Pheochromocytoma - UCSF | Department of Medicine
advertisement

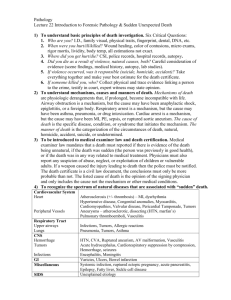
AD 8/02 Pheochromocytoma Key Points: 1) Pheochromocytomas are rare causes of hypertension. 2) Diagnosis is usually made by increased 24 hour urine catecholamine metabolites. 3) Surgery is the treatment of choice but is considered high risk due to hemodynamic instability. 4) Pre-operative treatment includes use of alpha blockers, beta blockers, and metyrasine. Epidemiology: Occurs in less than 0.2% of patients with hypertension and affects males and females equally. Age prevalence of 30-50yo. 10-15% are familial, although some estimates suggest a higher association. Rule of Tens: Ten percent of pheochromocytomas are: -bilateral -malignant -extra-adrenal -familial -in children Genetic predispositions: Von Hippel-Lindau: Autosomal dominant disease with predilection for pheochromocytomas(10-20%), retinal angiomas, cerebellar hemangioblastomas, renal/pancreatic/epididymal tumors. MEN-2: pheochomocytomas in 50%. Type “a” also has medullary thyroid carcinoma and hyperparathyroidism. Type “b” includes pheo, medullary thyroid carcinoma, and mucosal neuromas. **Routine genetic testing not recommeded in patients with pheos unless diagnosed under age 21, bilateral or extradrenal, or multiple paragangliomas. Pathopysiology: Pheochromocytomas are chromaffin cell tumor that synthesize and release catecholamines. Norepinephrine is usually the most abundant with smaller doses of epinephrine. In MEN-2, epinephrine is more common and in von Hippel Lindau norepinephrine is prevalent. Clinical Presentation: Symptoms are caused by the hypersecretion of norepinephrine and epinephrine (occasionally dopamine) and occur in 95% of patients. Few will have the classic triad of headache, palpitations, and sweating. Most will have one of these symptoms. Other symptoms include: --tremor, anxiety, panic attacks --nausea, emesis --weakness and fatigue --blurred vision, polyuria, polydipsia. Paroxysmal symptoms last minutes to hours and occur in 50%. Malignant hypertension may occur especially during stress, trauma, or physical activity. Complications: • Cardiac: CHF, MI, arrhythmias, orthostasis from volume contraction • Metabolic: Increased metabolic rate, weight loss • Endocrine: Hyperglycemia from suppression of insulin production by the excessive catecholamines Biochemical Tests: Unclear which is the best test, although most patients will have clearly abnormal values. • 24h urine metanephrines, vanillylmandelic acid (VMA), and free catecholamines: sensitivity is broad depending on the study 79-99%. Most feel this is the first best test, as the values are usually elevated. Urine metanephrines: >1.2mg/d. Can see falsely elevated levels if patient is on labetolol or buspirone (metabolite of buspirone mistakenly read as metanephrine). • Plasma catecholamines: Must be drawn under strict guidelines including patient fasting, supine for 30 minutes, and needle inserted at least 20 minutes prior to blood draw. Norepinephrine >2000pg/ml or epinephrine >200pg/ml is 95% specific and 85% sensitive. Metanephrine and normetanephrine plasma measurement are probably the most sensitive because these metabolites released directly from adrenals (>90% and 24-40%, respectively). AD 8/02 Pharmacologic tests: • Clonidine suppression test: indicated if urine and plasma studies are non-diagnostic and history is still suggestive. Clonidine will suppress the sympathetic nervous system but not the pheo production of catecholamines. If no pheo, clonidine 0.3mg should decrease norepi and epi to less than 500pg/ml by 23hours (92% accurate). False positives can occur with concomitant use of beta-blockers, TCAs, diuretics, or with renal failure. • Other test: Rarely needed but include glucagon, phentolamine, histamine, tyramine, and metaclopramide stimulation tests. Radiologic tests: • CT scan: 87% sensitive because it may miss tumors less than 1cm which means in MEN-2 can miss up to 25%. Generally though an inexpensive first test. • MRI: 98-100% sensitive, bonus ability to differentiate an adrenal pheo from other adrenal masses by T2 weighted images showing hyperintensity of pheos. • MIBG scan: meta-iodobenzylguanidine is a physiological analog of norepinephrine taken up by tissues that concentrate catecholamines. When labeled with I131 it can detect tumors missed by CT or MRI and is excellent for evaluation of metastasis. Patients should not be on phenoxybenzamine prior to scan. • PET scan: can detect tumors in unusual locations. • Adrenal Vein sampling: only needed when work up is inconclusive and should be done in experienced centers. Treatment: Surgical removal is treatment of choice but requires an experienced surgeon and anesthesiologist due to increased risk of operation. Some are now being successfully removed laparoscopically. Pre-operative treatment: Treat hypertension and volume contraction. Hypertensive treatment • Alpha blockade with phenoxybenzamine, a long acting alpha pre and post-synaptic adrenergic antagonist. 10mg BID and increase to 0.5mg/kg daily in divided doses as needed to control HTN for 2-3weeks prior to surgery. Hold the morning of surgery. Prazosin may be used but requires more frequent dosing. • Beta blockade can be added to treat tachycardia after adequate alpha blockade has been started. Labetolol best with its alpha 1 and beta-adrenergic antagonist activity. • Metyrosine (alphs-methyl-para-tyrosine) inhibits catecholamine synthesis and in one report patients receiving metyrosine had a smoother perioperative course than those receiving phenoxybenazamine alone. • Calcium channel blockers may be used if beta-blocker not tolerated. Highest risk periods are during anesthesia induction and when tumor is manipulated. Nitruprusside should be available. Post-operatively hypotension and shock may occur. Hypoglycemia may develop in 10-15% secondary to release of suppression of insulin by excess catecholamines. Catecholamine secretion should return to normal in about one week. Prognosis: Can be cured with surgery, although recurrence rate 14% in one series, with half of those being malignant. Risk of recurrence highest in familial disorders. All patients need long-term monitoring, although exact monitoring parameters have not been established. Malignant tumors have survival rate of less than 50%. Pain from metastatic bone lesions can be relieved with radiation therapy +/- chemotherapy. References: Dluhy. Pheochromocytoma—death of an axiom. NEJM Vol 346 May 2002. Eisenhofer, et al. Plasma Normetanephrines and Metanephrines for Detecting Pheochromocytomas in Von Hippel Lindau Disease and MEN Type 2. NEJM June 1999. Pheochomocytoma. Advance in Internal Medicine. 1990; 35: 195-200. Pheochromocytoma: diagnosis, localization, and management. NEJM 1984; 311(20) 1298-1303. Gotoh, et al. Laparoscopic adrenalectomy for pheochromocytoma: morbidity compared with adrenalectomy for tumors of other pathology. J Endourol, May 2002.