Journal of Orthopaedic Research 19 (2001) 436±440
www.elsevier.nl/locate/orthres
Ischemia causes muscle fatigue
Gita Murthy a, Alan R. Hargens b, Steve Lehman c, David M. Rempel a,*
a
Ergonomics Program, Department of Bioengineering, University of California, 1301 South 46th Street, Building 112 Richmond,
Berkeley and San Francisco, CA, USA
b
Department of Orthopaedics, University of California, San Diego, CA, USA
c
Department of Bioengineering, University of California, Berkeley, CA, USA
Received 24 March 2000; accepted 3 November 2000
Abstract
The purpose of this investigation was to determine whether ischemia, which reduces oxygenation in the extensor carpi radialis
(ECR) muscle, causes a reduction in muscle force production. In eight subjects, muscle oxygenation (TO2 ) of the right ECR was
measured noninvasively and continuously using near infrared spectroscopy (NIRS) while muscle twitch force was elicited by
transcutaneous electrical stimulation (1 Hz, 0.1 ms). Baseline measurements of blood volume, muscle oxygenation and twitch force
were recorded continuously, then a tourniquet on the upper arm was in¯ated to one of ®ve dierent pressure levels: 20, 40, 60
mm Hg (randomized order) and diastolic (69 9.8 mm Hg) and systolic (106 12.8 mm Hg) blood pressures. Each pressure level
was maintained for 3±5 min, and was followed by a recovery period sucient to allow measurements to return to baseline. For each
respective tourniquet pressure level, mean TO2 decreased from resting baseline (100% TO2 ) to 99 1.2% (SEM), 96 1.9%, 93 2.8%, 90 2.5%, and 86 2.7%, and mean twitch force decreased from resting baseline (100% force) to 99 0.7% (SEM), 96 2.7%, 93 3.1%, 88 3.2%, and 86 2.6%. Muscle oxygenation and twitch force at 60 mm Hg tourniquet compression and above
were signi®cantly lower (P < 0:05) than baseline value. Reduced twitch force was correlated in a dose-dependent manner with
reduced muscle oxygenation (r 0:78; P < 0:001). Although the correlation does not prove causation, the results indicate that ischemia leading to a 7% or greater reduction in muscle oxygenation causes decreased muscle force production in the forearm extensor
muscle. Thus, ischemia associated with a modest decline in TO2 causes muscle fatigue. Ó 2001 Orthopaedic Research Society.
Published by Elsevier Science Ltd. All rights reserved.
Introduction
In the workplace, localized muscle fatigue can be a
limiting factor for prolonged static work [25]. Along
with the shoulder supraspinatus and the neck muscles,
wrist extensor muscles, such as the extensor carpi radialis longus and brevis, are common sites of pain in the
workplace [3,5,25]. Sustained activation of the ECR is
required for the common tasks of wrist stabilization
during forearm pronation, supination, and ®nger extension, pinch and grip tasks. Because many occupations require sustained use of the ECR muscle, it is
important to study the etiology of fatigue in this muscle
to prevent discomfort and potential muscle injury.
Muscle fatigue may be de®ned as the failure to
maintain the required or expected force [12]. Muscle
fatigue can be caused by numerous central and periph*
Corresponding author. Tel.: +1-510-231-5720; fax: +1-510-2315729.
E-mail address: rempel@itsa.ucsf.edu (D.M. Rempel).
eral processes [14]. Among them, impairment of excitation±contraction coupling and alteration of contractile
properties by changes in concentrations of metabolic
product [2] are commonly studied and potentially important mechanisms. Reduced blood ¯ow [4,9] or decreased muscle oxygenation [20] has also been associated
with fatigue. In canine gastrocnemius muscle, Hogan
and colleagues [19] demonstrated a 30% reduction in
force with a 67% reduction in arterial oxygenation,
while no change in other intracellular metabolic processes was noted. However, in human experiments, the
association between hypoxia and fatigue (reduction in
muscle force) has proved controversial [11,13,20,31].
Although a few human studies show association [13,21]
between hypoxia and reduced muscle force production,
these studies often involve high-intensity exercise protocols to induce fatigue. Thus, the cause of fatigue may
be confounded by factors other than hypoxia such as
acidosis, which is also implicated in causing fatigue [14].
In a previous study of human ECR muscle, our group
demonstrated a signi®cant reduction in muscle oxygen-
0736-0266/01/$ - see front matter Ó 2001 Orthopaedic Research Society. Published by Elsevier Science Ltd. All rights reserved.
PII: S 0 7 3 6 - 0 2 6 6 ( 0 0 ) 9 0 0 1 9 - 6
G. Murthy et al. / Journal of Orthopaedic Research 19 (2001) 436±440
ation during contractions as low as 10% maximum
voluntary contraction (MVC) [28]. Although muscle
fatigue was not measured directly, perceived fatigue, as
estimated by the Borg's scale [6], increased linearly with
decreasing muscle oxygenation. To test the hypothesis
that a modest reduction in blood ¯ow, leading to reduced muscle oxygenation, causes fatigue, muscle force
production was studied with graded tourniquet compression.
Materials and methods
Eight subjects (®ve males, three females; age 32 11, mean SD)
participated in the study after giving their informed written consent.
All subjects were in good health and had no history of upper extremity
musculoskeletal disorders or surgeries. The study was approved by the
Human Research Institutional Review Boards at the University of
California at Berkeley and San Francisco.
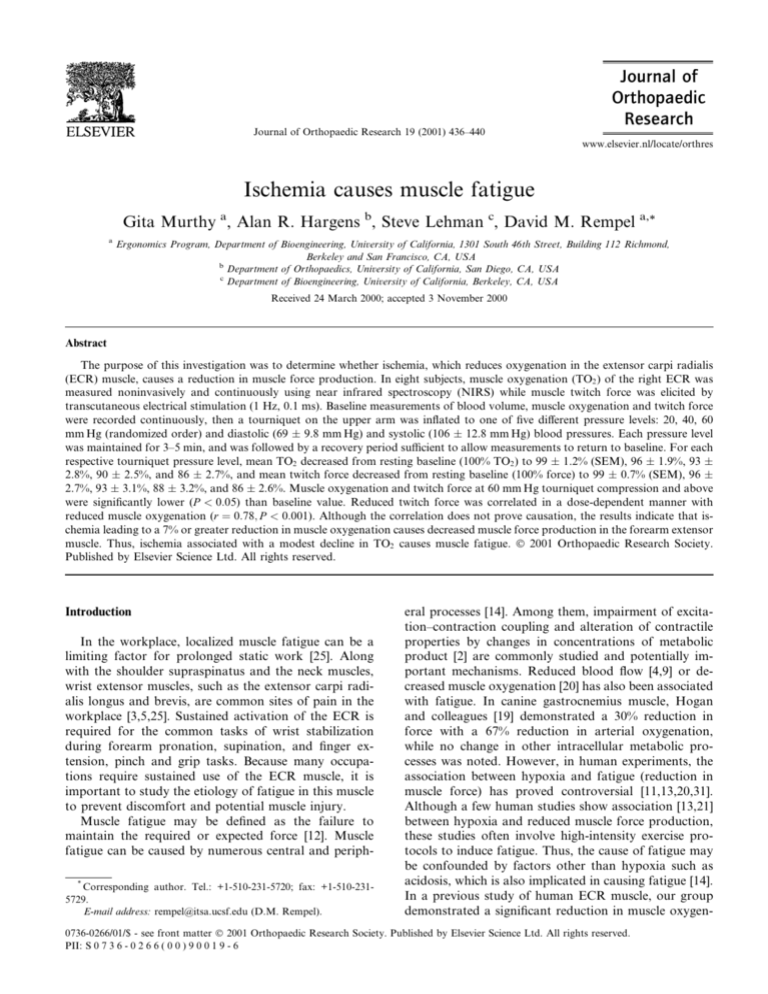
Subjects were seated in a chair, with shoulder abducted to 45° and
elbow ¯exed to 90° (Fig. 1). The right forearm was pronated 45° and
forearm was supported on the surface of an adjustable height. Subjects
performed no active exercise during the protocol; they were instructed
to relax their forearm and ®nger extensor muscles while their wrists
involuntarily extended as a result of electrical stimulation applied to
the ECR muscle.
Blood pressure was measured using a mercury manometer, ECR
muscle blood volume and oxygenation was measured using near infrared spectroscopy (NIRS; RunMan, NIM, Philadelphia, PA), and
Fig. 1. Experimental set-up of subject with tourniquet cu. The ace
bandage around the extensor carpi radialis muscle of the forearm secures an electrode to stimulate the muscle, and the near infrared
spectroscopy probe that detects muscle oxyhemoglobin and oxymyoglobin. The jig over the dorsum of the hand suspends the load cell over
the metacarpophalangeal joint and measures applied force as the wrist
extends with each 1 Hz electrical pulse.
437
forearm muscle twitch force production was measured during muscle
electrical stimulation. The NIRS device detects relative changes of
absorbency for oxygenated and deoxygenated hemoglobin and myoglobin [10]. The dierence in absorbency between two ®lters speci®c for
the oxy- or deoxyhemoglobin and myoglobin, respectively, re¯ects the
deoxygenation state of the muscle. The sum of the absorbency of the
two ®lters re¯ects total blood volume beneath the NIRS probe [18].
Muscle twitches were produced by transcutaneous stimulation of the
ECR using 1 Hz, 0.1 ms, 33 5 mA impulses (Grass S48 Stimulator,
Quincy, MA) over the skin of the ECR muscle belly. The skin over the
ECR muscle was shaved if necessary and cleaned with alcohol. A small
electrode (8 mm; in vivo Metrics, Healdsburg, CA) was secured on the
skin over the muscle belly at a site evoking maximal twitches. A larger
electrode (10 mm diameter) was placed over the bone on the lateral
side of the elbow joint. The twitch induced a wrist extension moment
that was measured using a load cell (Greenleaf, Menlo Park, CA)
placed above the dorsum of the second digit, just proximal to the
metacarpophalangeal joint. The magnitude of electrical stimulation
was de®ned as the electrical current above which the subject could no
longer tolerate a stimulus. This stimulus intensity was submaximal, as
determined by each subject. In a pilot study (n 4), 1 h of 1 Hz
stimulation of the ECR muscle did not by itself cause fatigue.
Muscle oxygenation and blood volume were measured using a
¯exible NIRS probe (8 3 cm dimensions), which was placed on the
ECR muscle belly and secured with an ace bandage, over the electrical
stimulation electrode. The depth of penetration of light from the NIRS
probe was estimated to 1±1.5 cm [30]. Proper placement of the probe
was veri®ed by observing muscle oxygenation changes during voluntary ECR muscle contraction.
A 14 cm wide tourniquet cu was wrapped around the right upper
arm. The experiment began with ECR muscle stimulation at one pulse
per second. Muscle blood volume, oxygenation, and twitch force values were measured continuously. All data were collected continuously
at 50 samples per second and processed using LabView 5.0 software
with a National Instrumentsâ data acquisition board (Austin, TX).
Twitch force potentiated during the ®rst 10 min then stabilized. The
cu was then in¯ated to one of ®ve pressure levels: 20 mm Hg, 40
mm Hg, 60 mm Hg, and subjects' diastolic and systolic blood pressures. The order of cu pressures was randomized. The cu was in¯ated to each pressure level within 15 s, and was maintained until
muscle oxygenation and twitch force values stabilized (3±5 min) and
then released for recovery. Recovery period lasted 5±15 min depending
on whether all measured variables returned to baseline levels.
At the end of the experimental protocol, the subject raised the right
arm vertically above head to drain the venous circulation and to
provide a minimum blood volume value. Next, a tourniquet cu was
in¯ated to 250 mm Hg to induce complete ischemia. A 2 kg weight was
suspended o the subjects' second and third metacarpophalangeal
joint, and subjects performed dynamic wrist extensions until oxygenation stabilized to a minimum value for about 5 s (ischemia), then the
cu was released. Muscle blood volume and oxygenation from each
subject, during the last 10 s of each cu compression level, were normalized to baseline (100% TO2 ) and ischemia (0% TO2 ).
The experiment was a repeated measures design, and Tukey's test
followed RANOVA analysis [15] when appropriate. Although muscle
oxygenation and blood volume were altered by tourniquet cu, muscle
oxygenation and blood volume are considered independent variables,
and twitch force is considered the dependent variable. Data were analyzed during the last 10 s of tourniquet compression. Mean values
were calculated for all measures (peak twitch force, mean twitch force,
TO2 ) across the last 10 s of tourniquet compression. Multiple regression analysis assuming dependent observations from repeated measures design was used to evaluate association between muscle
oxygenation and twitch force. In all cases, alpha was set at 0.05. Data
reported are means SEM, unless otherwise stated.
Results
Representative data from one subject showing muscle
oxygenation, blood volume, and twitch force at each
of the compression levels are presented in Fig. 2.
438
G. Murthy et al. / Journal of Orthopaedic Research 19 (2001) 436±440
Tourniquet compression was applied for a 3±5 min
period for each load. During compression, muscle
oxygenation and twitch force declined, and blood
volume increased. Between compressions, peak twitch
force and TO2 returned to within 10% of baseline before
the next compression began. During the ischemia part of
the protocol, muscle blood volume and oxygenation
levels reached minimum values within 5 min of activeloaded wrist exercise (Fig. 2f).
In all subjects (n 8), blood volume (Fig. 3) increased
and TO2 and twitch force (Fig. 4) decreased with increasing tourniquet compression levels. Muscle oxygenation decreased from resting baseline (100% TO2 ) to
99 1.2% (SEM), 96 1.9%, 93 2.8%, 90 2.5%,
and 86 2.7% at 20, 40, 60 mm Hg, 69 9.8 mm Hg,
and 106 12.8 mm Hg, respectively (Fig. 4). Mean
blood volume increased signi®cantly (P < 0:05) from
resting baseline (100% blood volume) to 112 2.7%,
133 8.4%, 144 15.4%, 144 12.2%, and 150 12.5% at 20, 40, 60 mm Hg, 69 9.8 mm Hg, and 106 12.8 mm Hg, respectively (Fig. 3), and plateaued above
60 mm Hg compression. Mean twitch force decreased
from resting baseline (100% force) to 99 0.7% (SEM),
96 2.7%, 93 3.1%, 88 3.2%, and 86 2.6% at 20,
40, 60 mm Hg, 69 9.8 mm Hg, and 106 12.8 mm Hg,
respectively (Fig. 4).
The correlation (r 0.78) between TO2 and twitch
force was statistically signi®cant (slope 0.88, RANOVA P < 0:001; R2 0:60; Fig. 5). Twitch force was
signi®cantly lower (Tukey test, P < 0:05) than baseline
when TO2 levels declined by 7% or more.
Fig. 3. Normalized extensor carpi radialis muscle blood volume (%
baseline) during 20, 40, 60 mm Hg, and diastolic and systolic tourniquet cu pressure levels (n 8). Error bars S.E.M.
Fig. 4. Normalized muscle oxygenation and twitch force production
during 20, 40, 60 mm Hg, and diastolic and systolic tourniquet cu
pressure levels (n 8). * Denotes signi®cantly lower (P < 0:05) value
than baseline 0 mm Hg compression. Error bars S.E.M.
Fig. 2. Typical data of twitch force, blood volume, and muscle oxygenation (TO2 ) during ®ve dierent levels of tourniquet compression
levels. For this subject, a 40 mm Hg, b 60 mm Hg, c 20 mm Hg,
d diastolic blood pressure, e systolic blood pressure, and f ischemic period. This ischemia (250 mm Hg) is performed to calibrate
the near infrared spectroscopy device so that the minimum value obtained is considered physiologic 0% for muscle blood volume and
oxygenation.
Fig. 5. Normalized twitch force as a function of muscle oxygenation in
the forearm extensor carpi radialis muscle (n 8; R2 0.60). Error
bars S.E.M.
G. Murthy et al. / Journal of Orthopaedic Research 19 (2001) 436±440
Discussion
This study demonstrates a signi®cant correlation between a decline in TO2 and a drop in twitch force during
tourniquet compression. Overall, a 7% or greater decrease in TO2 was associated with a signi®cant decrease
in ECR muscle force production. Although association
does not indicate causation, these ®ndings suggest that
ischemia and the resultant muscle hypoxemia cause
muscle fatigue.
Muscle fatigue induced by ischemia may be explained
by factors such as reduced clearance of H or phosphates from the muscle due to impaired circulation,
limited oxygen or other substrate delivery to the ECR
muscle, a decoupling of the excitation±contraction
process, or reduced excitation [14].
The tourniquet compression, especially near or above
the diastolic pressure, may reduce blood ¯ow to the
ECR muscle and hence limit catabolite clearance. Although ischemia was not quanti®ed directly in the experiment, 60 mm Hg was near the mean diastolic
pressure in the subjects, and is probably sucient to
cause venous occlusion. Vascular occlusion, especially at
levels of compression exceeding diastolic blood pressure,
can cause venous engorgement within seconds [16,26]. In
dogs, Meninger and Baker [26] showed two phases of
hemodynamic changes with venous occlusion. As the
venous compression increased from 5 to 40 mm Hg, an
initial rapid increase in total tissue volume occurred.
This change in volume was attributed to venous engorgement. Secondary to the rapid vascular volume increase, there is a gradual volume expansion, which was
explained by interstitial volume increase resulting from
transcapillary ¯uid ¯ux. The investigators demonstrated
that the increase of interstitial ¯uid, i.e., edema, also
occurs within seconds of venous occlusion [24,26].
In the present study, a similar linear increase in blood
volume seen as tourniquet compression increased from
20 to 60 mm Hg (Fig. 3) may be indicative of such venous engorgement. It is possible that the engorgement
from tourniquet application aects the strength of
electrical stimulation, thereby arti®cially reducing the
force produced by the extensor muscle. However, this is
an unlikely possibility because if a reduction in twitch
force is a function of venous engorgement and increased
limb volume, then force should decrease in proportion
to blood volume. Data from the present study indicate
poor correlation between force production and muscle
blood volume (r )0.38), thereby suggesting that this
argument is probably not valid.
Blood volume measurement from the NIRS device is
most likely accounted for by an increase in hemoglobin
and myoglobin, either oxygenated or deoxygenated [17].
Because we did not monitor forearm interstitial volume
change, we cannot conclude that muscle edema occurred. However, based on existing literature [16,24,26]
439
it is possible that edema accompanied venous engorgement. It is likely that venous occlusion limited removal
of metabolic products from the exercising ECR muscle.
Among metabolic products, H and Pi are known to
cause fatigue [8,27,29]. Furthermore, increase in H ion
concentration has been demonstrated to produce a
larger force reduction in the type IIb ®bers compared to
type I ®bers [32], and the ECR muscle is predominantly
composed of type IIb ®bers [22].
In addition to limiting catabolite removal, tourniquet
compression at or above 60 mm Hg may have reduced
blood ¯ow to the ECR muscle and hence reduced delivery of substrates besides oxygen that are critical for
energy production. Reduced blood ¯ow combined with
possible edema may have limited availability of bloodborne glucose or fatty acids. However, it is unlikely in
this study that the ECR muscle twitches signi®cantly
altered substrate delivery, as the muscles themselves
contain adequate glycogen stores.
The fatigue produced in this study may also be due to
reduction in excitation±contraction coupling, including
excitability to T-tubules, release of Ca2 , and sensitivity
of regulating proteins to Ca2 [1]. However, recovery
from fatigue due to changes in excitation±contraction
coupling is typically very slow [2]. Recovery of ECR
twitch force in this study was immediate following release of tourniquet cu. Thus, the decoupling of excitation±contraction mechanism is not likely to explain
the muscle fatigue measured in this study.
Likewise, it may be proposed that the fatigue is due to
de®cient muscle excitation. The tourniquet cu in our
experiment may have constricted the radial nerve that
supplies the ECR muscle, reduced action potential
transmission, and thereby decreased twitch force production. Although nerve conduction velocity or the M±
wave to assess nerve function was not measured in this
study, it is dicult to support such a mechanism. A
previous in vivo study in humans indicates that motor
function is not aected at 80 mm Hg tourniquet compression until the compression is applied for 30 to 50
min [23]. Furthermore, in another study [7], tourniquet
compression of 113 mm Hg applied directly over the
biceps brachii also showed no change in the M±wave
and nerve conduction velocity. Since the compression
applied in this study lasted a maximum of 5 min at each
pressure level, ranging from 20 to 106 mm Hg, and since
the muscle was directly stimulated, it is unlikely that
radial nerve function was altered.
Because ECR muscle volume, H ion concentration,
pH, or Ca2 sensitivity were not measured, it is dicult
to draw ®rm conclusions about the mechanism of
muscle fatigue in this study. Moreover, to conclude that
reduced oxygenation alone caused muscle fatigue may
be inaccurate because hypoxemia was induced using a
tourniquet cu. The cu impedes circulation and
thereby confounds the eects that hypoxia alone may
440
G. Murthy et al. / Journal of Orthopaedic Research 19 (2001) 436±440
have on muscle fatigue. However, we can conclude that
ischemia associated with a modest decline in tissue oxygen causes muscle fatigue. Future studies, whereby
only oxygen levels are altered without compromising
blood perfusion, are warranted to investigate the unique
role of oxygen in fatigue.
Acknowledgements
We thank the enthusiastic participation of our subjects and Drs. RH Fitts, MC Hogan, M Hudes, and P
Johnson for helpful discussion. We also thank Ms.
Karen Hutchinson for technical assistance. This research was supported by NASA-Headquarters Graduate Student Research Fellowship.
References
[1] Allen DG, Lee JA, Westerblad H. Intracellular calcium and
tension in isolated single muscle ®bers from Xenopus. J Physiol
(Lond) 1989;415:433±58.
[2] Allen DG, Westerblad H, Lee JA, Lannergren J. Role of
excitation±contraction coupling in muscle fatigue. Sports Med
1992;13(2):116±26.
[3] Armstrong T, Buckle P, Fine L, Hagberg M, Jonsson B, Kilbom
A, et al. A conceptual model for work-related neck and upperlimb musculoskeletal disorders. Scand J Work Environ Health
1993;19:73±84.
[4] Barcroft H, Millen JLE. The blood ¯ow through muscle during
sustained contraction. J Physiol (Lond) 1939;97:17±31.
[5] Bernard B, Sauter S, Petersen M, Fine L, Hales T. Los Angeles
Times. In: CDC NIOSH Health Hazard Evaluation Report,
HETA 90-013-2277, 1993.
[6] Borg GAV. Psychophysical basis of perceived exertion. Med Sci
Sports Exercise 1982;14(5):371±81.
[7] Brown T, Galea V, McComas A. Loss of twitch torque following
muscle compression. Muscle & Nerve 1997;20(2):167±71.
[8] Byrd SK, McCutcheon LJ, Hodgson DR, Gollnick PD. Altered
sarcoplasmic reticulum function after high-intensity exercise. J
Appl Physiol 1989;67:2072±7.
[9] Bystrom EG, Kilbom A. Physiological response in the forearm
during and after isometric intermittent handgrip. J Appl Physiol
1990;60:457±66.
[10] Chance B, Nioka S, Kent J, McCully K, Fountain M, Greenfeld
R, et al. Time-resolved spectroscopy of hemoglobin and myoglobin in resting and ischemic muscle. Analyt Biochem 1988;174:698±
707.
[11] Dodd SL, Powers SK, Brooks E, Crawford MP. Eects of reduced
O2 delivery with anemia, hypoxia, or ischemia on peak VO2 and
force in skeletal muscle. J Appl Physiol 1993;74(1):186±91.
[12] Edwards RHT. Hypotheses of central and peripheral mechanisms
underlying occupational muscle pain and injury. Eur J Appl
Physiol 1988;57:275±81.
[13] Eiken O, Tesch PA. Eects of hyperoxia and hypoxia on dynamic
and sustained static performance of the human quadriceps muscle.
Acta Physiol Scand 1984;122:629±33.
[14] Fitts RH. Cellular mechanisms of muscle fatigue. Circulation Rev
1994;74(1):49±94.
[15] Glantz SA, Slinker BK. Primer of applied regression and analysis
of variance. New York: McGraw-Hill; 1990. p. 381±460 [chapter
9].
[16] Granger HJ, Laine GA, Barnes GE, Lewis RE. Dynamics and
control of transmicrovascular ¯uid exchange. In: Staub NC,
Taylor AE, editors. Edema. New York: Raven Press; 1984. p.
189±228 [chapter 9].
[17] Hampson NB, Piantadosi C. Near infrared monitoring of human
skeletal muscle oxygenation during forearm ischemia. J Appl
Physiol 1988;64:2449±57.
[18] Hayden RE, Tavill MA, Nioka S, Kitai T, Chance B. Oxygenation
and blood volume changes in ¯aps according to near-infrared
spectrophotometry. Arch Otolaryngol Head Neck Surg
1996;122:1347±51.
[19] Hogan MC, Kurdak SS, Arthur PC. Eect of gradual reduction in
O2 delivery on intracellular homeostasis in contracting skeletal
muscle. J Appl Physiol 1996;80(4):1313±21.
[20] Hogan MC, Richardson RS, Kurdak SS. Initial fall in skeletal
muscle force development during ischemia is related to oxygen
availability. J Appl Physiol 1994;77(5):2380±4.
[21] Kaijser L. Limiting factors for aerobic muscle performance. Acta
Physiol Scand (Suppl) 1970;346:1±98.
[22] Ljung B-O, Leiber RL, Friden J. Wrist extensor muscle pathology
in lateral epicondylitis. J Hand Surg (Br) 1999;24(2):177±83.
[23] Lundborg G, Gelberman RH, Minteer-Convery M, Lee YF,
Hargens AR. Median nerve compression in the carpal tunnel±
functional response to experimentally induced controlled pressure.
J Hand Surg 1982;7(3):252±9.
[24] Lundvall JI, Lanne T. Much larger transcapillary hydrodynamic
conductivity in skeletal muscle and skin of man than previously
believed. Acta Physiol Scand 1989;136:7±16.
[25] Magnusson M. Posture. In: Andersson GBJ, Nordin M, Pope
MH, editors. Musculoskeletal disorders in the workplace. St.
Louis: Mosby-Year Book; 1997. p. 74 [chapter 8].
[26] Meninger RP, Baker CH. Vascular and extravascular volume
changes due to elevated venous pressure. Proc Soc Exp Biol Med
1975;148:669±74.
[27] Metzger JM, Moss RL. Eects on tension and stiness due to
reduced pH in mammalian fast- and slow-twitch skinned skeletal
muscle ®bers. J Physiol Lond 1990;428:737±50.
[28] Murthy G, Kahan NJ, Hargens AR, Rempel DM. Forearm
muscle oxygenation decreases with low levels of voluntary
contraction. J Orthop Res 1997;15(4):507±11.
[29] Pate E, Cooke R. A model of crossbridge action: the eects of
ATP, ADP, and Pi. J Muscle Res Cell Motil 1989;10:181±96.
[30] Patterson MS, Chance B, Wilson BC. Time resolved re¯ectance
and transmittance for the noninvasive measurement of tissue
optical properties. J Appl Opt 1989;28:2331±6.
[31] Stainsby WN, Brechue WF, O Drobinak DM, Barclay JK. Eects
of ischemic and hypoxic hypoxia on VO2 and lactic acid output
during tetanic contractions. J Appl Physiol 1990;68:574±9.
[32] Thorstensson A, Karlsson J. Fatigability and ®ber composition of
human skeletal muscle. Acta Physiol Scand 1976;98:318±22.