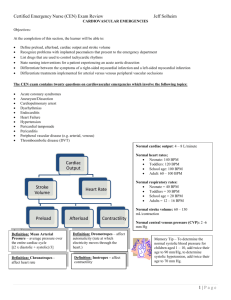
Certified Emergency Nurse (CEN) Exam Review Jeff Solheim CARDIOVASCULAR EMERGENCIES Objectives: At the completion of this section, the learner will be able to: Define preload, afterload, cardiac output and stroke volume Recognize problems with implanted pacemakers that present to the emergency department List drugs that are used to control tachycardic rhythms State nursing interventions for a patient experiencing an acute aortic dissection Differentiate between the symptoms of a right-sided myocardial infarction and a left-sided myocardial infarction Differentiate treatments implemented for arterial versus venous peripheral vascular occlusions The CEN exam contains twenty questions on cardiovascular emergencies which involve the following topics: Acute coronary syndromes Aneurysm/Dissection Cardiopulmonary arrest Dysrhythmias Endocarditis Heart Failure Hypertension Pericardial tamponade Pericarditis Peripheral vascular disease (e.g. arterial, venous) Thromboembolic disease (DVT) Normal cardiac output: 4 – 8 L/minute Normal heart rates; Neonate: 140 BPM Toddlers: 120 BPM School age: 100 BPM Adult: 60 – 100 BPM Cardiac Output Stroke Volume Heart Rate Normal respiratory rates: Neonate = 40 BPM Toddlers = 30 BPM School age = 20 BPM Adults = 12 – 16 BPM Normal stroke volume: 60 – 130 mL/contraction Preload Trauma Definition: Mean Arterial Pressure – average pressure over the entire cardiac cycle [(2 x diastolic + systolic)/3] Definition: Chronotropes affect heart rate Afterload Contractility Normal central venous pressure (CVP): 2 -6 mm Hg Definition: Dromotropes – affect automaticity (rate at which electricity moves through the heart.) Definition: Inotropes – affect contractility Memory Tip – To determine the normal systolic blood pressure for children aged 1 – 10, add twice their age to 90 mm/Hg, to determine systolic hypotension, add twice their age to 70 mm Hg. 1|Page Certified Emergency Nurse (CEN) Exam Review Jeff Solheim Cardiovascular pharmacology o Bradycardia Atropine (reverses cholinergic-mediated decreases in heart rate) Use with caution in cases of coronary ischemia and MI Unlikely to be effective after cardiac transplantation Not useful in Type II second-degree or third degree heart block Epinephrine (positive inotrope, dromotrope and chronotrope) Dopamine - Doses between 2 and 10 mcg/kg/minute effective to increase heart rate. Pacemaker therapy - pacemakers are used when the heart’s intrinsic pacemaking system is inadequate. Most effective for bradycardia, heart block and idioventricular rhythms. Two methods of pacing in ED: External (transcutaneous) –Large electrodes are placed on the skin, one on the back at the midthoracic level of the spine and a second on the front at the chest lead level of V 3. Transvenous – involves threading a catheter electrode into the right atrium or ventricle via the subclavian, internal jugular, brachial, or femoral vein. o Pacemaker settings Heart rate (how often the pacemaker fires) Pacemaker output (strength of pacemaker impulse) Sensitivity (degree which pacemaker senses intrinsic impulses) Implanted pacemaker: Problem solving o Failure to output Possible causes Battery failure Lead problem (lead fracture or fractured lead insulation) Oversensing Management: medications to increase intrinsic heart rate, temporary pacemaker. o Failure to capture Possible causes Failing battery Lead issue (lead fracture, dislodgement, fractured lead insulation) Exit block o Ischemia/infarction at endocardium site o Hyperkalemia o Class III antiarrhythmic drugs (e.g. amiodarone) Treatment: correct the problem, temporary pacing o Oversensing Causes Muscular activity Outside interference (MRI, electrocautery, digital cellular phone) Management – magnet application Tachycardia Cardioversion o If time allows: Assess potassium, magnesium and digoxin levels Remove dentures Allow patient to go to the bathroom Remove transdermal medication and patches Provide conscious sedation o Set to “sync”, assure sync is working 2|Page Certified Emergency Nurse (CEN) Exam Review Jeff Solheim o Do not give calcium channel blockers or beta-blockers to patients with bradycardia, heart blocks, heart failure, etc. Set energy level Narrow and regular QRS complexes: 50 to 100 Joules (J) Narrow but irregular QRS complexes: 120 to 200 J (biphasic waveform) or 200 J (monophasic waveform) Wide and regular QRS complexes: 100 J Wide but irregular QRS complexes: Patient will require defibrillation (nonsynchronized) Pediatric: 0.5 – 1 Joule/kg increased to 2 Joule/kg o Deliver shock after “all clear” Under breasts of large breasted woman Shave hairy chests Do not cardiovert over pacemaker or ICD o Increase energy if unsuccessful and repeat Internal cardiac defibrillator o Malfunctions Continuous unneeded firing: apply a magnet Firing during cardiac arrest Allow ICD to work Apply magnet if ICD continues to fire but does not convert the rhythm. Wait 30 seconds after final firing to manually defibrillate Keep paddles/patches 10 cm away from ICD. Narrow Complex o Vagal maneuvers o Adenosine Rapid IV push followed by 20 cc saline bolus May cause transient heart block or asystole o Calcium channel blockers (-depine) Vasodilators, negative inotrope, negative chronotrope, negative dromotrope. o Beta-blockers (-lol) Vasodilators, negative inotrope, negative chronotrope, negative dromotrope. Cardioselective beta-blockers – Beta-one blockers only (ideal for patients with pre-existing pulmonary conditions) E.g. – Propranolol, Nadolol, Timolol, Pindolol, Carteolol, Penbutolol Non-cardioselective beta-blockers - beta-one and beta two blocking. E.g. – Acebutolol, Atenolol, Metoprolol, Esmolol, Betaxolol, Bisoprolol Wide complex o Unstable: cardioversion and/or precordial thump (for witnessed arrest on a monitor in the absence of immediate defibrillation) o Stable Procainamide IV Monitor for: o Hypotension o Widening of the QRS complex more than 50% Amiodarone – may cause nausea, bradycardia, hypotension Sotalol 3|Page Certified Emergency Nurse (CEN) Exam Review o Drug Epinephrine (Adrenalin) Isoproterenol (Isuprel) Dopamine (Intropin, Dopastat) Norepinephrine bitartrate (Levophed) Phenylephrine (NeoSynephrine) o Nitroglycerin Diazoxide (Hyperstat) Notes Positive inotrope, dromotrope and chronotrope as well as vasoconstrictor alpha, beta-one and beta-two stimulation – can increase myocardial workload, can cause myocardial ischemia. alpha, beta-one and beta-two stimulation 2 – 10 mcg/kg/minute cardiac output > 10 mcg/kg/minute BP Peripheral venous and arterial vasoconstrictor and cardiac stimulant considered in the treatment of hypotension or shock. Pure alpha-agonist Vasodilators (monitor for hypotension) Drug Angiotensin Converter Enzymes (ACE Inhibitors). End in –pril Milrinone/Amrinone Sodium Nitroprusside (Nipride) Jeff Solheim Vasoconstrictors (monitor for hypertension. May cause local necrosis in cases of infiltration. Infiltration treated with phentolamine) Pharmacology preload and afterload through vasodilation and diuresis Vasodilator/positive inotrope Potent venous AND arterial dilator Venous dilator (arterial dilator in higher doses) Coronary artery dilator Arterial dilator for significant hypertension Notes Monitor for dry cough, hyperkalemia and angioedema Treatment for heart failure Protect from light (aluminum foil or opaque plastic) Give IV in glass bottles through PVC tubing. Inhibits release of insulin (can cause hyperglycemia) Hypertension o Severe elevations in blood pressure can lead to: Hypertensive encephalopathy (altered LOC, dizziness, headache, stroke seizures) Retinal hemorrhages with visual complaints Renal damage (hematuria, oliguria) Chest pain and ischemia Heart failure (enlarged heart, S3/S4 heart sounds) Epistaxis Acute Aortic Dissection (tear in the intimal layer of the aorta, which exposes the degenerated medial layer to the forces of blood pressure. These forces cleave or dissect the two layers of the arterial wall) o Ascending Dissection (A) Most common and lethal o Descending Dissection (B) C o Descending into Ascending (C) o Risk factors Hypertension Connective tissue disease (e.g. Marfan’s syndrome) Pregnancy Trauma A B 4|Page Certified Emergency Nurse (CEN) Exam Review o o Ascending dissection - pain in the substernal area, throat, jaw or face Descending dissection - pain in the intrascapular or lower back areas, abdomen, flank and lower extremities. Changes in blood pressure (Difference of more then 10 mm Hg when comparing SBP of various limbs). Symptoms of spinal cord hypoxia such paresthesia, hemiplegia and paraplegia. Signs of hypovolemia, hct, WBC ( BUN and creatinine if renal arteries affected) Treatment Prepare for rapid deterioration (oxygen, large bore IV) Blood products and fluid resuscitation as needed. Narcotics (pain) Anti-hypertensives Jeff Solheim Clinical manifestations Pain (may be described as a sudden onset tearing, ripping, sharp, knife-like pain not relieved by analgesics) Nitroprusside (Nipride) Labetalol (Normadyne, Trandate) Calcium channel blockers such as verapamil (Isoptin, Calan) or diltiazem (Cardizem) Surgical repair/ open thoracotomy Heart failure[Occurs when the heart can no longer produce sufficient cardiac output at normal filling pressures to meet metabolic demands (usually when the left ventricular ejection fraction falls below 40%)] o Clinical manifestations Right-sided failure Left-sided failure o Treatment: Peripheral edema Hemoptysis Vasodilators (morphine, Nitroprusside, Hepatomegaly Progressive dyspnea ACE inhibitors) JVD Crackles on auscultation Diuretics CVP Increased pulmonary artery pressures Positive inotropes (lanoxin, dobutamine) Dopamine to support blood pressure Coronary artery disease Symptom progression Event Stable angina Easily relieved by Pain rest/NTG EKG changes Cardiac Enzymes Transient ST depression Normal Unstable angina Lasts longer than 20 minutes Transient ST depression/ T wave inversion NSTEMI Continuous chest pain ST segment depression and T wave abnormalities STEMI Pain described as worse than angina ST segment elevation > 2 mm in leads V , V and V and > 1 mm in Normal Elevated Elevated 1 2 3 all other leads 5|Page Certified Emergency Nurse (CEN) Exam Review M O Medication Morphine Sulfate Dose 2 -4 mg IV push, repeat q5-30 minutes as needed Oxygen Nitroglycerin 4 L/min via nasal cannula S/L or spray q3-5 minutes up to 3 doses 12.5 – 25 mcg bolus IV followed by an infusion 1020 mcg/minute 160 – 325 mg PO (chewable) N Aspirin A Comments pain preload myocardial oxygen demand Titrate to keep oxygen saturation above 95% Limit SBP changes to <10% if normotensive or < 30% if hypertensive Hold if SBP < 90 mmHg Contraindicated for people who have taken Viagra or Levitra within 24 hours Maybe repeated in patients who have already taken ASA or are on daily doses Location of MI based on changes in various leads o • • • • • • • • Jeff Solheim Treatment considerations for a myocardial infarction Location of MI Anterior Expected lead changes V , V and V Anterior/Septal V,V Lateral I, AVL, V , V Inferior Right Ventricle II, III, AVF RV , RV , RV Posterior Tall R waves and ST depression in V and V 2 3 4 1 2 5 4 5 6 6 1 2 Thrombolytics Contraindications Recent internal bleeding (less than one month prior to arrival) Known bleeding diathesis History of cerebrovascular accident Recent surgery Intracranial arteriovenous malformations Uncontrolled hypertension (SBP > 180 mm Hg, DBP > 110 mm Hg) Trauma within the past ten days Recent cardiopulmonary resuscitation efforts • • • • • • • Relative Contraindications Minor trauma Diabetic retinopathy Pregnancy Concurrent anticoagulation Severe trauma in the past six months Any previous central nervous system event Unsuccessful central venous puncture Monitoring after thrombolytics Monitor for bleeding o Venipuncture/ABG puncture sites o GCS for intracranial bleeding o Abdominal girth o Bruising in the flanks Reduce risk for bleeding o Minimize movement o Limit venipunctures/ABGs o Minimize invasive blood pressures Monitor for reperfusion o Resolution of chest pain o Normalizing ST segment changes o Reperfusion arrhythmias 6|Page Certified Emergency Nurse (CEN) Exam Review Jeff Solheim Right Ventricular Infarct o Move leads to right side of chest V1R Fourth intercostal space along the left sternal border. (same as lead V 2) V2R Fourth intercostal space along the right sternal border. (Same as lead V 1) V3R Midway between leads V2R and V4R V4R (V7) Fifth intercostal space at the right midclavicular line V5R (V8) Midway between V4R and V6R in the fifth intercostal space V6R (V9) Right midaxillary line at the fifth intercostal space Symptom Right side Left side Nausea and vomiting Dyspnea/Orthopnea Diaphoresis Tachycardia Bradycardia Hypertension Hypotension JVD o Treatment Fluid loading Inotropic support Avoid vasodilators (morphine, nitroglycerin, diuretics) All other treatments as per MI protocols Variant angina (also known as variable angina, Prinzmetal’s angina or coronary artery spasms – caused by ischemia secondary to a spasm in the coronary artery.) o Often occurs in younger individuals who may have no coronary heart disease o Causes chest pain that is often more severe than typical angina pain. Pain tends to be cyclical Often occurs between midnight and 8 AM o EKG may show ST elevation that resolves with resolution of pain. o Treated with nitroglycerin or calcium channel blockers Infections involving the heart o Infective Endocarditis (general term used to describe inflammation of the endocardium, especially the cardiac valves) Clinical manifestations Signs of infection (Fever, anorexia, weight loss, night sweats, myalgia, fatigue, malaise) Pain (Pleuritic chest pain, abdominal or back pain Signs of Embolization (stroke signs, hemoptysis, splinter hemorrhages, petechiae of the conjunctiva, palate, neck, upper trunk, or extremities, Osler’s nodes, Janeway lesions) Diagnosis WBC ESR Blood cultures Echocardiogram Treatment Definition: Osler’s nodes – tender, subcutaneous nodules, often in the pulp of the digits. Long term IV antibiotics May require admission with cardiac monitoring Definition: Janeway Lesions – non-tender erythematous, hemorrhagic, or pustular lesions often on the palms or soles 7|Page Certified Emergency Nurse (CEN) Exam Review Jeff Solheim Pericarditis (inflammation of the pericardial sac) o Common causes MI (2 – 3 days after the MI) Connective tissue disorders Renal failure Mediastinal injury Neoplasms or radiation Infectious processes o Clinical manifestations Pain (exacerbated by deep inspiration, coughing, swallowing, supine position, but relieved by leaning forward or sitting up) Indications of infection (malaise, fever, chills, dyspnea and cough) Tachycardia and tachypnea Auscultation of pericardial friction rub EKG changes ST segment elevation with upright T waves in all leads except aVR and V 1. T waves flatten, the ST segment returns to baseline after several days T wave inversion (it may take weeks or months for the T waves to return to normal). o Treatment Allow patient position of comfort (sitting upright with legs dangling) Definition: Kussmaul’s Anti-inflammatory agents Sign - Elevation of neck veins with inspiration Antipyretics during spontaneous Antibiotics breathing Colchicine (for cases related to gout) Pericardial tamponade (accumulation of fluid in the pericardial sac) o Clinical manifestations Beck’s triad (muffled heart tones, hypotension, JVD) Kussmaul’s sign Obstructive shock (narrowing pulse pressure, cool, moist skin, urinary output) o Treatment Pericardiocentesis (Emergent cases) Surgery Peripheral vascular occlusions Provacation of pain Quality of pain Region and radiation of pain Severity of pain Timing of pain Objective findings SYMPTOMS Arterial occlusion Pain is always present, it occurs at rest, with movement and with exercise May be described as a burning discomfort Typically hurts from the area of the occlusion distally because all tissue distal to the occlusion will be void of adequate oxygen Described as excrutiating Pain starts as soon as the occlusion develops and is not easily relieved Cold extremity with decreases pulses that may progress to paralysis Venous occlusion Pain is more common with walking or other activity and diminishes with rest Described as a deep ache or throbbing type of pain Localized to the area around the occlusion Described as an aching or throbbing Pain which evolves Swelling of the extremity with deep muscle tenderness, darkened color and a possible fever 8|Page Certified Emergency Nurse (CEN) Exam Review Positioning Activity Treatment TREATMENT CONSIDERATIONS Arterial occlusion Elevate HOB but do not elevated extremity Encourage activity Thrombolytic infusion, embolectomy , balloon catheter extraction or bypass grafting Education Jeff Solheim Venous occlusion Elevate affected extremity Absolute bedrest Anticoagulants or thrombolytics Warm packs over site Increase fluids Monitor for PE, stroke, MI Blunt cardiac injury (right ventricle most often affected.) o Clinical manifestations range from mild chest pain to cardiac failure o Possible EKG changes Tachycardia PAC PVC Atrial fibrillation SA or AV block VF or VT ST and T wave abnormalities o Treatment Cardiac monitor IV access (fluid restriction to prevent heart failure) Interventions for heart failure and dysrhythmias as appropriate Admission 9|Page Certified Emergency Nurse (CEN) Exam Review Jeff Solheim Practice Questions Which of the following patients carries the highest risk of contracting endocarditis? a. b. c. d. An 81-year old patient being treated for acute hypertension A 39-year-old patient who had a large tattoo engraved two weeks previously A 22-year old patient who has had two cases of conjunctivitis in the past three weeks A 51-year old patient who had an inferior wall myocardial infarction four weeks previously Which of the following assessment findings is more consistent with a peripheral vascular venous occlusion? a. b. c. d. A burning discomfort in an extremity A fever associated with a pale, cool extremity Excruciating pain which is relieved with activity An aching pain localized to one area of an extremity A pediatric patient weighing 12 kg is to be cardioverted. What is the appropriate initial energy level? a.) b.) c.) d.) 3 Joules 12 Joules 36 Joules 50 Joules A patient presents to the ED with a blood pressure of 234/144 mm Hg. If pharmacological treatment is undertaken for this disorder, which of the following blood pressure readings would be optimal within 30 minutes of treatment initiation? a. b. c. d. 120/80 mm Hg 140/90 mm Hg 164/100 mm Hg 200/100 mm Hg ANSWERS: B, D, B, C 10 | P a g e Certified Emergency Nurse (CEN) Exam Review Jeff Solheim REFERENCES American Heart Association. (2010, November). Adult Advanced Cardiovascular Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation , pp. S729 - S767. Baird, M. S., Hicks-Keen, J., & Swearingen, P. L. (2005). Manual to critial care nursing: Nursing interventions and collaborative management. St. Louis MO: Mosby. Beall, B. D. (2005). Salicylate overdose. In E. L. Mitchell, & R. Medzon (Eds.), Introduction to Emergency Medicine (pp. 469 - 473). Philadelphia, Pennsylvania: Lippincott, Williams and Wilkins. Carter, J. S. (2004, November 2). Atoms, molecules, water and pH. Retrieved July 27, 2008, from File atom H2O: http://biology.clc.uc.edu/courses/bio104/atom-h2o.htm Center for disease control and prevention. (2008, February 22). Bacterial vaginosis. Retrieved September 29, 2008, from Center for disease control and prevention: http://www.cdc.gov/STD/BV/STDFact-Bacterial-Vaginosis.htm#Treatment Center for disease control and prevention. (2007). Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings 2007 . Retrieved April 15, 2008, from Center for disease control and prevention: http://www.cdc.gov/ncidod/dhqp/gl_isolation.html Center for Disease Control. (2007, September 21). Traumatic Brain Injury. Retrieved June 2, 2008, from National Center for injury prevention and control: http://www.cdc.gov/ncipc/factsheets/tbi.htm Corbett, J. V. (2004). Laboratory tests and diagnostic procedures (6 ed.). Upper Saddle River: Pearson Prentice Hall. Danis, D., Blansfield, J., & Gervasini, A. (2007). Handbook of clinical trauma: the first hour (4 ed.). St. Louis: Mosby Elsevier. Emergency Nurses Association. (2004). Emergency Nursing Pediatric Course Provider Manual (3 ed.). Des Plaines: Emergency Nurses Association. Emergency Nurses Association. (2007). Trauma Nursing Core Course Provider Manual (6 ed.). Des Plaines Il: Emergency Nurses Association. Ferrell, J. J. (2007). Forensic aspects of emergency nursing. In K. S. Hoyt, & J. Selfridge-Thomas (Eds.), Emergency Nursing Core Curriculum (6 ed., pp. 1025 - 1032). Philiadelphia: Saunders - Elsevier. Gray, R. O. (2009). Hypertension. In J. A. Marx, R. S. Hockberger, & R. M. Walls (Eds.), Rosen's Emergency Medicine (7 ed.). St. Louis: Mosby-Elsevier. Hebra, A. (2006, May 5). Intestinal volvulus. Retrieved July 28, 2008, from eMedicine: http://www.emedicine.com/ped/topic1205.htm Hoek, T. L., Morrison, L. J., Shuster, M., Donnino, M., Sinz, E., Lavonas, E. J., et al. (2010). Part 12: Cardiac Arrest in Special Situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation , S829 - S 861. Honigman, B. K. (2005). Emergency Medicine (2 ed.). (mitchell, & e. L. Mitchell, Eds.) baltimore: Lippincott, Williams, Wilkins. Hospital Incident Command System. (2008, July 28). Retrieved August 11, 2008, from Western Safety Products: http://images.google.com/imgres?imgurl=http://www.westernsafety.com/HICSnew/hics_color2.jpg&imgrefurl=http://www.westernsafety.com/HICSnew/hics2006pg1.html&h=1315&w=720&sz=134&hl=en&start=1&um=1&tbnid=uZww2DkgFtensM:&tbnh=150&tbnw=82&prev=/ images%3Fq%3D Hoyt, K. S., & Selfridge-Thomas, J. (Eds.). (2007). Emergency Nursing Core Curriculum (6 ed.). St. Louis: Saunders Elsevier. International Critical Incident Stress Foundation Inc. (2004). Related articles and resources. Retrieved August 11, 2008, from International Critical Incident Stress Foundation Inc.: http://www.icisf.org/articles/ 11 | P a g e Certified Emergency Nurse (CEN) Exam Review Jeff Solheim Kaplow, R., & Hardin, S. R. (2007). Critical Care Nursing. Boston: Jones and Bartlett Publishers. Kleinman, M. E., Chameides, L, Schexnayder, S. M., Samson, R. A., Hazinski, M. F. Atkins, K. L.. et al.. (2010, November). Pediatric Advanced Life support. Circulation 122 , pp. S876 - S908. Kowalak, J. P., & Welsh, W. (Eds.). (2003). Handbook of diagnostic tests (3 ed.). Baltimore: Lippincott Williams and Wilkins. Life Source. (2008). Organ and Tissue Donation Manual. St. Paul: Life Source. Link, M. S., Atkins, D. L., Passman, R. S., Halperin, H. R., Samson, R. A., White, R. D., et al. (2010). 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care: Part 6: Electrical Therapies. Circulation , 122, S706 - S719. Marino, P. L. (2007). ICU book (3 ed.). Philidelphia: Lippincott Williams and Wilkins. Marx J. A., R. S. Hockberger, & R. M. Walls (Eds.) (2009), Rosen's Emergency Medicine (7 ed.). St. Louis: Mosby-Elsevier. McCance, K. L., & Heuther, S. E. (2002). Pathophysiology: The biologic basis for disease in adults and children. St. Louis: Mosby. Mitchell, E. L., & Medzon, R. (2005). Introduction to emergency medicine. Baltimore : Lippincott Williams and Wilkins. National institutes of health. (2007, May 25). Preterm labor and birth. Retrieved October 2, 2008, from National Institute of child health and human development: http://www.nichd.nih.gov/health/topics/Preterm_Labor_and_Birth.cfm Neumar, R. W., Otto, C. W., Link, M. S., Kronick, S. L., Shuster, M., Callaway, C. W., et al. (2010). Part 8; Adult Advanced Cardiovascular Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 122 , S729-767S. Niemann, J. T., & Squire, B. (2009). Implantable Cardiac Devices. In J. A. Marx, R. S. Hockberger, & R. M. Walls (Eds.), Rosen's Emergency Medicine (7 ed.). St. Louis: Mosby-Elsevier. Newberry, L. (Ed.). (2003). Sheehy's Emergency Nursing (5 ed.). St. Louis: Mosby. Newberry, L., & Criddle, L. (Eds.). (2005). Sheehy's manual of emergency care (6 ed.). St. Louis: Elsevier Mosby. Niemann, J. T., & Squire, B. (2009). Implantable Cardiac Devices. In J. A. Marx, R. S. Hockberger, & R. M. Walls (Eds.), Rosen's Emergency Medicine (7 ed.). St. Louis: Mosby-Elsevier. O'Toole, M. T. (Ed.). (2003). Encyclopedia and dictionary of medicine, nursing and allied health (7 ed.). St. Louis: Saunders Elsevier. Peitzman, A. B., Rhodes, M., Schwab, C. W., Yealy, D. M., & Fabian, T. C. (2007). The trauma manual: trauma and acute care surgery. Philadelphia : Lippincott Williams and Wilkins. Peberdy, M. A., Callaway, C. W., Neumar, R. W., Geocadin, R. G., Zimmerman, J. L., Donnino, M., et al. (2010). Post-Cardiac Arrest Care. Circulation , 122, 768-786. United Network for Organ Sharing. (2008, July 16). Membership. Retrieved July 16, 2008, from United Network for Organ Sharing: http://www.unos.org/whoWeAre/membership.asp United States Department of Health and Human Services. (2003, May). OCR Privacy Brief. Retrieved May 17, 2008, from Summary of the HIPAA privacy rule: http://www.hhs.gov/ocr/privacysummary.pdf Urden, L. D., Stacy, K. M., & Lough, M. E. (2002). Critical Care Nursing (4 ed.). St. Louis: Mosby. ValueOptions New Jersey. (n.d.). What is HIPAA? Retrieved May 17, 2008, from ValueOptions New Jersey: http://www.vonewjersey.com/VONJDocuments/WhatIsHIPAA.pdf 12 | P a g e