization does not occur. The myometrium is the middle muscular layer which contracts during delivery of a baby and the outermost perimetrium. - The vagina is a thin walled tube 3-4 inches long which receives the penis during intercourse. - It is also called the birth canal. - The vagina has a partially closed thin layer called the hymen which usually ruptures during the first sexual intercourse. External Structures collectively called the vulva include the following: - The mons pubis which is the fully rounded area overlying the pubic symphysis. - The large fleshy hair covered labia majora are folds on either side of the smaller hairless labia minora; these flank the vagina. - The labia majora enclose the vestibule area which contains the vagina and urethral openings. - Greater vestibule glands- flank the vagina and produce a lubricating secretion. - The clitoris hooded by a prepuce sits anterior and superior to the vestibule- it corresponds to the male penis and is composed of erectile tissue. Mensus- the menstrual cycle. -The uterus is essential for the growth of a fetus, however it is onlya short period where conditions are right for implantation. -The menstrual cycle keeps the uterus in perfect timing and conditions to receive a fertilized egg in a process called implantation. -As a cycle mensus usually takes 28 days and is influenced by different levels of hormones released at different times controlled by anterior pituitary gonadotropic hormones FSH and LH. -Menstrual phase days 1-5 The functional superficial layer of the endometrium detaches from the uterus was and is accompanied my bleeding for 3-5 days (up to 7). The average blood loss is only 50-150 mL. By day 5 growing ovarian follicles are beginning to produce more estrogen. -Proliferative phase days 6-14 Rising estrogen levels from the follicles cause the endometrial lining to regenerate and glands form within it It becomes thick and velvety Ovulation occurs within the ovary at the end of this phase in response to a sudden rise in LH -Secretory phase-days 15-28 Levels of progesterone rise (produced by the corpus luteum) adding to the increase in blood flow to the velvety endometrial lining Progesterone also causes the glands in the endometrium to secrete nutrients into the uterus which will sustain an embryo until implantation (if fertilization occurs) If fertilization does NOT occur the corpus luteum begins to degenerate as LH declines. The sudden decrease in hormones causes the endometrial lining blood vessels to spasm and kink, cutting off supplies and cells begin to die The cycle starts over again Mammary Glands function is to produce milk to nourish a newborn baby. stimulated to increase in size during puberty by hormones (estrogen) modified sweat glands, part of the skin composed of fat and lobules of alveolar glands which produce milk, milk passes out to the lactiferous ducts and exits through the protruding nipple. External structures include the pigmented areola and nipple. Fertilization- the union of egg and sperm Timing is key- the oocyte is only viable for 12-24 hours after ovulation Sperm remain viable 24-48 hours after expulsion Sperm may be deposited before ovulation 48 hours prior and up to 24 hours after ovulation for conditions to be suitable for fertilization. This is a 3-4 day window. It takes 1-2 hours for the sperm to travel up the 12 cm uterine tube to reach the ovulated oocyte. Millions of sperm reach the oocyte, enzymes break down the corona radiate surrounding the oocyte The acrosome of the sperm makes contact with the oocyte membrane receptors The sperm is pulled into the cytoplasm and the oocyte completes its second meiotic division forming an Ovum and a polar body then changes occur in the egg to keep other sperm from entering LOOK diagram fertilization.pdf Finally the genetic material of the sperm and the egg unite in fertilization to form a zygote-the first cell of a new individual Embryonic and Fetal Development Zygote undergoes cell division to become an embryo The developing embryo reaches the uterus about 3 days after ovulation and is a tiny ball of cells (about 16) Embryo floats in uterus and continues to divide into about 100 cells in a hollow sphere called a blastocyst The blastocyst secretes an LH-like hormone called human chorionic gonatoropin-stimulates the corpus luteum to produce progesterone which continues the blood supply to the endometrial lining By 7 days after ovulation the blasocyst has implanted into the endometrial lining Development is continuing and the primary germ layers (ectoderm, mesoderm, endoderm) are formed Placenta is formed By 3rd week placenta is functioning By the second month the placenta is producing all hormones to maintain pregnancy By the 8th week all organ systems have been laid down and groundwork is complete At 9th week now referred to as fetus During fetal stage grows from 3 cm to about 36 cm About 270 days after fertilization pregnancy is considered to be full term Childbirth- also called parturition expels the infant from the uterus during labor. During the last few weeks of pregnancy estrogen levels peak causing the myometrium to form oxytocin receptorsit also interferes with progesterone which acts to calm uterine muscles during pregnancy Now the uterine muscle begins to quiver these “practice” contractions are called Braxton Hicks contractions The fetus starts to release oxytocin which stimulates prostoglandins-combined these initiate more frequent and powerful contractions Now true labor begins Labor is often divided into 3 stages -Dilation Stage From initial contractions to 10 cm dialation and infants head pressing against cervix Longest stage usually 6-12 hours -Expulsion Stage Period of full dialation to delivery of the infant Accompanied by the urge to push Takes as long as 2 hours (avg 50 min 1st child) Infants usally are born head first facing down After birth the umbilical cord is clamped and cut Breech (but first) deliveries are much more difficult and the use of forceps or vacuum extractor are often necessary -Placental Stage Actually the delivery of the placenta, usually happens within 15 min of birth Often called the afterbirth Effects of pregnancy on the mother Uterus enlarges slowly to consume the majority of space within the abdominopelvic cavity Fundus reaches the xiphoid process Ribs flare to help accommodate space Center of gravity changes Accentuated lumbar curvature Nearing birth placenta releases the hormone relaxin causing pelvic ligaments and pubic symphasis to soften and increase in motility Good nutrition is important through pregnancy as building materials for tissues and organs o If this does not occur the fetus will “steal” nutrients from the mothers body to make up for the lack of building materials Pregnancy requires about 300 additional calories for fetal growth keeping nutrition in mind Morning sickness is often a symptom of nausea in response to elevated levels of progesterone o *this occurs until the woman adjusts to the increased levels-and some women never adjust Heartburn is often a symptom as the stomach and esophagus are pushed upward causing the pyloric sphincter to open more easily Constipation often occurs because of decreased motility of the digestive tract due to overcrowding Kidneys have increased duty as they cleanse the blood of the fetus too, causing more frequent urination o NOTE the blood of the fetus does not mix –see FAQ’s Nasal mucosa respond to estrogen becoming swollen and congested –this symptom usually occurs later in pregnancy and can in some cases cause noticeable physical swelling in and around the nose Blood volume rises 25-45% much of which is water Increase in blood pressure and pulse as cardiac output must increase to propel more blood Venous return is poor especially in lower limbs-sometimes resulting in varicose veins Developmental Aspects and Homeostatic Imbalances Sex of an individual IS determined at the time of conception-but gonad formation does not begin until the 8th week this is sometimes called the indifferent stage After gonads are formed it testosterone is present (produced by the fetal testes) the male duct system will result, if absent in significant quantities the female duct system will arise Puberty- usually between 10-15yrs is the time when reproductive accessory organs grow and mature o Boys- puberty begins with growth of the testes followed by increased hair growth in pubic, auxillary and facial regions then the penis enlarges for the next 2 years o Girls- puberty begins with the budding of the breasts often apparent by age 11, increased hair growth follows then about two years after puberty has begun the 1st menstrual cycle (menache) occurs. It takes about 2 more years until regular ovulation and fertility are accomplished Even though these steps remain the same sequence the age of onset varies greatly among individuals FAQ’s 1. What are hormones? a. Hormones are chemicals secreted in one tissue which travel via body fluids to other parts of the body. Its like a chemical messenger that affects growth and behavior. 2. Do women have testosterone? a. Yes. Usually small amounts, increased levels are associated with weight gain (apple shaped body), acne, menstrual irregularities, high cholesterol and more. 3. Do mother’s and baby’s blood mix? a. No. Not in normal situations. Diffusion allows for the transfer of nutrients and wastes. See link Fetal Anatomy: Understanding Placenta Anatomy | BabyZone