Presentation
advertisement
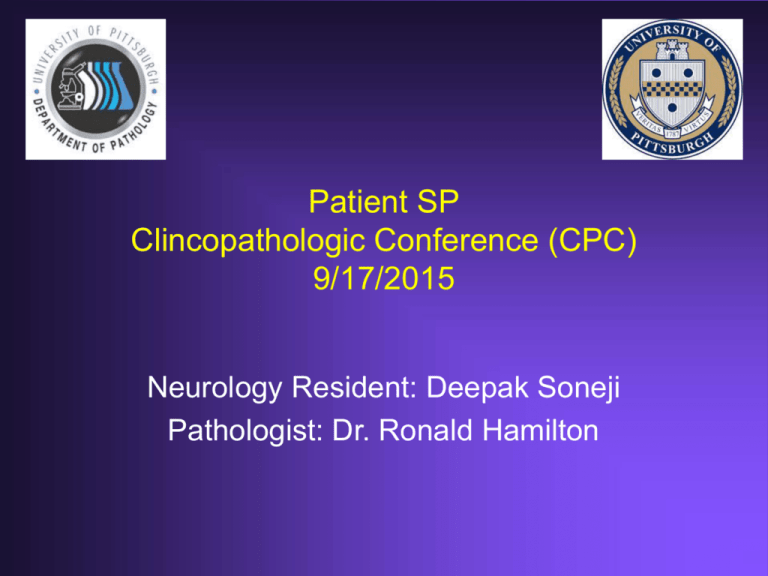
Patient SP Clincopathologic Conference (CPC) 9/17/2015 Neurology Resident: Deepak Soneji Pathologist: Dr. Ronald Hamilton CC: cognitive decline, personality changes, hallucinations HPI: 60 yo F with h/o HTN who presented to the ED per recommendation of her outpt neurologist for ~3 months of cognitive decline. Per husband, sx may have started 8 months prior to admission, with episodes of staring when asked a question or simply not responding when family tried to speak to her. Then 3 months prior to admission, pt and family took trip to rural northern PA where pt was noted to be more withdrawn, exhibited evidence of visual + auditory hallucinations, and made nonsensical statements. Sx acutely worsened in the 4 weeks prior to presentation, where pt was essentially sleeping all day. Her gait was noted to be unsteady, though pt did not have any falls. In the last 2 weeks, pt had become completely dependent on her husband to perform all her IADLs (e.g. pt didn’t know what to do when handed a utensil or a piece of toilet paper). Husband noted some urinary incontinence in the last week. Some family members noted “twitching” of L forearm which lasted ~30s-1 minute each. Further history: pt had been “stressed” in recent months due to her mother being diagnosed with Alzheimer’s approximately 1 year ago; no h/o depression, anxiety, or substance abuse. No new medications or access to other people’s meds. No recent bug bites, rashes, fevers, chills, sweats, weight loss, headaches, CP, SOB, cough, abd pain, n/v/d Remainder of ROS: per husband, negative Histories PMH/PSH: HTN Fam Hx: Mother with unknown thyroid d/o, Alzheimer’s dementia (diagnosed in her 80s) Soc Hx: used to work as telephone operator but currently unemployed, former 0.5ppd smoker for ~5 years, rare EtOH, no illicits; lives in Johnstown, PA with husband; no children Meds: HCTZ 25mg, no OTCs or herbals Allergies: None Physical Exam • • • • • • • • • • T 37.4C, BP 125/82, P 83 and regular, RR 16, O2 97% on RA GENERAL: NAD, somnolent but easily arousable, oriented to person only EYES: no scleral injection, no discharge or icterus ENT: Oral mucosa dry, pharynx without erythema or exudate NECK: Supple, non-tender, no LAD, no thyromegaly LUNGS: Lungs clear to auscultation bilaterally, no crackles or wheezes appreciated HEART: normal rate, reg rhythm, no m/g/r, no peripheral edema ABDOMEN: Non-distended, no stigmata of liver disease, +BS, no organomegaly, NT, no rebound or guarding SKIN: warm, dry, without rashes, no jaundice EXTREMITIES: Without tenderness or deformity, no effusions PSYCH: flat affect, minimally conversant, poor eye contact Physical Exam • MS: Somnolent but easily arousable, orientation as above. Language fluent but makes nonsensical statements. Attention poor. Follows commands inconsistently. Naming intact. Cannot spell "WORLD" backward or perform serial 7s, recalls 0/3 words; +glabellar, +BL grasp • CN: PERRL. EOMI without nystagmus. +blink to threat. Facial sensation intact to LT. Facial muscles full and symmetric. Hearing intact to conversation. SCMs and shoulder shrug normal. Tongue midline. • MOTOR: Normal bulk, increased tone and spasticity of UE BL. No pronator drift. Trace low amplitude rhythmic movement of L forearm (only observed this 1x during hospital course) • UE strength 5/5 deltoids, biceps, triceps, hand grip bilaterally • LE strength 5/5 iliopsoas, gluteals, hamstrings, quadriceps, tibialis anterior, gastrocnemius • REFLEXES: 3+ at biceps, triceps, brachioradialis, patella, and achilles. No clonus. Flexor plantar response bilaterally. Hoffman negative. • SENSORY: Withdraws all 4 extremities to noxious stimulation • COORDINATION: Did not participate in FTN or HTS • GAIT: limited exam, required assistance x2 to sit up from bed Differential Diagnosis • • • • • • • Infectious vs. autoimmune encephalitis CJD Sarcoid CNS lymphoma NPH Neurodegenerative d/o such as DLB CNS vasculitis Initial Labs • CBC: WBC 6.7, Hgb 12.9, Plt 138 • BMP: Na 159, K 3.6, Cl 123, CO2 25, BUN 30, Cr 0.9 • ALT 107, AST 61, AP 62, Tbili 0.7, Albumin 3.4 Imaging Imaging Diagnostic Workup • ESR 72, Anti-TPO 18 (normal<10), TSH WNL but Free T4 low (0.74) • NH3, copper, ceruloplasmin, Pb, serum ACE, ANA, RF, SSA/SSB, Lupus ab, B12, anti-thyroglobulin ab, Lyme ab, RPR, HIV ab, Hep A/B/C screen, UA, UDS, serum autoimmune encephalitis panel unremarkable • SPEP showing elevating a2 and gamma globulins but no monoclonal proteins; UPEP neg • LP: OP 14 cm H20, 15 WBCs (95% lymphs), glucose 67, protein 105 • Cytology neg • VZV, HSV, EBV PCRs neg, bacterial and fungal cx NG; West Nile ab, Crypto ag, India ink stain, AFB cx neg (OSH) • OCBs and elevated IgG index • Autoimmune encephalitis panel neg • EEG: mod generalized slowing, no focal slowing, no seizures or epileptiform discharges • CT C/A/P w/ contrast: incidental BL PEs w/o cardiac strain, 1.2cm R thyroid nodule, no lymphadenopathy, no suspicious masses • LE venous duplex: BL DVTs Hospital Course • Pt started on IVF to correct free water deficit • Empiric IV solumedrol 500mg q12 for planned 5d course • no significant improvement after 3d • Heparin gtt - > therapeutic Lovenox for PE/DVT • WBC rose to 17 on day 5, but we attributed this to steroids • CXR neg, UA pos -> started pt on cefuroxime • By day 5 of admission, transaminases continued to rise • RUQ u/s w/ dopplers -> no evidence of cirrhosis, no thrombosis • GI consulted • On the evening of day 5, pt became tachypneic and hypotensive • Condition C called; by the time CCM arrived, pt was apneic and in pulseless arrest • CPR, urgent intubation, CCM team noted ?coffee ground emesis in airway • Stat labs revealed Hgb 4.0, Plt 54, Lactate 26, ABG w/ pH of 6.95 • pt transferred to NICU where she continued to deteriorate despite multiple pressors, bicarb drip, and transfusions; family contacted and eventually made pt CMO • Autopsy report revealed massive spontaneous LLQ retroperitoneal bleed; no GI bleed; no occult malignancy Predicted Pathology Gross specimen -edema in amygdala, temporal lobes, thalami Microscopic Perivascular inflammation -lymphocitic infiltration -viral inclusions?