ADRENAL MEDULLA 6
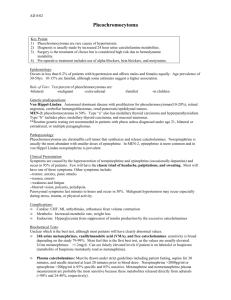
advertisement

ADRENAL MEDULLA ADRENAL MEDULLA • Inner part of adrenal gland • Neural in origin • Formed in parallel with peripheral nervous system • Composed of chromaffin cells (phaeochromocytes) with wide venous sinusoids permeating between them HORMONES PRODUCED • Catecholamines – Epinephrine (adrenaline) 80-90% – Norepinephrine (noradrenaline) 10-20% – Dopamine General features of adrenal medullary secretion • Half-life of the catecholamines is only about 2 minutes. Metabolic end-products include metanephrines and vanillylmandelic acid (VMA) both of which can be measured in plasma and urine • Removal of the adrenal medulla reduces plasma epinephrine to very low levels but does not alter plasma norepinephrine. Difference between the actions of epinephrine and norepinephrine • First, epinephrine, has greater effect in stimulating the beta receptors, has a greater effect on cardiac stimulation than does norepinephrine. • Second, epinephrine causes only weak constriction of the blood vessels in the muscles, in comparison with much stronger constriction caused by norepinephrine. • A third difference; Epinephrine has 5 to 10 times as great a metabolic effect as norepinephrine. General features of adrenal medullary secretion • Because many of the actions of epinephrine are also mediated by nor-epinephrine, the adrenal medulla is not essential for life. • The vasoconstrictive action of norepinephrine is essential for the maintenance of normal blood pressure, especially when an individual is standing. Plasma norepinephrine levels double when one goes from a lying to a standing position. People with inadequate production of nor-epinephrine suffer from orthostatic hypotension. • Epinephrine is a stress hormone and rapidly increases in response to exercise, exposure to cold, emergencies, and hypoglycemia Major metabolic actions of epinephrine • Liver: Epinephrine increases the activity of liver and muscle phosphorylase, promoting glycogenolysis. This increases glucose output by the liver. • Skeletal muscle: Epinephrine promotes glycogenolysis but because muscle lacks glucose-6-phosphatase, glucose cannot be released by skeletal muscle; instead, it must be metabolized at least to lactate before being released into the circulation. • Adipose tissue: Epinephrine increases lipolysis in adipose tissue by increasing the activity of hormone-sensitive lipase. Glycerol from TG breakdown is a minor substrate for gluconeogenesis. • Epinephrine increases the metabolic rate. This will not occur without thy-roid hormones or the adrenal cortex Physiological actions of catecholamines • Role in stress & emotions – Catecholamines participate along with sympathetic nervous system – Brings about changes in various body systems & metabolism to meet the effect of stress effectively – Fright, fight or flight reaction (emergency) Circulatory changes produced in humans by the slow intravenous infusion of epinephrine and norepinephrine EFFECTS OF CATECHOLAMINES ON CVS On total peripheral resistance On heart rate Epinephrine Epinephrine • Vasodilation so ↓ TPR Norepinephrine • Vasoconstriction so ↑ TPR • ↑ HR & force of contraction (Direct action) Norepinephrine • ↓ HR (Reflex mechanism) - Marey’s reflex EFFECTS OF CATECHOLAMINES ON CVS ON BLOOD PRESSURE ON CARDIAC OUTPUT EPINEPHRINE EPINEPHRINE • ↑ SBP – DUE TO INCREASED H.R. • ↓ DBP – DUE TO VASODILATION • ↑ PULSE PRESSURE • ↑ C.O. NOREPINEPHRINE • ↓ C.O. • ↑ BOTH SBP & DBP • ↓ / N PULSE PRESSURE DUE TO DIRECT EFFECT H.R. NOREPINEPHRINE DUE TO ↓ HR Applied aspects - PHAEOCHROMOCYTOMA • Tumours of adrenal medulla • Usually benign • Secrete large amounts of epinephrine & norepinephrine Features : • • • • • • • • Hypertension Headache Sweating Palpitation Anxiety Increased body temperature Hyperglycemia Increased urinary excretion of catecholamines, metanephrines and VMA • Paragangliomas are extrarenal pheochromocytomas of sympathetic ganglia located primarily within the abdomen and that secrete norepinephrine. • Pheochromocytomas are highly vascular and encapsulated. • Episodic release of hormone, particularly when it is mainly norepinephrine, can abruptly cause a hypertensive crisis. Can be induced by physical stimuli that displaces abdominal contents. • Most reliable screening is plasma or urine metanephrines. • Usually curable but can be fatal if undiagnosed Helen Ames is a 51-year-old homemaker who experienced what she thought were severe menopausal symptoms. These awful “attacks” were becoming more frequent. Her heart raced and pounded; she had a throbbing headache and visual disturbances; she felt hot, but her hands and feet were cold; and she was nauseated, sometimes to the point of vomiting. Mrs. Ames called her physician, who agreed that the symptoms were probably menopausal and prescribed hormone replacement therapy over the phone. Mrs. Ames took the hormones (a combination of estrogen and progesterone), but they did not relieve her symptoms. The attacks were occurring almost daily. She made an appointment with her physician. In the physician’s office, Mrs. Ames’ blood pressure was severely elevated at 200/110, and her heart rate was increased at 110 beats/min. To rule out a pheochromocytoma (a rare tumor of the adrenal medulla), the physician ordered a 24-hour urine measurement of vanillylmandelic acid (VMA). To his surprise, the results of the 24-hour urinary VMA test were positive, a finding that provided nearly conclusive evidence of a pheochromocytoma. A computed tomographic scan confirmed that Mrs. Ames had a 3-cm mass on her right adrenal gland. While awaiting surgery to remove the tumor, she was given phenoxybenzamine, an α1-adrenergic antagonist. After an appropriate dosage of phenoxybenzamine was established, she was also given a low dose of propranolol, a β-adrenergic antagonist. She was cleared for surgery when the medications had decreased her blood pressure to 140/90. 1. What is the relationship of the adrenal medulla to the autonomic nervous system? 2. What hormones are secreted by a pheochromocytoma? 3. Why does an elevated urinary level of VMA (a metabolite of epinephrine and norepinephrine) suggest the presence of a pheochromocytoma? 4. In view of the pathophysiology of pheochromocytoma, explain Mrs. Ames’ symptoms, specifically her increased heart rate, pounding heart, cold hands and feet, visual disturbances, and nausea and vomiting. What receptors are involved in each of these symptoms? 5. Why are two values reported for arterial pressure, and what is the significance of each value? Why were both the systolic and diastolic blood pressures elevated? 6. Is there a plausible explanation for the fact that Mrs. Ames felt hot, even though her hands and feet were cold? 7. How did phenoxybenzamine lower Mrs. Ames’ blood pressure? 8. After the dosage of phenoxybenzamine was established, what was the goal of adding a low dose of propranolol? 9. What might have happened if Mrs. Ames had been given propranolol alone?