Pre-Operative Medical History and Physical
advertisement
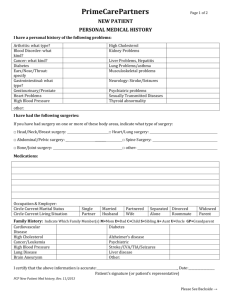
Dear Doctor: _________________________________________, is scheduled to undergo surgery on the following date : ____________________________________. Prior to surgery, our anesthesiologists’ request: This should include: H&P EKG (40 and older); chest x-ray (only if clinically indicated) LAB CBC, Platelet count, PT, PTT Urinalysis HIV, Hepatitis B & C tests. Pregnancy test (if applicable) Chem panel to include the -Routine renal and hepatic tests, including electrolytes -Calcium -Thyroid function T3 & T4 & TSH Other tests you determine to be clinically indicated. Please complete the enclosed pre-surgical evaluation form and return it with the written results of all laboratory studies. The H & P and all lab work, EKG and other results must be received by us, 14 days prior to surgery date. PLEASE DO NOT DELETE ANY OF THE ABOVE REQUESTED TESTS AND PLEASE REVIEW AND “SIGN OFF” ON ALL LABS, X-RAYS AND EKG REPORTS. You may FAX the H&P, clearance for surgery and pertinent laboratory results to (310) 278-0114. Thank you for your cooperation. Lic#G15529 Yours very truly, Robert Kotler, MD, FACS Pre-Operative Medical History and Physical Examination Patient’s Name:____________________________________________________________Date:_____________ Chief Complaint:_____________________________________________________________________________ History of Present Illness:____________________________________________________________________ Illness:______________________________________________________________________________________ Proposed Surgical Procedure(s):_____________________________________________________________ _____________________________________________________________________________________ Pertinent Medical History: Current Medications: Allergies: 1.__________________________ _____ None _____ Codeine 2.__________________________ _____ Penicillin _____ Morphine 3.__________________________ _____ Sulfa _____ Compazine 4.__________________________ _____ Tetanus _____ Iodine 5.__________________________ Medical Disorders: _____ AIDS _____ Anesthetic Reaction _____ Asthma _____ Bleeding/Clotting Disorder _____ Cancer _____ Coronary Artery Disease _____ Diabetes _____ Rheumatoid Disease OB/GYN History: LMP Social History: GR _____ Hepatitis _____ High Blood Pressure _____ Past M.I. _____ Peripheral Vascular Disease _____ Psychiatric Disorder _____ Pulmonary Disease _____ Drug Addiction _____ Other P AB Living Children Cigarettes _______________ packs per day Alcohol _______________ drinks per day/wk Drug abuse _______________ Surgical History: Type of Surgery 1.__________________________________________________________________________________ 2.__________________________________________________________________________________ 3.__________________________________________________________________________________ 4.__________________________________________________________________________________ 5.__________________________________________________________________________________ PHYSICAL EXAMINATION: AGE: SEX: HEIGHT: BP: P: R: WEIGHT: HEENT: GLANDS: NECK: CHEST: BREASTS: CARDIO: ABD: GU/RECTAL: EXTREMITIES: SKIN: CNS: IMPRESSION/DIAGNOSIS: I have reviewed all pre-operative lab, x-ray and EKG results. [circle one] YES NO Patient is medically cleared for proposed procedure(s). YES NO PHYSICIAN’S SIGNATURE: DATE: ADDRESS: PHONE NUMBER: PRINT NAME: [circle one]