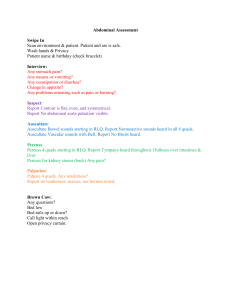
Head-to-Toe Beginner's Assessment (begin with vital signs) Neuro
advertisement

Head-to-Toe Beginner’s Assessment (begin with vital signs) Neuro Alert and Oriented times person, place, time. (A&O x 1,2,3) Responds appropriately, inappropriately? Confused? Re-orients. Pupil size and reactivity (1mm,2mm etc./brisk, sluggish, fixed/dilated) Facial Symmetry- observe, have patient smile. Does one side of mouth or face droop? Musculoskeletal Moves all extremities. MAE x4. Numbness? Pain-Pain Scale? Have pt. grip your hands and lift feet- check for weakness Wheelchair? Walker? Cane? Integument Skin warm, cool, hot? (be sure to note extremities- not just centrally) Skin dry, moist, diaphoretic (extremities as well) Skin color- pink, pale, brown, yellow, mottled Wounds? Rash? Bruising? Pulmonary Bilateral Breath sounds clear all lobes, even and unlabored? Shallow? Deep? Labored? Crackles, wheezes, rhonchi, Cheyenne-Stokes? See-saw or uneven respirations (pneumothorax) Type of oxygen delivery and amount or on room air? Chest Tubes present? Cardiac/Circulatory Peripheral pulses- radial, pedal, posterior tibial, popliteal +1,+2,+3 (weak-bounding) Capillary refill < 3 sec. Edema present 1 – 4 pitting? JVD? (Jugular venous distention) Heart Sounds – S1–S2 – try to listen for extra sounds – Listen at all 5 points Abdomen Shape of abdomen- flat, round, obese, firm, distended? Bowel sounds in all 4 quadrants (BS + x 4 quads) – active, hypoactive, hyperactive, absent? Nutrition – eating? What percentage of meals? Tube Feedings? Last bowel movement – diarrhea, constipation, blood in stool? Urinary Urinary output. Amount, color, clarity, sediments, odor Difficulty or unable to void. Signs/symptoms of infection? Reproductive In a brief assessment genitalia can be deferred unless there is a problem or your patient is OB/GYN or prostate surgery etc.. Psychosocial Laughing, smiling, talkative, crying? Family or support system? Teaching Ex. What could you teach the patient/family in order to help that patient live more independently? 07/21/10 1730 Shift assessment completed. VS: Temp 98.6 (O), AP 80 reg., RR 14, B/P 148/80. Pupils 2mm, brisk. MAE x 4 with weakness noted bilaterally in the lower extremities. Grip strength = strong . Pain 0 on 0 – 10 scale. Skin is pink, warm and dry. 3 cm. bruise noted on right thigh. Sacral area reddened. Will speak to wound RN about frequent repositioning and use of protective skin barrier cream. Breath sounds clear and un-labored, diminished in bases. S1-S2 present and regular. No murmurs noted. Radial pulses, pedal pulses, posterior tibial (RP, DP, PT) +2 bilaterally with capillary refill < 3 sec.. +1 dependent edema noted bilaterally – MD aware. (NOTE: be sure and check doctor’s notes to make sure he IS aware – even if another nurse told you he know about it!) Abdomen flat, soft BS + x 4 quads. Pt. states she is eating well “ about 90% “of regular diet. Her last BM was yesterday and she states she “didn’t quite make it to the toilet”. Urinating without difficulty although patient states “I sometimes can’t make it to the bathroom in time and wet myself”. Ambulates with walker. Smiles and laughs often. Will talk to patient about wearing “adult” briefs to help with her incontinence problem. B. Pauley RN 07/21/10 1830 Spoke with patient regarding the use of adult briefs. Pt. states she would like “to give them a try”. Also spoke with MD about potential area of skin breakdown and obtained order for consult with wound nurse. Nurse will schedule visit for tomorrow 07/22/10. B. Pauley RN