Adrenal Medulla
advertisement

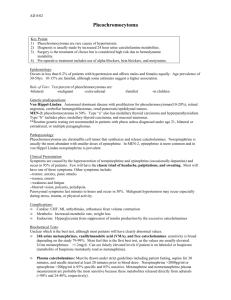
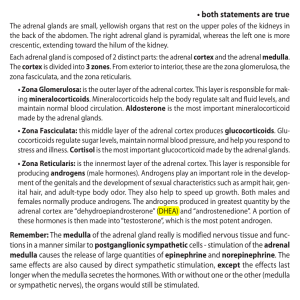
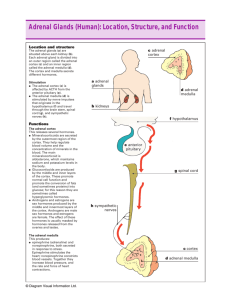
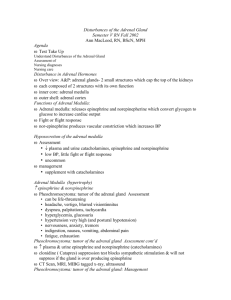
Adrenal Medulla Physiology Bob Bing-You, MD, MEd, MBA Medical Director Maine Center for Endocrinology A Case of the Sweats • 32 y.o. white male • 6 month h/o increased sweating; nonexertional, profuse • Occasional h/a’s, palpitations • Father had a “high calcium problem” and his paternal GGM had thyroid surgery for a tumor Adrenal Over-production • Adrenal Medulla – Catecholamines, norepinephrine, epinephrine • Adrenal Cortex – surgical disease – Cushing’s syndrome – Hyperaldosteronism [Conn’s Syndrome] – Androgen-producing tumors Adrenal medulla function • Stimulated by sympathetic nervous system to release epinephrine and norepinephrine • 80% epi and 20% norepi • Effects on tissues 10 x longer than direct sympathetic stimulation due to slow removal Catecholamine effects • Norepinephrine – – – – Vascular vasoconstriction Increased heart rate Inhibit GI tract Pupil dilation • Epinephrine – Greater effect on cardiac activity – Weaker vasoconstriction [less effect on BP] Other effects • Epi >> norepi increasing metabolic rate • Support vascular “tone” • Catecholamines support direct stimulation of tissues activated by sympathetic system • Back-up system for each other Tiger fight-or-flight • • • • • • • arterial pressure blood flow to all active muscles rates cellular metabolism throughout body blood glucose concentration glycolysis in muscle mental activity rate of blood coagulation Catecholamine biosynthesis • Tyrosine » dopamine » norepinenephrine » epinephrine • Degraded to vanillylmandelic acid [VMA] and metanephrines Pheochromocytoma • Rare: 1/1000 HTN patients – Resistant HTN, secondary cause considered • Triad of symptoms • Multiple Endocrine Neoplasia [MEN] Type 2A and 2 B – “PAT”: parathyroid, adrenal pheo, medullary thyroid cancer – “MAT”: mucocutaneous neuromas Case of the sweats • 32 y.o. white male • 6 month h/o increased sweating; nonexertional, profuse • Occasional h/a’s, palpitations • Father had a “high calcium problem” and his paternal GGM had thyroid surgery for a tumor What MEN syndrome does he have? • • • • A. MEN 1 B. MEN 2a C. MEN 3c D. MEN 2b Diagnosis • Plasma metanephrines • 24 hour urine catecholamines, sensitivity of metanephrines > VMA • Adrenal MRI, MIBG functional scan • MEN2A genetic testing Catecholamine Receptors • • • • • • Alpha -vasoconstriction -iris dilation -bronchoconstriction -cardiac contractility -hepatic glucose production • • • • Beta -cardioacceleration -bronchodilation -lipolysis Pre-op Rx • Block Adrenergic receptors • Alpha blockade before beta – Phenoxybenzamine, phentolamine • Beta blockade when orthostatic – Propanolol for non-selectivity, metoprolol or atenolol for β1 selection • ?labetolol Other Rx • Hydration • Intra-cardiac monitoring • Severe HTN, arrhythmias – During induction, tumor manipulation, or anytime! • Nipride • Laparoscopic surgery Surgical Outcome • 1% operative mortality • 5-10% recur, ?MEN syndrome • Catecholamine levels can remain elevated for several weeks • Persistent HTN suggests missed tissue • Malignant pheos 45% 5-year survival, ?I131-meta-iodo-benzylguanidine Take-home Points • Catecholamines needed for daily life and stress responses • Medulla and sympathetic system linked • Pheos rare but one of few chances to cure HTN • Pre-op medical Rx important • Operative events raises your own catecholamines! Reference • Diagnostic and therapeutic strategies in pheochromocytoma, M.S. Golub, The Endocrinologist, 1992;2:101-6. Questions?