Case Presentation Continued
advertisement

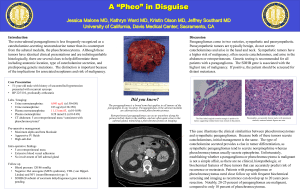
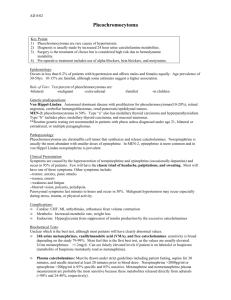
An Abnormal Case of an Abnormal Headache Peter Stempniewicz, MD and Alex Tatusov, MD Hahnemann University Hospital-Drexel University College of Medicine Philadelphia, PA Objectives • To help diagnose and treat paragangliomas • To differentiate paragangliomas from pheochromocytomas Background • Paragangliomas (PG) are rare neuroendocrine tumors that arise from the extra-adrenal autonomic paraganglia. • PGs can be parasympathetic and thus non-secretory, or they can be sympathetic and have the ability to secrete catecholamines. • Parasympathetic PGs are usually found in the neck, while the sympathetic PG are usually anywhere along the sympathetic trunk below the neck, most commonly in the abdomen. Case Presentation CC: Headache, palpitations, feeling of impending doom HPI: The patient was a 76 year old female who originally presented to the ER with complaints of palpitations, headache, high blood pressure and a sensation of impending doom. She said that she was in her usual state of health until the week prior where she had an episode of chest wall pounding that was associated with a sensation of “impending doom.” She was able to measure her blood pressure at that time, and it was measured to be around 180/100. She never had any history of hypertension before, so she went to an urgent care clinic, where she was prescribed a low dose of amlodipine. Since then, she still had several similar episodes in the past week, and then was told to go to the emergency room by her cardiologist, who she had called. These symptoms had no triggers or particular time of onset. She denied any associated diaphoresis, nausea, vomiting, cough, shortness of breath, fevers, chills, lightheadedness, or seizures. PMH: Hypothyroidism, hyperlipidemia, and a benign non-secretory paraganglioma that was resected from her chest 5 years prior. PE: Unremarkable Initial Labs: CBC, CMP, TSH were unremarkable. However, given her symptoms there was concern for a pheochromocytoma, so plasma fractionated catecholamines were checked. RESEARCH POSTER PRESENTATION DESIGN © 2012 www.PosterPresentations.com Case Presentation Continued She was feeling better the next day, so she was discharged home, but then later came back 5 days later with similar complaints, with the addition of left facial and left leg parasthesias. The results of her previously ordered plasma fractionated catecholamines had come back by this time, and they were found to be elevated. The lab results revealed an elevated norepinephrine of 845 pg/ml (NL<420) and an elevated total catecholamines of 863 pg/ml (NL<504). Chromogranin A was also elevated at 6 nmol/L (NL<5). She was started on an alpha receptor antagonist, and had a CT scan of the abdomen and chest to look for a pheochromocytoma or recurrent paraganglioma in her chest. CT scan of the abdomen was negative for pheochromocytoma and the CT scan of the chest was negative for recurrent paraganglioma. This lead to some head scratching, so a 24 hour urine metanephrine was also checked, but came back within normal limits, most likely since it was measured after the episodic event. A CT scan of the neck was then decided upon, which showed an enhancing mass splaying the left carotid bulb measuring approximately 17x12x14 mm. The mass had asymmetric enhancement on the right side and somewhat heterogeneous internal enhancement characteristic of a paraganglioma. Afterwards, she decided that she wanted to have the surgery at another hospital that was closer to where she lived, and was shortly discharged. Figure 1. CT of the neck showing an enhancing mass splaying the left carotid bulb. Figure 2. There are several staging systems used to classify carotid body tumors, with the Shamblin criteria being the most used: • Type I tumors are localized with splaying of the carotid bifurcation but little attachment to the carotid vessels • Type II tumors partially surround the carotid vessels • Type III tumors intimately surround the carotids • Type IIIB tumors are of any size that are intimately adherent to the carotid vessels Discussion Paraganliomas are neuroendocrine tumors that arise from embryonic neural crest cells and are found at autonomic paraganglia. They are cellularly identically to the more known pheochromocytomas, with the main difference being location. The two terms have changed in definition over time. In the 2004 WHO classification, the term pheochromocytoma is reserved for adrenal catecholamine secreting tumors, while paraganglioma is the term used to describe extraadrenal tumors of sympathetic or parasympathetic paraganglia origin (regardless of secretory status). Catecholamine-secreting paragangliomas often present clinically with hypertension, episodic headache, sweating, and tachycardia. Secretory paragangliomas are found in the sympathetic paraverterbral ganglia of the thorax, abdomen, and pelvis, with around 75% being located in the abdomen. Only about 5% of paragangliomas arising within the skull base and neck region are secretory. Resection is the definitive treatment for secretory paragangliomas. Alpha blockade is usually given 10-14 days prior to resection. References 1. The North American Neuroendocrine Tumor Society consensus guideline for the diagnosis and management of neuroendocrine tumors: pheochromocytoma, paraganglioma, and medullary thyroid cancer. Chen H, Sippel RS, O'Dorisio MS, Vinik AI, Lloyd RV, Pacak K, North American Neuroendocrine Tumor Society (NANETS) Pancreas. 2010 Aug;39(6):775-83. 2. S. Arya, V. Rao, S. Juvekar, and A.K. Dcruz.Carotid Body Tumors: Objective Criteria to Predict the 4. Shamblin Group on MR ImagingAJNR Am J Neuroradiol August 2008 29: 13493. http://www.uptodate.com/contents/ paragangliomas-epidemiology-clinical-presentationdiagnosis-and-histology 4. http://www.uptodate.com/contents/ paragangliomas-treatment-of-locoregional-disease