ECG (EKG) Lead Placement
advertisement

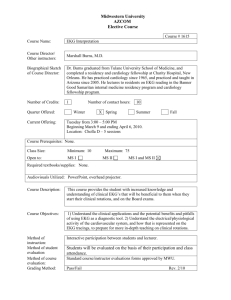
ECG (EKG) Lead Placement Debbie Kennedy, MS, RN, CHES Staff Development Coordinator, Ohio State University Wexner Medical Center, Education, Development & Resources Department In Consultation with: Mary Beth Fontana, MD, Associate Professor Emeritus, Division of Cardiovascular Diseases Department of Internal Medicine OSU ECG (EKG) Lead Placement Objectives Primary Objective: Demonstrate the ability to independently perform basic ECG (EKG) lead placement. Secondary Objective: Describe how to place ECG (EKG) leads on a patient. EKG Lead Placement: General Overview In this module you will learn and be able to: List the indications, contraindications and complications of EKG Describe how to properly apply electrodes needed to obtain a 12 lead EKG After you complete the module, you will: Demonstrate proper location and technique for EKG lead placement Demonstrate appropriate professionalism when performing EKG lead placement, which includes communicating and working with the patient while performing the procedure The term ECG is an abbreviation for Electrocardiogram. You will also see it abbreviated as EKG; the two abbreviations are interchangeable. In this module, Electrocardiogram will be referred to as EKG. I have provided you with an overview of what you will learn and be able to do as a result of completing this module. You will be prepared to perform EKG lead placement skillfully and demonstrate appropriate professionalism when performing EKG lead placement. Skillful EKG lead placement will produce an accurate EKG recording for precise interpretation of a 12 lead EKG. Introduction to EKG • Diagnostic test – Measures and records electrical activity of the heart in detail – Provides different views of electrical activity of heart • 12 views using 10 electrodes • Interpretation of EKG can aid in the diagnosis of wide range of heart conditions and guide initiation of therapy • Accuracy of EKG tracing and interpretation can be affected by – Position of patient – Skin preparation – Lead electrode placement “Because of its broad applicability, the accurate recording and precise interpretation of the EKG are critical.” JACC 2007 An EKG provides information about the electrical system of the heart from 12 different views using 10 electrodes. It is the most commonly conducted cardiovascular diagnostic procedure for a wide range of minor and life threatening heart conditions and initiation of therapy. In this module, we will focus on three aspects of the EKG that you will perform and that can affect the accuracy of the tracing and interpretation. Specifically these are: position of the patient, skin preparation, and lead electrode placement. Professionally developed and endorsed evidence-based standards for all phases of the EKG recording, along with guidelines for interpretation, have been established to ensure a high level of precision and improve the accuracy and usefulness of the EKG in practice. According to the Journal of the American College of Cardiology “Because of its broad applicability, the accurate recording and precise interpretation of the EKG are critical.” Clearly stated, if the EKG is not performed accurately, the interpretation can be adversely affected. Anatomy: Heart Conduction System Electrical activation of heart muscle cells occurs in sequence determined by heart’s conduction SA system Node Sequence of activation produces waves on EKG Electrodes and leads produce record of AV Node activity electrodes placed in standard locations using standardized reference axes activity recorded combinations of electrodes are called EKG leads First to provide a context for the EKG, we will briefly review the systems of the heart. • • • • • Heart has specialized tissue to support two systems, electrical and mechanical. The electrical conduction system coordinates the muscle cell mechanical system activity. The result is cardiac output. Heart rate is set by a small collection of specialized cells called the sinoatrial (SA) node, located in the right atrium. It is the heart’s “natural pacemaker”. SA node automatically discharges, without control from the brain; both atria contract. Electrical impulse travels through the atria to reach another area of the heart, the atrioventricular (AV) node, which serves as a relay point Impulses spread throughout specialized cells and the ventricles contract. Indications, Contraindications and Complications of EKG • Diagnosis of abnormal conduction of impulses through the heart Indications Contraindications Complications • Disturbances of normal electrical activity (arrhythmias) • Abnormalities resulting from genetic factors, chamber enlargement, chemical imbalances or blood flow problems • Preoperative assessment • Severe trauma to the chest • Uncooperative patient • None known Performing an EKG – Initial Preparation 1. 2. 3. 4. 5. 6. 7. 8. 9. Check physician order and gather machine/supplies Wash hands upon entering room and before touching patient Identify yourself to patient Identify patient by first/last name, date of birth Explain procedure Encourage patient to relax and assist Answer questions about procedure Remove clothing from waist up; provide privacy Enter patient data into machine To prepare to perform the EKG, 1) First check the physician's order and gather the EKG machine and supplies to take to the patient. 2) Wash your hands upon entering the room and before touching the patient. 3) identify yourself to the patient, giving your name and title. It is important to work with the patient in a professional manner to prepare them for the procedure, show respect and compassion and engage them in helping you with your commitment to excellence in getting the most accurate EKG reading. 4) Correctly identify the patient by asking them to give you their first and last name and date of birth. 5) Next, you will explain that you are going to perform an EKG that the doctor has ordered. Explain the procedure as simply and briefly as possible. Ask the patient if they have ever had an EKG. Describe the EKG as a test that gives a picture of how the heart is functioning. It is painless and will take about 10 minutes – more time to prepare to run the test than the actual test. When it is finished, you will give the printout to the doctor who will interpret the findings and talk with the patient. Explain how you will prepare the patient for the EKG. Let them know you will be placing “stickers” on their chest, arms and legs that will be connected to wires to the machine. Tell them you will need to clean their skin and apply some pressure with your fingers to locate where to place the leads to get an accurate recording. 6) Encourage the patient to help you get the best recording by relaxing, lying still, breathing normally and not talking when you are ready to run the report. 7) Ask the patient if they have any questions and answer as needed. 8) Explain to the patient that you will need them to remove all clothing from the waist up, give them a gown to put on, open in the front. Also, you will need their arms and legs exposed toward the wrist and ankles. Provide privacy and assistance as needed for the patient to get undressed. 9) Once the patient is ready, reenter the room. Prepare the machine by entering patient data. Positioning Patient • Place in supine position – Head flat or at no more than 45 degrees – Arms and legs free • If patient cannot lie flat or at no more than 45 degrees – Position patient for comfort and document altered position for EKG Rationale: position can alter EKG tracing To begin the procedure for obtaining EKG, you must first position the patient. Position of the patient can alter the EKG tracing. The standard position of the patient is supine – head flat or at no more than a 45 degree angle, with arms and legs free. If the patient cannot lie with their head flat or at no more than 45 degrees, position the patient for comfort. You must make a note of the altered position in your documentation so that the physician can consider the position when interpreting the EKG. Skin Preparation • It is essential to prepare the skin at the electrode sites before placing the electrodes Rationale: for best electrical conduction - de-fat and gently abrade the skin - maintain full skin contact with electrodes The next important step for preparing to place the electrodes is skin preparation. Before applying the electrodes, each area where you will place an electrode needs to be cleaned. Use an alcohol pad to de-fat the skin and a dry cloth or 2 by 2 gauze pad to gently abrade the top layer of cells of the skin. Not only does this ensure full contact of the electrode with the skin for best conduction, but also can reduce noise and improve the quality of the recorded EKG. Skin Preparation Normal Oily Diaphoretic If skin is very oily or soiled, wash with soap and water; dry Briskly rub skin with dry cloth to dry Clean skin with alcohol pad-allow to dry Briskly rub skin with alcohol pad-allow to dry Clean skin with alcohol pad-allow to dry Briskly rub skin with dry cloth or 2x2 pad Briskly rub skin with dry cloth or 2x2 pad Briskly rub skin with dry cloth or 2x2 pad This chart describes what is required for skin preparation for three common skin conditions which you will see in your patients. At each site where you will place an electrode: 1. For normal skin – clean first with an alcohol pad. Allow the alcohol to dry for the maximum benefit of de-fatting the skin. When dry, briskly rub the skin with a dry cloth or 2 by 2 gauze pad to abrade the top layer of cells. 2. For oily or soiled skin – to clean the skin, wash first with soap and water and dry. Next, briskly rub the skin with an alcohol pad. Allow the alcohol to dry. When dry, briskly rub skin with a dry cloth or 2 by 2 pad. 3. For diaphoretic skin – to dry the skin, briskly rub with a cloth or gauze pad. Next clean the skin with an alcohol pad. Allow the alcohol to dry. When dry, briskly rub skin with a dry cloth or 2 by 2 pad. A special consideration might be hairy chests; separate hairs or clip hairs. Shave only as necessary. Lead Electrode Placement • • • • • Accuracy of ECG interpretation relies on consistent lead electrode placement Four electrodes for limb leads: – right and left arms (RA LA) – right and left legs (RL LL) Six electrodes for chest leads: V1 through V6 Flat against skin Direction of lead wires: – may point in any direction • • • IMPORTANT: maintain full contact of electrode with skin with no stress/pulling on lead wires Test electrode adhesive pads to ensure sticky/moist Before performing, double check that the lead clips/wires are securely attached and going to the correct electrode The third important step is lead electrode placement. 1) Accuracy of the EKG tracing and interpretation relies on you correctly and consistently placing the electrodes. 2) You will place a total of 10 electrodes. 3) There are four electrodes for limb leads named RA right arm, LA left arm, RL right leg and LL left leg.4) There are six electrodes for chest leads named V 1 through V 6. 5) Electrodes should adhere to the skin and lay flat against skin 6) Electrodes may point in any direction as long as they maintain full contact with the skin when connected and there is no stress or pulling on the lead wires. 7) Electrodes should have adequate adhesive to be sticky and moist. 8) Before performing the EKG, double check that the leads clips/wires are securely attached and going to the correct electrode. Go to the attachments to see pictures of the clips and wires. You will notice that they are labeled and color coded. Chest Lead Electrode Placement - Landmarks • It is essential to use landmarks and palpate to find and position chest lead electrodes Rationale: - Consistent, proper lead electrode placement - Inaccurate placement of an electrode may lead to inaccurate waveforms and incorrect EKG interpretation If lead electrodes cannot be accurately placed as noted, clearly document the actual location of lead electrode placement on the EKG. First, place the chest lead electrodes. Because the accuracy of the EKG tracing and interpretation relies on consistent and proper placement, it is essential to use landmarks and palpate when positioning the electrodes. If electrodes cannot be placed in the standard position as described here, you must clearly document the actual, altered location of electrode placement Chest Lead Electrode Placement - Palpate • • • • • • V1 V2 V3 V4 V5 V6 4th intercostal space (ICS)*, right sternal border 4th ICS, left sternal border equidistant between V2 and V4 5th ICS, at the midclavicular line at the horizontal level to V4 at the anterior axillary line at the horizontal level to V4 at the midaxillary line Locate 4th ICS by finding Angle of Louis @ 2nd rib, or use 1st rib below clavicle; count down to 4th ICS The names of the six chest lead electrodes are listed here along with their proper landmarks for position. When placing the electrodes, you will palpate to find the location of the landmarks and position the electrodes. Go to the next slide to view the actual position of the electrodes on the chest. Chest Lead Electrode Placement Suprasternal Notch Clavicle Angle of Louis Horizontal Plane As you begin electrode placement on the chest it is important to locate the landmarks by palpating with the index finger. For V1, find the fourth intercostal space and the right sternal border. You can locate the 4th intercostal space in one of two ways. The first and preferred for greatest accuracy is to use the Angle of Louis. The Angle of Louis is the angle between the upper part of the sternum and the body of the sternum. You can identify it as a bony prominence. Find the suprasternal notch where the clavicle joins the sternum. Apply pressure as you run your fingers down the sternum to the bony prominence. This will be the Angle of Louis at the 2nd rib. Find the 2nd intercostal space and count down to the 4th intercostal space. The second alternative is to locate the 1st rib under the clavicle and count each rib and intercostal space to the 4th. Take caution using this alternative as there is more room for error. The 1st intercostal space may be incorrectly identified as above the 1st rib, directly under the clavicle. Next you will use the same method of palpation to position V2 using the landmark of the 4th intercostal space and left sternal border. Skip placing V3 and go next to V4. From the 4th intercostal space on the left, palpate the 5th intercostal space. Locate the middle of the left clavicle, draw an imaginary line to the 5th intercostal space and place V4 where the two intersect. Place V3 on a diagonal line between V2 and V4. Skip placing V5 and go next to V6. On a horizontal plane, or straight line, from V4, move your index finger to locate the point at the mid axilla. Place V6. Place V5 on a horizontal plane from V4 midway between V4 and V6 (most accurate way to identify) OR at the anterior axillary line. Note: According to 2007 guidelines, more research study is needed to determine the effect of breast tissue on EKG. Currently it is recommended that electrodes be placed under the breast in women, with no change in placement, until additional studies using electrodes placed on top of the breast are available. Limb Lead Electrode Placement • • Place on fleshy areas; avoid bony prominences Position in approximately same location on each limb – right arm and left arm below elbow, on lower forearm, inside of wrist – right leg and left leg; below knee on lower leg, inside of ankle If lead electrodes cannot be accurately placed in standard position, clearly document actual/alternate location of lead electrode placement Finish with limb lead electrode placement. Evidence suggests that placing electrodes on the limbs in a position other than the standard can alter the EKG. The following standards apply to limb electrode placement: 1) electrodes should be placed in fleshy areas on the inside of the arms and legs, near the wrist and ankle, avoiding bony prominences 2) electrodes should be placed equidistant from the heart and in approximately the same place on each limb. If a patient has an amputated portion of the limb, place the electrode on the fleshy area of the inside of the limb, as distal on the limb as possible. place the electrode for the opposite limb in the same altered position and record in the notes. Note standard placement of arm and leg electrodes in the picture. Final Steps Explain to Attach lead clips/wires to electrodes Turn on EKG machine the patient how important it is to lie still and be relaxed while recording Record the EKG View of person with EKG lead placement connected to EKG machine 15 Once you have accurately and correctly placed the limb and chest electrodes, you will attach the lead wires by fastening the clip of the wire to the electrode. Wires are color coded and labeled for each arm as LA, RA, for each leg as RL, LL, and for each chest lead, V1 through V6. The physician’s interpretation can be affected if the lead wires are connected to the wrong electrodes. Turn on the EKG machine. Explain to the patient you are ready to record the EKG and ask them to help by lying still and relaxing for just a moment. Record the EKG - you will get a paper printout. Normal EKG This picture represents an EKG with a stable baseline and no interference with the recording. It is a clear tracing that the physician will be able to interpret. Troubleshooting – What to Look For • Recognize a technically unsatisfactory tracing • Identify cause of problem • Correct problem – ask for assistance if necessary • Verify that problem is resolved and EKG tracing is without interference • Three main problems are: – electrical interference – wandering baseline – somatic or muscle tremor If you have not performed the EKG correctly, you will see problems with the tracing. It is important to recognize a technically unsatisfactory tracing by identifying the cause of the problem, correcting the problem and verifying that the problem is resolved and the EKG tracing is without interference before giving it to the physician. Three main problems you may see are: electrical interference, wandering baseline and somatic or muscle tremor. For each of the main problems, we will talk about how to identify the problem, the cause and what you can do to resolve the problem. Electrical Interference The first problem is electrical interference. You will see that the waveform appears as a very jagged series of lines running close together. Troubleshooting: Electrical Interference • What is the cause? – Multiple pieces of electrical equipment in use, patient using electrical appliance, improper grounding, lights • How do you troubleshoot? – – – – – – – Move electrical devices away from bed Unplug nonessential electrical devices Turn lights off Turn cell phone off Ensure cable is not lying on EKG machine or lead wires are not twisted If plug, ensure machine is plugged into 3 prong outlet Move to another room Electrical interference may have a variety of causes: multiple pieces of electrical equipment in use, patient using an electrical appliance, improper grounding of the machine (right leg is a ground wire), lights in the room To correct the problem, you could do any of the following items listed connected to electrical activity in the room. Wandering Baseline The second problem is wandering baseline. The waveform moves up and down over the course of the tracing. Troubleshooting: Wandering Baseline What is the cause? Bad lead electrode connection or exaggerated respiratory movements How do you troubleshoot? Check all leads and electrodes for correct position remove and replace misplaced leads or electrodes Check all lead electrodes for full contact with skin may have tension on wire that pulls lead electrode away remove lead electrode and replace skin may be oily or diaphoretic re-prep skin and reapply lead electrodes Have patient breath in and out and hold breath as you run EKG Wandering baseline is caused by a poor connection between the lead and the skin. To correct the problem, you could do any of the following items as listed Somatic or Muscle Tremor The third problem is somatic or muscle tremor. The waveform shows movement in the form of lines spiking and running close together. Troubleshooting: Somatic Tremor • What is the cause? – Skeletal muscle movement (eg chills, nervousness, restlessness, or disease such as Parkinson’s) • How do you troubleshoot? – Cover patient if chilled – Position patient’s hands under hips to quiet movement – Check with nurse/physician for alternate lead placement higher on the limbs if movement is not as exaggerated Causes of somatic or muscle tremor are related to skeletal muscle movement. To correct the problem, you could do any of the following items as listed to quiet the patient’s movements. Interpretation Perform according to established procedures Provide a technically correct EKG to the physician for interpretation Maximize diagnostic accuracy of the EKG The EKG is not an exact science. To maximize diagnostic accuracy, the EKG must be performed according to the established procedures and standards outlined on this module. A technically correct EKG is best for the physician and the patient. Completion • Take the clear EKG tracing to the physician • Remove electrodes and assist patient to sitting position – determine patient’s tolerance of procedure • Discard supplies • Wash hands • Document *Once you have completed the recording and before you remove the electrodes, you will take the clear tracing to the physician. The next step will be to remove the electrodes and help the patient sit up and get dressed if needed. Check with the patient to see how they are feeling. Finally, you will discard supplies. Remove the machine from the room. Wash your hands and document that you completed the procedure, any deviation in position or lead placement from the standard and how the patient tolerated the procedure. Pediatrics • Same procedures and standards would be used for children and infants. EKG Lead Placement Skill Checklist • Review the steps for EKG Lead Placement by reviewing the attachment: – Skill Performance Checklist - EKG Lead Placement • Note: critical and non critical behaviors – Critical behaviors (in bold type) are those that if performed incorrectly may directly affect the safety of the patient or the outcome of the procedure – Non critical behaviors (in non bold type) are those that if performed incorrectly may or may not affect the outcome of the procedure Go to the attachment: Skill Performance Checklist for EKG Lead Placement and review the steps for EKG lead placement.. It shows you at a glance the steps outlined in this module for EKG lead placement by defining the critical and non critical behaviors you will be expected to perform in the skills check off. Critical behaviors are those that if performed incorrectly may directly affect the safety of the patient or the outcome of the procedure. Non critical behaviors are those that if performed incorrectly may or may not affect the outcome of the procedure. Video: EKG Lead Placement Procedure Watch the video which shows the performance of the procedure – 15:20 minutes. Thank you.