The Respiratory System
advertisement

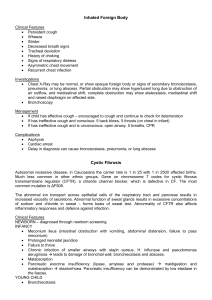
The Respiratory System Correlated to the Roy Adaptation Model and Nursing Process Sandy Marks, RN, BSN, MS(HCA) N212 Medical Surgical Nursing 1 Spring 2008 Journey through Roy Adaptation Model (RAM) Roy Adaptation Model → Patients primarily with alterations in physiological mode → oxygenation → respiratory system Course Packet (2007), p 104 Objectives - 1 Review the anatomy and physiology of the respiratory system Describe the respiratory changes associated with aging Objectives - 2 Discuss the purpose and interventions (preparation, explanation, procedure, postcare) for the following diagnostic tests: X-rays: chest, bronchogram, CT, lung scan Direct visualization: bronchoscopy Sputum specimen Thoracentesis Pulmonary function tests (PFT) Oximetry Magnetic resonance imaging (MRI) Cultures Objectives - 3 Describe the nursing assessment of the following cardinal signs and symptoms: cough sputum dyspnea Discuss the pathophysiology, nursing assessment, interventions, and evaluation for Pneumonia The Art of Caring dscherer.com Respiratory Review 1. 2. 1. 2. 3. 4. 5. Purpose = provide oxygen for tissue metabolism (O2) remove carbon dioxide (CO2) Influences functions of: acid-base balance speech sense of smell fluid balance temperature control Review the anatomy and physiology of the respiratory system trachea upper respiratory tract lower respiratory tract 1. 2. bronchi divided by trachea (windpipe) bronchioles bronchi bronchioles alveolar ducts alveoli alveoli Chabner, 2007 Gas Exchange occurs at alveolar capillary membrane occurs by diffusion Pulmonary edema = 1. 2. excess fluid fills alveoli spaces impairs exchange of O2 and CO2 capillary Chabner, 2007 Normal lung tissue 300 million alveoli surface area = tennis court Right bronchus 1. 2. slightly wider shorter more vertical increases problems with intubation aspiration Chabner, 2007 Physiologic changes associated with aging dscherer.com Alveoli alveolar surface area decreases diffusion capacity decreases elastic recoil decreases bronchioles and alveolar ducts dilate ability to cough decreases airways close early Lungs residual volume increases vital capacity decreases efficiency of oxygen and carbon dioxide exchange decreases elasticity decreases Pharynx and Larynx muscles atrophy vocal cords become slack laryngeal muscles lose elasticity and cartilage Pulmonary Vasculature increased vascular resistance to blood flow through pulmonary vascular system occurs pulmonary capillary blood volume decreases risk of hypoxia increases Exercise Tolerance and Muscle Strength Exercise Tolerance body’s response to hypoxia and hypercapnea decreases Muscle Strength respiratory muscle strength, especially the diaphragm and intercostals, decreases Susceptibility to Infection effectiveness of the cilia increases immunoglobulin A decreases alveolar macrophages are altered Chest Wall anteroposterior (AP) diameter increases thorax becomes shorter progressive kyphoscoliosis occurs chest wall compliance (elasticity) decreases mobility may decrease osteoporosis is possible Summary on effects of aging ↓ recoil and compliance AP diameter ↓ functional alveoli ↓ in Pa02 Respiratory defense mechanisms less effective Altered respiratory controls More gradual response to changes in O2 and Co2 levels in blood Diagnostic Tests X-rays: chest, bronchogram, CT, lung scan Direct visualization: bronchoscopy Sputum specimen and Cultures Thoracentesis Pulmonary function tests (PFT) Oximetry Magnetic resonance imaging (MRI) Chest X-Ray Screen, diagnose, evaluate treatment Instructions: X-ray Positions Chabner, 2007 Chest X-Ray (Cont.) Posterior Anterior View Left Lateral View Bronchogram Slightly oblique www.fotosearch.com Computed Tomography: CT Scan Images in crosssection view Uses contrast agents Right upper Lobe Instructions: Lung Scan most to detect emboli no food restrictions breathes radioactive material through a tube for 5 minutes 6 ventilation images taken radioactive injection same 6 images retaken compare images www.ucl.ac.uk Ventilation- air distribution in lung Perfusion- blood supply to & within lung www.diiradiology.com www.washingtonhospital.org Bronchoscopy Diagnose problems and assess changes in bronchi / bronchioles Performed to remove foreign body, secretions, or to obtain specimens of tissue or mucus for further study Post-Procedure Care / Instructions: Sputum Specimen To diagnose; evaluate treatment Specimen: ID organisms or abnormal cells Culture & Sensitivity (C&S) Cytology Gram stains (e.g. Acid Fast Bacilli) Thoracentesis Specimen from pleural fluid Treat pleural effusion Assess for complications Post-Procedure care: Positions •Sitting on side of bed over bedside table chest elevated •Lying on affected side •Straddling a chair Pneumothorax Chabner, 2007 Pulmonary Function Test (PFTs) Evaluate lung function Observe for increased dyspnea or bronchospasm Instructions: Pulse Oximetry Measures arterial oxygen saturation Pulse oximetry probe on ears, nose, finger, toes, forehead False readings Intermittent or continuous monitoring Ideal values When to Notify MD MRI Frontal View White masses = Hodgkin Disease lesions Chabner, 2007 MRI – transverse view – same patient Chabner, 2007 Nursing Assessment: Cardinal Signs and Symptoms of: 1. Cough 2. Sputum 3. Dyspnea Cough – Main Sign of Lung Disease how long present occurs at a specific time (smokers = upon wakening in AM) related to activity productive vs nonproductive congested dry tickling hacking Sputum – normally 3 oz produced/day important symptom associated with coughing Check: duration – long term, short term color – rust colored consistency – thick, thin, watery, frothy odor- foul amount – describe in tsp, or fractions of cup and if increasing (external or internal cause) 1. 2. 3. 4. 5. Dyspnea – subjective data (perception) 1. 2. 3. 4. difficulty in breathing or breathlessness Check: onset – slow or abrupt duration - # of hours, time of day relieving factors – position change, med, stop activity wheezing, crackles, rales, or stridor occur with breathlessness Quantify by assessing if interferes with ADL PND or orthopnea Lung sounds wheezing crackles stridor auscultation – sequence pg. 534, Iggy bronchial = trachea & mainstem bronchi bronchovesicular = branching bronchi vesicular = small bronchiole periphery Pneumonia: Case Study Nursing Student Tools Concept Map – Pneumonia Medical-Surgical Map (Medimap) Nursing Map Course Packet (2007), pgs 115-117 Pathophysiology Toxic sprinkles anyone? Etiology Cause bacteria (75%) viruses fungi Mycoplasma parasites chemicals Classifications Community-acquired pneumonia (CAP) Onset in community or during 1st 2 days of hospitalization (Strep. pneumoniae most common) Hospital-acquired Pneumonia (HAP / nosocomial) Occurring 48 hrs or longer after hospitalization Aspiration pneumonia Pneumonia caused by opportunistic organisms Pneumocystis Carinii Risk Factors CAP Older adult Chronic/coexisting condition Recent history or exposure to viral or influenza infections History of tobacco or alcohol use HAP Older adult Chronic lung disease ALOC Aspiration ET, Trach, NG / GT Immunocompromised Mechanical ventilation Clinical Manifestations - 1 Fevers, chills, anorexia Pleuritic chest pain SOB Crackles / wheezes Cough, sputum production Tachypnea Clinical Manifestations - 2 Mycoplasma (Atypical) feeling tired or weak, headaches, sore throat, or diarrhea. Eventually, most develop a dry cough. They can, also, develop fever, chills, earaches, chest pain “walking pneumonia” Diagnosis Diagnosis → Physical exam → crackles, rhonchi / wheezes CXR → area of increased density (infiltrates / consolidation) Sputum specimen – Gram stain LUL Infiltrates CXRLUL Pneumonia www.med.wayne.edu Interventions and Treatment Treatment Antibiotics → choose based on age, suspected cause & immune status Supportive care → IV fluids, supplemental oxygen therapy, respiratory monitoring, cough enhancement *may take 6-8 weeks for CXR to normalize Nursing Diagnoses… Impaired gas exchange R/T Pneumonia Pain R/T infection in lung Pneumonia Complications Hypoxemia Pleural effusion Atelectasis Pleurisy Atelectasis Pleurisy Pleural Effusion Atelectasis A = obstruction B = accumulation of fluid of air Chabner, 2007 Additional learning resources NANDA approved nursing diagnoses specific to respiratory system: p125 of study packet Skills Lab: Heart and Lung Sounds Trainer Learning Lung Sounds, Cardionics CD Audio-visual material Resources Beers, M. & Berkow, R. (Ed.). (2000). The Merck Manual of Geriatrics (3rd ed.). Whitehouse Station: Merck & Co., Inc. Chabner (2007). The Language of Medicine (8th ed.). St. Louis: Saunders. Ignatavicius, D. & Workman, L. (2006). MedicalSurgical Nursing Critical Thinking for Collaborative Care (5th ed.). St. Louis: Elsevier Saunders. Scherer, D. (2008). Pictures retrieved March 31 and available at dscherer.com dscherer.com