Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
CARDIOVASCULAR EMERGENCIES
Objectives:
At the completion of this section, the learner will be able to:
Define preload, afterload, cardiac output and stroke volume
Recognize problems with implanted pacemakers that present to the emergency department
List drugs that are used to control tachycardic rhythms
State nursing interventions for a patient experiencing an acute aortic dissection
Differentiate between the symptoms of a right-sided myocardial infarction and a left-sided myocardial infarction
Differentiate treatments implemented for arterial versus venous peripheral vascular occlusions
The CEN exam contains twenty questions on cardiovascular emergencies which involve the following topics:
Acute coronary syndromes
Aneurysm/Dissection
Cardiopulmonary arrest
Dysrhythmias
Endocarditis
Heart Failure
Hypertension
Pericardial tamponade
Pericarditis
Peripheral vascular disease (e.g. arterial, venous)
Thromboembolic disease (DVT)
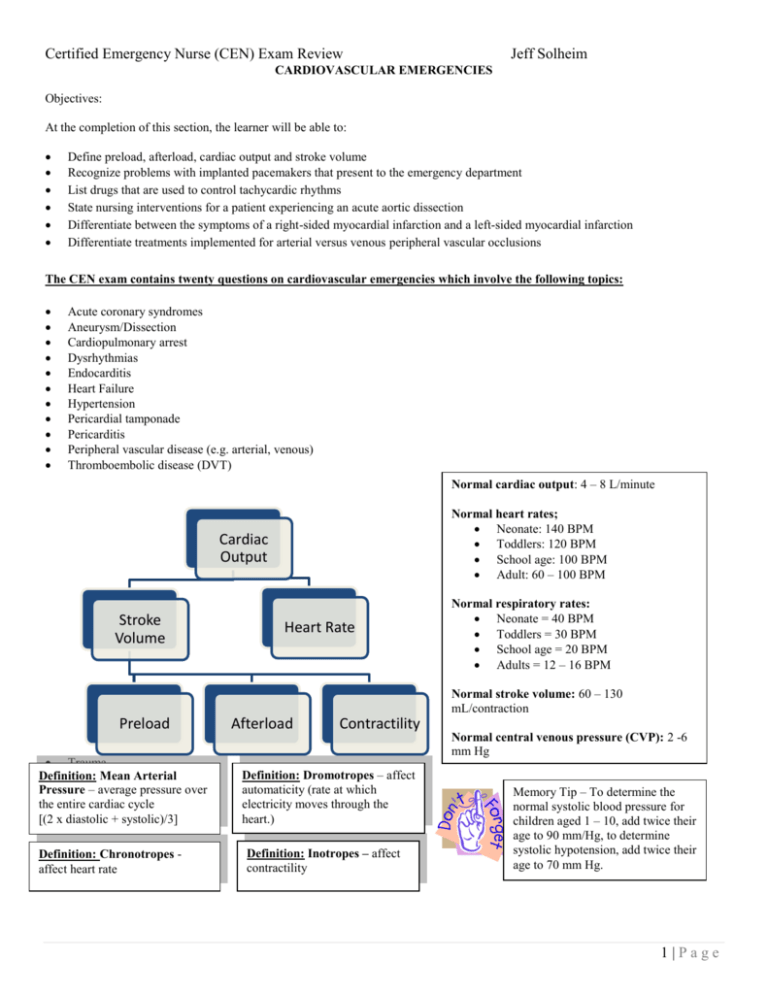
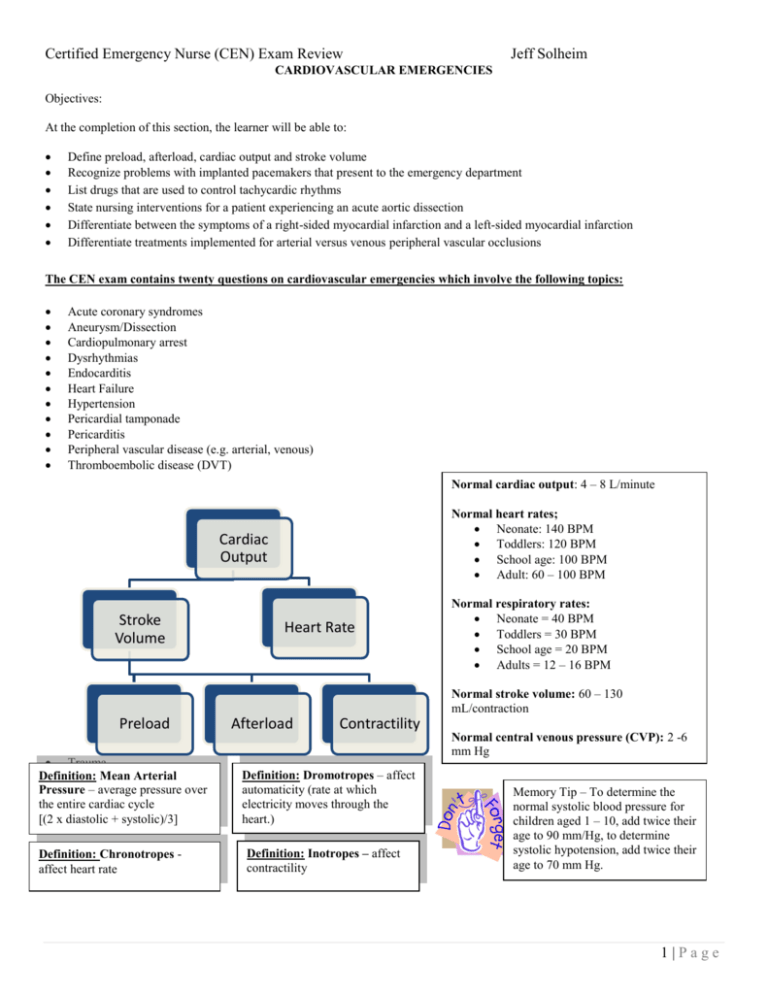
Normal cardiac output: 4 – 8 L/minute
Normal heart rates;
Neonate: 140 BPM
Toddlers: 120 BPM
School age: 100 BPM
Adult: 60 – 100 BPM
Cardiac
Output
Stroke
Volume
Heart Rate
Normal respiratory rates:
Neonate = 40 BPM
Toddlers = 30 BPM
School age = 20 BPM
Adults = 12 – 16 BPM
Normal stroke volume: 60 – 130
mL/contraction
Preload
Trauma
Definition: Mean Arterial
Pressure – average pressure over
the entire cardiac cycle
[(2 x diastolic + systolic)/3]
Definition: Chronotropes affect heart rate
Afterload
Contractility
Normal central venous pressure (CVP): 2 -6
mm Hg
Definition: Dromotropes – affect
automaticity (rate at which
electricity moves through the
heart.)
Definition: Inotropes – affect
contractility
Memory Tip – To determine the
normal systolic blood pressure for
children aged 1 – 10, add twice their
age to 90 mm/Hg, to determine
systolic hypotension, add twice their
age to 70 mm Hg.
1|Page
Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
Cardiovascular pharmacology
o Bradycardia
Atropine (reverses cholinergic-mediated decreases in heart rate)
Use with caution in cases of coronary ischemia and MI
Unlikely to be effective after cardiac transplantation
Not useful in Type II second-degree or third degree heart block
Epinephrine (positive inotrope, dromotrope and chronotrope)
Dopamine - Doses between 2 and 10 mcg/kg/minute effective to increase heart rate.
Pacemaker therapy - pacemakers are used when the heart’s intrinsic pacemaking system is inadequate.
Most effective for bradycardia, heart block and idioventricular rhythms. Two methods of pacing in ED:
External (transcutaneous) –Large electrodes are placed on the skin, one on the back at the
midthoracic level of the spine and a second on the front at the chest lead level of V 3.
Transvenous – involves threading a catheter electrode into the right atrium or ventricle via the
subclavian, internal jugular, brachial, or femoral vein.
o Pacemaker settings
Heart rate (how often the pacemaker fires)
Pacemaker output (strength of pacemaker impulse)
Sensitivity (degree which pacemaker senses intrinsic impulses)
Implanted pacemaker: Problem solving
o Failure to output
Possible causes
Battery failure
Lead problem (lead fracture or fractured lead insulation)
Oversensing
Management: medications to increase intrinsic heart rate, temporary pacemaker.
o Failure to capture
Possible causes
Failing battery
Lead issue (lead fracture, dislodgement, fractured lead insulation)
Exit block
o Ischemia/infarction at endocardium site
o Hyperkalemia
o Class III antiarrhythmic drugs (e.g. amiodarone)
Treatment: correct the problem, temporary pacing
o Oversensing
Causes
Muscular activity
Outside interference (MRI, electrocautery, digital cellular phone)
Management – magnet application
Tachycardia
Cardioversion
o If time allows:
Assess potassium, magnesium and digoxin levels
Remove dentures
Allow patient to go to the bathroom
Remove transdermal medication and patches
Provide conscious sedation
o Set to “sync”, assure sync is working
2|Page
Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
o
Do not give
calcium
channel
blockers or
beta-blockers to
patients with
bradycardia,
heart blocks,
heart failure,
etc.
Set energy level
Narrow and regular QRS complexes: 50 to 100 Joules (J)
Narrow but irregular QRS complexes: 120 to 200 J (biphasic waveform) or 200
J (monophasic waveform)
Wide and regular QRS complexes: 100 J
Wide but irregular QRS complexes: Patient will require defibrillation
(nonsynchronized)
Pediatric: 0.5 – 1 Joule/kg increased to 2 Joule/kg
o Deliver shock after “all clear”
Under breasts of large breasted woman
Shave hairy chests
Do not cardiovert over pacemaker or ICD
o Increase energy if unsuccessful and repeat
Internal cardiac defibrillator
o Malfunctions
Continuous unneeded firing: apply a magnet
Firing during cardiac arrest
Allow ICD to work
Apply magnet if ICD continues to fire but does not convert the rhythm.
Wait 30 seconds after final firing to manually defibrillate
Keep paddles/patches 10 cm away from ICD.
Narrow Complex
o Vagal maneuvers
o Adenosine
Rapid IV push followed by 20 cc saline bolus
May cause transient heart block or asystole
o Calcium channel blockers (-depine)
Vasodilators, negative inotrope, negative chronotrope, negative dromotrope.
o Beta-blockers (-lol)
Vasodilators, negative inotrope, negative chronotrope, negative dromotrope.
Cardioselective beta-blockers – Beta-one blockers only (ideal for patients with
pre-existing pulmonary conditions) E.g. – Propranolol, Nadolol, Timolol,
Pindolol, Carteolol, Penbutolol
Non-cardioselective beta-blockers - beta-one and beta two blocking. E.g. –
Acebutolol, Atenolol, Metoprolol, Esmolol, Betaxolol, Bisoprolol
Wide complex
o Unstable: cardioversion and/or precordial thump (for witnessed arrest on a monitor in the
absence of immediate defibrillation)
o Stable
Procainamide IV
Monitor for:
o Hypotension
o Widening of the QRS complex more than 50%
Amiodarone – may cause nausea, bradycardia, hypotension
Sotalol
3|Page
Certified Emergency Nurse (CEN) Exam Review
o
Drug
Epinephrine (Adrenalin)
Isoproterenol (Isuprel)
Dopamine (Intropin, Dopastat)
Norepinephrine bitartrate
(Levophed)
Phenylephrine (NeoSynephrine)
o
Nitroglycerin
Diazoxide (Hyperstat)
Notes
Positive inotrope, dromotrope and chronotrope as well as vasoconstrictor
alpha, beta-one and beta-two stimulation – can increase myocardial
workload, can cause myocardial ischemia.
alpha, beta-one and beta-two stimulation
2 – 10 mcg/kg/minute cardiac output
> 10 mcg/kg/minute BP
Peripheral venous and arterial vasoconstrictor and cardiac stimulant
considered in the treatment of hypotension or shock.
Pure alpha-agonist
Vasodilators (monitor for hypotension)
Drug
Angiotensin Converter Enzymes
(ACE Inhibitors). End in –pril
Milrinone/Amrinone
Sodium Nitroprusside (Nipride)
Jeff Solheim
Vasoconstrictors (monitor for hypertension. May cause local necrosis in cases of infiltration. Infiltration treated
with phentolamine)
Pharmacology
preload and afterload through
vasodilation and diuresis
Vasodilator/positive inotrope
Potent venous AND arterial dilator
Venous dilator (arterial dilator in higher
doses)
Coronary artery dilator
Arterial dilator for significant hypertension
Notes
Monitor for dry cough, hyperkalemia and
angioedema
Treatment for heart failure
Protect from light (aluminum foil or opaque plastic)
Give IV in glass bottles through PVC tubing.
Inhibits release of insulin (can cause hyperglycemia)
Hypertension
o Severe elevations in blood pressure can lead to:
Hypertensive encephalopathy (altered LOC, dizziness, headache, stroke seizures)
Retinal hemorrhages with visual complaints
Renal damage (hematuria, oliguria)
Chest pain and ischemia
Heart failure (enlarged heart, S3/S4 heart sounds)
Epistaxis
Acute Aortic Dissection (tear in the intimal layer of the aorta, which exposes the degenerated medial layer to the forces of
blood pressure. These forces cleave or dissect the two layers of the arterial wall)
o Ascending Dissection (A)
Most common and lethal
o Descending Dissection (B)
C
o
Descending into Ascending (C)
o
Risk factors
Hypertension
Connective tissue disease (e.g. Marfan’s syndrome)
Pregnancy
Trauma
A
B
4|Page
Certified Emergency Nurse (CEN) Exam Review
o
o
Ascending dissection - pain in the substernal area, throat, jaw or face
Descending dissection - pain in the intrascapular or lower back areas, abdomen, flank and
lower extremities.
Changes in blood pressure (Difference of more then 10 mm Hg when comparing SBP of
various limbs).
Symptoms of spinal cord hypoxia such paresthesia, hemiplegia and paraplegia.
Signs of hypovolemia, hct, WBC ( BUN and creatinine if renal arteries affected)
Treatment
Prepare for rapid deterioration (oxygen, large bore IV)
Blood products and fluid resuscitation as needed.
Narcotics (pain)
Anti-hypertensives
Jeff Solheim
Clinical manifestations
Pain (may be described as a sudden onset tearing, ripping, sharp, knife-like pain not relieved by
analgesics)
Nitroprusside (Nipride)
Labetalol (Normadyne, Trandate)
Calcium channel blockers such as verapamil (Isoptin, Calan) or diltiazem (Cardizem)
Surgical repair/ open thoracotomy
Heart failure[Occurs when the heart can no longer produce sufficient cardiac output at normal filling pressures to meet metabolic
demands (usually when the left ventricular ejection fraction falls below 40%)]
o Clinical manifestations
Right-sided failure
Left-sided failure
o Treatment:
Peripheral edema Hemoptysis
Vasodilators (morphine, Nitroprusside,
Hepatomegaly
Progressive dyspnea
ACE inhibitors)
JVD
Crackles on auscultation
Diuretics
CVP
Increased pulmonary artery pressures
Positive inotropes (lanoxin, dobutamine)
Dopamine to support blood pressure
Coronary artery disease
Symptom progression
Event
Stable angina
Easily relieved by
Pain
rest/NTG
EKG changes
Cardiac
Enzymes
Transient ST
depression
Normal
Unstable angina
Lasts longer than 20
minutes
Transient ST
depression/ T wave
inversion
NSTEMI
Continuous chest
pain
ST segment
depression and T
wave abnormalities
STEMI
Pain described as worse than
angina
ST segment elevation > 2 mm in
leads V , V and V and > 1 mm in
Normal
Elevated
Elevated
1
2
3
all other leads
5|Page
Certified Emergency Nurse (CEN) Exam Review
M
O
Medication
Morphine
Sulfate
Dose
2 -4 mg IV push, repeat q5-30
minutes as needed
Oxygen
Nitroglycerin
4 L/min via nasal cannula
S/L or spray q3-5 minutes
up to 3 doses
12.5 – 25 mcg bolus IV
followed by an infusion 1020 mcg/minute
160 – 325 mg PO (chewable)
N
Aspirin
A
Comments
pain
preload
myocardial oxygen demand
Titrate to keep oxygen saturation above 95%
Limit SBP changes to <10% if normotensive or < 30% if
hypertensive
Hold if SBP < 90 mmHg
Contraindicated for people who have taken Viagra or
Levitra within 24 hours
Maybe repeated in patients who have already taken ASA or
are on daily doses
Location of MI based on changes in various leads
o
•
•
•
•
•
•
•
•
Jeff Solheim
Treatment considerations for a myocardial infarction
Location of MI
Anterior
Expected lead changes
V , V and V
Anterior/Septal
V,V
Lateral
I, AVL, V , V
Inferior
Right Ventricle
II, III, AVF
RV , RV , RV
Posterior
Tall R waves and ST depression in V and V
2
3
4
1
2
5
4
5
6
6
1
2
Thrombolytics
Contraindications
Recent internal bleeding (less than one month prior to arrival)
Known bleeding diathesis
History of cerebrovascular accident
Recent surgery
Intracranial arteriovenous malformations
Uncontrolled hypertension (SBP > 180 mm Hg, DBP > 110 mm Hg)
Trauma within the past ten days
Recent cardiopulmonary resuscitation efforts
•
•
•
•
•
•
•
Relative Contraindications
Minor trauma
Diabetic retinopathy
Pregnancy
Concurrent anticoagulation
Severe trauma in the past six months
Any previous central nervous system
event
Unsuccessful central venous puncture
Monitoring after thrombolytics
Monitor for bleeding
o Venipuncture/ABG puncture sites
o GCS for intracranial bleeding
o Abdominal girth
o Bruising in the flanks
Reduce risk for bleeding
o Minimize movement
o Limit venipunctures/ABGs
o Minimize invasive blood pressures
Monitor for reperfusion
o Resolution of chest pain
o Normalizing ST segment changes
o Reperfusion arrhythmias
6|Page
Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
Right Ventricular Infarct
o Move leads to right side of chest
V1R
Fourth intercostal space along the left sternal border. (same as lead V 2)
V2R
Fourth intercostal space along the right sternal border. (Same as lead V 1)
V3R
Midway between leads V2R and V4R
V4R (V7)
Fifth intercostal space at the right midclavicular line
V5R (V8)
Midway between V4R and V6R in the fifth intercostal space
V6R (V9)
Right midaxillary line at the fifth intercostal space
Symptom
Right side
Left side
Nausea and vomiting
Dyspnea/Orthopnea
Diaphoresis
Tachycardia
Bradycardia
Hypertension
Hypotension
JVD
o Treatment
Fluid loading
Inotropic support
Avoid vasodilators (morphine, nitroglycerin, diuretics)
All other treatments as per MI protocols
Variant angina (also known as variable angina, Prinzmetal’s angina or coronary artery spasms – caused by ischemia secondary
to a spasm in the coronary artery.)
o Often occurs in younger individuals who may have no coronary heart disease
o Causes chest pain that is often more severe than typical angina pain.
Pain tends to be cyclical
Often occurs between midnight and 8 AM
o EKG may show ST elevation that resolves with resolution of pain.
o Treated with nitroglycerin or calcium channel blockers
Infections involving the heart
o Infective Endocarditis (general term used to describe inflammation of the endocardium, especially the cardiac valves)
Clinical manifestations
Signs of infection (Fever, anorexia, weight loss, night sweats, myalgia, fatigue, malaise)
Pain (Pleuritic chest pain, abdominal or back pain
Signs of Embolization (stroke signs, hemoptysis, splinter hemorrhages, petechiae of the conjunctiva,
palate, neck, upper trunk, or extremities, Osler’s nodes, Janeway lesions)
Diagnosis
WBC
ESR
Blood cultures
Echocardiogram
Treatment
Definition: Osler’s
nodes – tender,
subcutaneous nodules,
often in the pulp of the
digits.
Long term IV antibiotics
May require admission with cardiac monitoring
Definition: Janeway
Lesions – non-tender
erythematous,
hemorrhagic, or pustular
lesions often on the palms
or soles
7|Page
Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
Pericarditis (inflammation of the pericardial sac)
o Common causes
MI (2 – 3 days after the MI)
Connective tissue disorders
Renal failure
Mediastinal injury
Neoplasms or radiation
Infectious processes
o Clinical manifestations
Pain (exacerbated by deep inspiration, coughing, swallowing, supine position, but relieved by leaning forward
or sitting up)
Indications of infection (malaise, fever, chills, dyspnea and cough)
Tachycardia and tachypnea
Auscultation of pericardial friction rub
EKG changes
ST segment elevation with upright T waves in all leads except aVR and V 1.
T waves flatten, the ST segment returns to baseline after several days
T wave inversion (it may take weeks or months for the T waves to return to normal).
o
Treatment
Allow patient position of comfort (sitting upright with legs dangling)
Definition: Kussmaul’s
Anti-inflammatory agents
Sign - Elevation of neck
veins with inspiration
Antipyretics
during spontaneous
Antibiotics
breathing
Colchicine (for cases related to gout)
Pericardial tamponade (accumulation of fluid in the pericardial sac)
o Clinical manifestations
Beck’s triad (muffled heart tones, hypotension, JVD)
Kussmaul’s sign
Obstructive shock (narrowing pulse pressure, cool, moist skin, urinary output)
o Treatment
Pericardiocentesis (Emergent cases)
Surgery
Peripheral vascular occlusions
Provacation of pain
Quality of pain
Region and radiation
of pain
Severity of pain
Timing of pain
Objective findings
SYMPTOMS
Arterial occlusion
Pain is always present, it occurs at rest, with
movement and with exercise
May be described as a burning discomfort
Typically hurts from the area of the occlusion
distally because all tissue distal to the occlusion will
be void of adequate oxygen
Described as excrutiating
Pain starts as soon as the occlusion develops and is
not easily relieved
Cold extremity with decreases pulses that may
progress to paralysis
Venous occlusion
Pain is more common with walking or other
activity and diminishes with rest
Described as a deep ache or throbbing type of
pain
Localized to the area around the occlusion
Described as an aching or throbbing
Pain which evolves
Swelling of the extremity with deep muscle
tenderness, darkened color and a possible fever
8|Page
Certified Emergency Nurse (CEN) Exam Review
Positioning
Activity
Treatment
TREATMENT CONSIDERATIONS
Arterial occlusion
Elevate HOB but do not elevated
extremity
Encourage activity
Thrombolytic infusion,
embolectomy , balloon catheter
extraction or bypass grafting
Education
Jeff Solheim
Venous occlusion
Elevate affected extremity
Absolute bedrest
Anticoagulants or thrombolytics
Warm packs over site
Increase fluids
Monitor for PE, stroke, MI
Blunt cardiac injury (right ventricle most often affected.)
o Clinical manifestations range from mild chest pain to cardiac failure
o Possible EKG changes
Tachycardia
PAC
PVC
Atrial fibrillation
SA or AV block
VF or VT
ST and T wave abnormalities
o Treatment
Cardiac monitor
IV access (fluid restriction to prevent heart failure)
Interventions for heart failure and dysrhythmias as appropriate
Admission
9|Page
Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
Practice Questions
Which of the following patients carries the highest risk of contracting endocarditis?
a.
b.
c.
d.
An 81-year old patient being treated for acute hypertension
A 39-year-old patient who had a large tattoo engraved two weeks previously
A 22-year old patient who has had two cases of conjunctivitis in the past three weeks
A 51-year old patient who had an inferior wall myocardial infarction four weeks previously
Which of the following assessment findings is more consistent with a peripheral vascular venous occlusion?
a.
b.
c.
d.
A burning discomfort in an extremity
A fever associated with a pale, cool extremity
Excruciating pain which is relieved with activity
An aching pain localized to one area of an extremity
A pediatric patient weighing 12 kg is to be cardioverted. What is the appropriate initial energy level?
a.)
b.)
c.)
d.)
3 Joules
12 Joules
36 Joules
50 Joules
A patient presents to the ED with a blood pressure of 234/144 mm Hg. If pharmacological treatment is undertaken for this disorder,
which of the following blood pressure readings would be optimal within 30 minutes of treatment initiation?
a.
b.
c.
d.
120/80 mm Hg
140/90 mm Hg
164/100 mm Hg
200/100 mm Hg
ANSWERS: B, D, B, C
10 | P a g e
Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
REFERENCES
American Heart Association. (2010, November). Adult Advanced Cardiovascular Life Support: 2010 American Heart Association
Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation , pp. S729 - S767.
Baird, M. S., Hicks-Keen, J., & Swearingen, P. L. (2005). Manual to critial care nursing: Nursing interventions and collaborative
management. St. Louis MO: Mosby.
Beall, B. D. (2005). Salicylate overdose. In E. L. Mitchell, & R. Medzon (Eds.), Introduction to Emergency Medicine (pp. 469 - 473).
Philadelphia, Pennsylvania: Lippincott, Williams and Wilkins.
Carter, J. S. (2004, November 2). Atoms, molecules, water and pH. Retrieved July 27, 2008, from File atom H2O:
http://biology.clc.uc.edu/courses/bio104/atom-h2o.htm
Center for disease control and prevention. (2008, February 22). Bacterial vaginosis. Retrieved September 29, 2008, from Center for
disease control and prevention: http://www.cdc.gov/STD/BV/STDFact-Bacterial-Vaginosis.htm#Treatment
Center for disease control and prevention. (2007). Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents
in Healthcare Settings 2007 . Retrieved April 15, 2008, from Center for disease control and prevention:
http://www.cdc.gov/ncidod/dhqp/gl_isolation.html
Center for Disease Control. (2007, September 21). Traumatic Brain Injury. Retrieved June 2, 2008, from National Center for injury
prevention and control: http://www.cdc.gov/ncipc/factsheets/tbi.htm
Corbett, J. V. (2004). Laboratory tests and diagnostic procedures (6 ed.). Upper Saddle River: Pearson Prentice Hall.
Danis, D., Blansfield, J., & Gervasini, A. (2007). Handbook of clinical trauma: the first hour (4 ed.). St. Louis: Mosby Elsevier.
Emergency Nurses Association. (2004). Emergency Nursing Pediatric Course Provider Manual (3 ed.). Des Plaines: Emergency
Nurses Association.
Emergency Nurses Association. (2007). Trauma Nursing Core Course Provider Manual (6 ed.). Des Plaines Il: Emergency Nurses
Association.
Ferrell, J. J. (2007). Forensic aspects of emergency nursing. In K. S. Hoyt, & J. Selfridge-Thomas (Eds.), Emergency Nursing Core
Curriculum (6 ed., pp. 1025 - 1032). Philiadelphia: Saunders - Elsevier.
Gray, R. O. (2009). Hypertension. In J. A. Marx, R. S. Hockberger, & R. M. Walls (Eds.), Rosen's Emergency Medicine (7 ed.). St.
Louis: Mosby-Elsevier.
Hebra, A. (2006, May 5). Intestinal volvulus. Retrieved July 28, 2008, from eMedicine: http://www.emedicine.com/ped/topic1205.htm
Hoek, T. L., Morrison, L. J., Shuster, M., Donnino, M., Sinz, E., Lavonas, E. J., et al. (2010). Part 12: Cardiac Arrest in Special
Situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care.
Circulation , S829 - S 861.
Honigman, B. K. (2005). Emergency Medicine (2 ed.). (mitchell, & e. L. Mitchell, Eds.) baltimore: Lippincott, Williams, Wilkins.
Hospital Incident Command System. (2008, July 28). Retrieved August 11, 2008, from Western Safety Products:
http://images.google.com/imgres?imgurl=http://www.westernsafety.com/HICSnew/hics_color2.jpg&imgrefurl=http://www.westernsafety.com/HICSnew/hics2006pg1.html&h=1315&w=720&sz=134&hl=en&start=1&um=1&tbnid=uZww2DkgFtensM:&tbnh=150&tbnw=82&prev=/
images%3Fq%3D
Hoyt, K. S., & Selfridge-Thomas, J. (Eds.). (2007). Emergency Nursing Core Curriculum (6 ed.). St. Louis: Saunders Elsevier.
International Critical Incident Stress Foundation Inc. (2004). Related articles and resources. Retrieved August 11, 2008, from
International Critical Incident Stress Foundation Inc.: http://www.icisf.org/articles/
11 | P a g e
Certified Emergency Nurse (CEN) Exam Review
Jeff Solheim
Kaplow, R., & Hardin, S. R. (2007). Critical Care Nursing. Boston: Jones and Bartlett Publishers.
Kleinman, M. E., Chameides, L, Schexnayder, S. M., Samson, R. A., Hazinski, M. F. Atkins, K. L.. et al.. (2010, November).
Pediatric Advanced Life support. Circulation 122 , pp. S876 - S908.
Kowalak, J. P., & Welsh, W. (Eds.). (2003). Handbook of diagnostic tests (3 ed.). Baltimore: Lippincott Williams and Wilkins.
Life Source. (2008). Organ and Tissue Donation Manual. St. Paul: Life Source.
Link, M. S., Atkins, D. L., Passman, R. S., Halperin, H. R., Samson, R. A., White, R. D., et al. (2010). 2010 American Heart
Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care: Part 6: Electrical Therapies.
Circulation , 122, S706 - S719.
Marino, P. L. (2007). ICU book (3 ed.). Philidelphia: Lippincott Williams and Wilkins.
Marx J. A., R. S. Hockberger, & R. M. Walls (Eds.) (2009), Rosen's Emergency Medicine (7 ed.). St. Louis: Mosby-Elsevier.
McCance, K. L., & Heuther, S. E. (2002). Pathophysiology: The biologic basis for disease in adults and children. St. Louis: Mosby.
Mitchell, E. L., & Medzon, R. (2005). Introduction to emergency medicine. Baltimore : Lippincott Williams and Wilkins.
National institutes of health. (2007, May 25). Preterm labor and birth. Retrieved October 2, 2008, from National Institute of child
health and human development: http://www.nichd.nih.gov/health/topics/Preterm_Labor_and_Birth.cfm
Neumar, R. W., Otto, C. W., Link, M. S., Kronick, S. L., Shuster, M., Callaway, C. W., et al. (2010). Part 8; Adult Advanced
Cardiovascular Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency
Cardiovascular Care. Circulation 122 , S729-767S.
Niemann, J. T., & Squire, B. (2009). Implantable Cardiac Devices. In J. A. Marx, R. S. Hockberger, & R. M. Walls (Eds.), Rosen's
Emergency Medicine (7 ed.). St. Louis: Mosby-Elsevier.
Newberry, L. (Ed.). (2003). Sheehy's Emergency Nursing (5 ed.). St. Louis: Mosby.
Newberry, L., & Criddle, L. (Eds.). (2005). Sheehy's manual of emergency care (6 ed.). St. Louis: Elsevier Mosby.
Niemann, J. T., & Squire, B. (2009). Implantable Cardiac Devices. In J. A. Marx, R. S. Hockberger, & R. M. Walls (Eds.), Rosen's
Emergency Medicine (7 ed.). St. Louis: Mosby-Elsevier.
O'Toole, M. T. (Ed.). (2003). Encyclopedia and dictionary of medicine, nursing and allied health (7 ed.). St. Louis: Saunders Elsevier.
Peitzman, A. B., Rhodes, M., Schwab, C. W., Yealy, D. M., & Fabian, T. C. (2007). The trauma manual: trauma and acute care
surgery. Philadelphia : Lippincott Williams and Wilkins.
Peberdy, M. A., Callaway, C. W., Neumar, R. W., Geocadin, R. G., Zimmerman, J. L., Donnino, M., et al. (2010). Post-Cardiac Arrest
Care. Circulation , 122, 768-786.
United Network for Organ Sharing. (2008, July 16). Membership. Retrieved July 16, 2008, from United Network for Organ Sharing:
http://www.unos.org/whoWeAre/membership.asp
United States Department of Health and Human Services. (2003, May). OCR Privacy Brief. Retrieved May 17, 2008, from Summary
of the HIPAA privacy rule: http://www.hhs.gov/ocr/privacysummary.pdf
Urden, L. D., Stacy, K. M., & Lough, M. E. (2002). Critical Care Nursing (4 ed.). St. Louis: Mosby.
ValueOptions New Jersey. (n.d.). What is HIPAA? Retrieved May 17, 2008, from ValueOptions New Jersey:
http://www.vonewjersey.com/VONJDocuments/WhatIsHIPAA.pdf
12 | P a g e