Example
advertisement

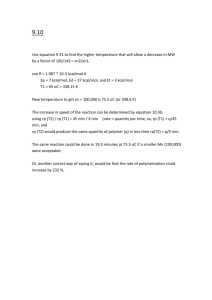
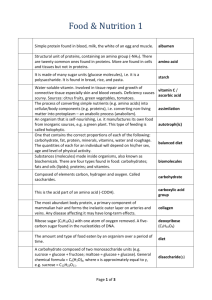
Debunking Myths and Updating Your Exercise Science NASM Educational Workshop Developed by: Fabio Comana, MA., MS..NASM CPT, CES & PES; NSCA CSCS; ACSM EP-C; ACE CPT & HC; CISSN. Faculty Instructor – NASM, SDSU and UCSD. Workshop Objectives: 1. 2. 3. 4. 5. Describe new updates to the USDA Dietary Guidelines. Discuss emerging research in sugar and disease. Explain new discoveries associated with fat intake. Summarize key principles and applications of the energy pathways. Distinguish true HIIT programming from more appropriate programming solutions for clients. 6. Develop and deliver alternatives to traditional HIIT workouts. 7. Demonstrate proper mechanics and technique to many popular exercises. 8. Describe the relationship of stability and mobility throughout the kinetic chain. 9. Administer and interpret observations from NASM’ overhead squat movement screen. 10. Design and implement a systematic corrective exercise program that delivers client solutions. Workshop Curriculum: Time Material Covered 0:00 – 0:10 Introduction 0:10 – 0:35 USDA Dietary Guidelines Updates 0:35 – 1:15 Sugar and Disease. 1:15 – 1:50 Emerging Research in Fat 1:50 – 2:25 Energy Pathways – Overview 2:25 – 3:05 HIIT Solutions 3:05 – 3:35 Lunch 3:35 – 4:25 Upper and Lower Extremity Movement Mechanics 4:25 – 5:05 Stability-Mobility: NASM overhead squat movement screen 5:05 – 5:50 Corrective Exercise 5:50 – 6:00 Closing Remarks 2015 – 2020 USDA Dietary Guidelines Updates USDA Guidelines Updates USDA Guidelines Update… Release January 11, 2016 1. 2. 3. 4. 5. Follow a healthy eating pattern across lifespan – all food and beverage choices matter. Choose a healthy eating pattern with appropriate kcal level to help achieve/maintain healthy body weight, support nutrient adequacy, and reduce risk of chronic disease. Focus on variety, nutrient density, and amount – to meet nutrient needs within kcal limits, select a variety of nutrient-dense foods across/within all food groups in recommended amounts. Limit kcal from added sugars and saturated fats, and reduce sodium intake. Reduce quantity of foods-beverages higher in these components to levels that fit within healthy eating patterns. Shift to healthier food-beverage choices – select nutrient-dense foodsbeverages across/within all groups v. less healthy choices, but cultural and personal preferences to make shifts easier to accomplish and maintain. Support healthy eating patterns for all. Everyone plays a role in helping create/support healthy eating patterns in multiple settings nationwide – from home to school, to work, and to communities. USDA Guidelines Update… In more detail: A healthy eating pattern includes: • • • • • • Variety of vegetables from all of the subgroups—dark green, red and orange, legumes (beans and peas), starchy, and other. Fruits, especially whole fruits. Grains, at least half of which are whole grains. Fat-free or low-fat dairy, including milk, yogurt, cheese, and/or fortified soy beverages. Variety of protein foods, including seafood, lean meats and poultry, eggs, legumes (beans and peas), and nuts, seeds, and soy products. Healthy oils. A healthy eating pattern limits saturated fats, trans fats, added sugars, and sodium: • • • • Consume < 10% of calories per day from added sugars (new) – v. 10% for all sugars. Consume < 10% of calories per day from saturated fats (same). Consume < 2,300 milligrams (mg) / day of sodium (same). If alcohol is consumed – consume in moderation (≤1 drink/day – women and ≤ 2 drinks/day – men) (same). USDA Guidelines Update… Food Group Amount* Vegetables 2½ cup eq./day • Dark green 1½ cup eq./week • Red and orange 5½ cup eq./week • Legumes (beans, peas) 1½ cup eq./week • Starchy 5 cup eq./week • Other 4 cup eq./week Fruits 2 cup eq./day Grains 6 oz. eq./day • Whole grains ≥ 3 oz. eq./day • Refined grains ≤ 3 oz. eq./day Dairy 3 cup eq./day Protein Foods 5½ oz. eq./day • Seafood 8 oz. eq./week • Meats, poultry, eggs 26 oz. eq./week • Nuts, seeds, soy products 4 oz. eq./week Oils 27 g/day Discretionary kcal (% total) 270 kcal/day (14%) Food Group Serving Size Vegetables • • ½ cup chopped = ½ cup equivalent. 1 cup raw (leafy) = ½ cup equivalent (new). Fruits • • • ½ cup fresh/frozen fruit = ½ cup equivalent. ½ cup juice = ½ cup equivalent. ¼ cup dried fruit = ½ cup equivalent. Grains • • • 1 oz. (~ 1 slice) grains = 1 oz. equivalent. ½ cup cooked grains = 1 oz. equivalent. 1 cup unsweetened cereal (¾ cup sweetened) = 1 oz. equivalent. Dairy • • • 8 oz. dairy = 1 cup equivalent. 8 oz. fat-free yogurt = 1 cup equivalent. 1½ oz. cheese = 1 cup equivalent. Proteins • • • • • 1 large egg = 1 oz. equivalent. 1 TBL peanut butter = 1 oz. equivalent. 1 oz. nuts/seeds = 2 oz. equivalent (new). ½ cup beans = 2 oz. equivalent (new). 1 oz. meat = 1 oz. equivalent. USDA Guidelines Update… Current Dietary Intakes v. Recommended • Approx. ¾ population follows diet low in vegetables, fruits, dairy, and oils. • Over ½ population meets or exceeding total grain and total protein foods recommendations. • Most Americans exceed recommendations for added sugars, saturated fats, and sodium USDA Guidelines Update… Nutrient Ref Kcal Child 1-3 Female 4-8 Male 4-8 Female 9-13 Male 9-13 Female 14-18 Male 14-18 Female 19-30 Male 19-30 Female 31-50 Male 31-50 Female 51+ Male 51+ 1,000 1,200 1,400 1,600 1,600 1,800 1,800 2,200, 2,800, 3,200 2,000 2,400, 2,600, 3,000 1,800 2,200 1,600 2,000 Protein (g) RDA 13 19 19 34 34 46 52 46 56 46 56 46 56 Protein (% kcal) AMDR 5-20 10-30 10-30 10-30 10-30 10-30 10-30 10-35 10-35 10-35 10-35 10-35 10-35 CHO (g) RDA 130 130 130 130 130 130 130 130 130 130 130 130 130 CHO (% kcal) AMDR 45-65 45-65 45-65 45-65 45-65 45-65 45-65 45-65 45-65 45-65 45-65 45-65 45-65 Fiber (g) 14g/1,000 kcal 14 16.8 19.6 22.4 25.2 25.2 30.8 28 33.6 25.2 30.8 22.4 28 Added sugars (% kcal) DGA <10% <10% <10% <10% <10% <10% <10% <10% <10% <10% <10% <10% <10% Total fat (% kcal) AMDR 30-40 25-35 25-35 25-35 25-35 25-35 25-35 20-35 20-35 20-35 20-35 20-35 20-35 Sat fat (% kcal) DGA <10% <10% <10% <10% <10% <10% <10% <10% <10% <10% <10% <10% <10% Linoleic acid (O-6) AI (g) 7 10 10 10 12 11 16 12 17 12 17 11 14 Linolenic acid ALA) AI (g) 0.7 0.9 0.9 1 1.2 1.1 1.6 1.1 1.6 1.1 1.6 1.1 1.6 Sugar and Disease Sugars Research Sugars … Simple Sugars = monosaccharides and disaccharides. • • 3 nutritionally important monosaccharides: Same chemical structure (C6H12O6). Classification Description # Units Sources Monosaccharides Smallest CHO unit. Only absorbable forms 1 unit Glucose, Fructose, Galactose ONLY glucose = Insulin response Nutrient Galactose Glucose Fructose Mechanism Glucose Active absorption = faster uptake rates. Galactose • Glucose = fuel + storage form in body • Galactose = structural compound at cell membrane / liver conversion to glucose or fat. Fructose Facilitated absorption = slower uptake rate. • Can cause GI distress. • Fructose = liver conversion to glucose or fat. Sugars … Classification Description # Units Sources 2 units • Sucrose = 1 glucose + 1 fructose, • Lactose = 1 glucose + 1 galactose • Maltose = 2 glucose Most Sweeteners Disaccharides Lactose Intolerant Simple Sugars Maltose Lactose Galactose + Glucose Glucose + Glucose Sucrose Glucose + Fructose Brown sugar Sucrose or Sugar Corn syrup Molasses High fructose corn syrup (HFCS) Maple sugar Caramel Brown rice syrup Fructose Glucose Lactose Date sugar Molasses powder Maple syrup Fruit sugar Dextrose Honey Dextrin Sugars … Sugars v. High Fructose Corn Syrup (1960s). • • Group of corn starches (glucose polymers) undergoing enzymatic processing – increases fructose content, then mixed with pure corn syrup (~ 100% glucose). Common HFCS form = HFCS 55 (55% fructose) – most commonly used. Comparable sweetness to sucrose; cheaper alternative. Does HFCS contribute to obesity? • Same rate as natural sugars (caloric density: 1 g = 4 kcal). • Coincidental entry to market with start of obesity epidemic (1970s). Does HFCS contribute to diabetes? • Perhaps little more than sugar given new research on fructose and obesity (leptin resistance), and diabetes. Does HFCS cause any other health concerns? • Yes, elevated levels of reactive carbonyls – 10x higher in HFCS (elevated in diabetics). • Believed to accelerate tissue damage (vascular, nerve). Sugars … Current Intakes … Men Women Current Guidelines* Total CHO Intake 48.0 % of total kcal 51.0 % of total kcal 45 – 65% of total kcal Sugar Intake 24.2 % of total kcal (13% added sugar) 25.3 % of total kcal (13% added sugar) ≤ 10 % of added sugar • Total sugar consumption = 130 lbs. each year (adults) (45 lbs. of sucrose). o 39 % increase since 1950. o Average adult = 22 tsp per day (children = 23 tsp per day). o Equivalent to 848 cans of 12 oz. (355 mL) soda / year. • HFCS consumption = 35 lbs. each year (adults). * 2014 – World Health Organization (WHO) recommendation for total sugar intake = aim for ≤ 5 % of total kcal • New USDA Guidelines: 10% added sugar = 12 tsp per day. Sugars … Current Intakes … American Heart Association (AHA) Center for Science in the Public Interest (CSPI) Women 6 tsp. added sugar 100 kcal (6½ tsp.) added sugar Men 9 tsp. added sugar 150 kcal (9½ tsp.) added sugar Added Sugars to US Diet Mixed Dishes Diary Grains 4% 2% Spreads, Dressings, Condiments, etc. 6% Beverages (not milk or juice) 8% 47% 31% Snacks and Sweets Vegetables 1% Fruit and Fruit Juice 1% Diabetes and Inflammation … Two types – affects 29.1 million adults (9.3% of population). • • • • Type I: 5 – 10% of diabetics (no insulin production). Type II: 90 – 95% of diabetics (adequate insulin – receptor resistance). Almost ½ US adults have Diabetes / Pre-diabetes (86 million – up from 79m). Cost = $245 billion (2012). Study: 75,000 nurses and 39,000 health professionals (22 years) • Sugary drink ≥ 1 per day = 30% increased for diabetes risk v. ≤ 1 per month. • Fruit juice ≥ 1 per day = 21% increased for diabetes risk v. ≤ 1 per week. Diabetes and Inflammation … Blood sugar fluctuates constantly throughout day. • Glycohemoglobin (HbA1c) – glycated hemoglobin (sugar bound to Hgb in red blood cells) represents chronic blood glucose levels (previous 8 weeks). • HbA1c associated with CVD, kidney disease (nephropathy), and retinal eye damage (retinopathy) – inflammation of walls and vessels. Blood glucose: Glycohemoglobin (HbA1c): ≥ 126 mg / dL ------------------------------------------< 126 mg / dL ≥ 6.5% ------------------------------------------< 6.5 % ≥ 100 mg / dL -----------------------------------------< 100 mg / dL ≥ 5.7 % -----------------------------------------< 5.7 % Diabetes and Inflammation … Inflammation – natural response to trauma and/or infection. • Chronic inflammation overwhelms physiological systems = functional impairment. Sugar Elevated blood sugar Release of cytokine interleukin-6 (IL-6) C-Reactive Protein release Attaches to collagen (protein) = glycosylation = inflammation Activates immune response Increases risk of heart attack (4½x) Harvard School of Public Health (ongoing) Nurse’s Health Study (n= 75,000) • 761 had either been diagnosed with or died from heart disease 1984 – 1994 • Strong correlation between highglycemic carbohydrate diet and CVD. • High-carbohydrate diets (especially high sugar = 2x increase in heart attack risk v. moderate-carbohydrate diets) Fructose and Disease … Fructose in Body Liver – Conversion to Glucose Excess = Fat Minimal use as Fuel Released as Triglycerides (deposition) Stored in Liver Fructose Research: • With equal intakes as glucose (25% of daily kcal) = more abdominal (visceral) and liver fat with fructose o Glucose = more subcutaneous fat. o Fructose = elevated dyslipidemia (Triglycerides – TG increased 10%; elevated LDLs). • Increased liver fat = Non-alcoholic Fatty Liver Disease (NAFLD) – cirrhosis. o Insulin passes from pancreas via liver into circulation. NAFLD = liver insulin resistance – liver fails to recognize insulin = increased insulin = diabetes. Fructose and Disease … Fructose Research (cont.): • Increased leptin (hormone suppressing appetite) resistance in brain (less passes into brain). o Also due to increased TG levels. o Equals increased caloric intake and obesity. • Dementia. o Elevated insulin levels shrink # insulin receptors in blood-brain-barrier. o Less insulin effect = less glucose enters brain = elevated cortisol (damages hippocampus). o Insulin can help clear beta-amyloids (peptide plaques – associated with Alzheimer’s) – less insulin effect = less clearance. • Increased levels of uric acid in joints (gout): o Less hepatic (liver) ATP production = more uric acid. Fructose and Disease … Food Fructose (to total sugar) Glucose (of total sugar) Glucose (dextrose) 0.0 % 100.0 % Plum 39.4 % 60.6 % Apricot 42.0 % 58.0 % Peach 46.4 % 53.6 % Maple Syrup 48.5 % 51.5 % Brown Sugar 49.5 % 51.5 % White Sugar (Cane sugar) 50.0 % 50.0 % Honey 50.5 % 44.5 % Orange / Orange Juice Concentrate 51.0 % 49.0 % Strawberry 51.8 % 48.2 % Banana 50.0 % 50.0 % Pineapple 51.0 % 49.0 % Grape / Grape Juice Concentrate 52 – 53 % 48.0 % Mango 53.4 % 46.6 % Papaya 61.0 % 39.0 % Apple / Apple Juice Concentrate 66.5 % 33.5 % Pear 67.3 % 32.6 % Agave 56 – 92 % 8 – 44 % Sugar v. Sweetener… Which do you choose? • Safest sweeteners: o Sugar alcohols – erythritol. o Stevia leaf extract (minus acesulfame-K). o Neotame. • Moderately Safe: o Sugar alcohols (xylitol, maltitol, sorbitol). o Sucralose. • Avoid: o Aspartame. o Saccharin. Your Turn … Think-Pair-Share – Quick Quizlets. • Question 1: Describe one structural and one functional difference between glucose and fructose. • Question 2: Define current nutritional guidelines for sugar. • Question 3: Identify possible mental health concerns associated with fructose. • Question 4: Briefly describe how fructose can lead to an increased risk developing diabetes. Emerging Research in Fats Fats Research Fats … Omega 3/6 Polyunsaturated Fats Biologically-active compounds (eicosanoids) derived from PUFAs (larger fatty acids: 18 – 22 carbon length). • Omega-3 and Omega-6 fatty acids = essential fatty acids. • • • • • • • Healthier Eicosanoids (Omega-3) Unhealthier Eicosanoids (Omega-6) Eicosapentaenoic Acid (EPA) – n-3; 20:5 Docosahexaenoic Acid (DHA) – n-3, 22-6 Alpha-linolenic Acid (ALA) – n-3, 18:3 Gamma-linolenic Acid (GLA) – n-6, 18:3 Linoleic Acid (LA) – n-6; 18:2 Arachidonic Acid (ADA) – n-6; 20:4 Gamma-linoleic acid – n-6; 18:2 Omega-3 FA Omega-6 FA Blood vessel / airway dilation. Reduced blood clotting (blood thinning). Improved blood lipid profiles. Reduced coronary vessel inflammation. Reduced levels of inflammatory agents in circulation (e.g., cytokines). Improved cell wall permeability. Gradual slowing of cellular aging. • • • • Many of the opposite. Cell growth (brain, muscles) – ADA (animal and dairy fats). Inflammatory markers (PGE1) to trigger acute immune response. Nervous system functioning – myelin sheaths. Fats … DHA Diet (e.g. flaxseed) Diet (e.g. Corn) ALA LA EPA ADA • LA required for production of inflammatory markers (e.g., PGE1 messenger) – triggers acute immune responses. • LA also converts to ADA. o Large quantities of ADA = PGE2 messengers (chronic pain / inflammation). • EPA (omega-3) manufactures PGE3 messengers – turn off inflammatory process. LA Gamma-linolenic acid (GLA) Delta-6-desaturase (enzyme). ALA EPA Relatively useless Omega-3 FA. • Excessive LA conversion to GLA reduces ALA conversion. • Conversion rates (at best) = 8 – 20%, but western diets (high omega-6s) = 1 – 5%. Fats … • Omega-3 Sources Omega-6 Sources EPA & DHA Fish oils (salmon, mackerel, trout, krill, anchovies) Corn, peanuts, safflower, sunflower, grains. ALA Vegetable sources (e.g., flaxseed, chia, canola oil) Ideal Ratios: 1-to-1 to 3-to-1 ratios between O-6 and O-3. ALA MUST be converted to EPA/DHA: o Conversion rates (at best) = 8 – 20%, but western diets (high omega-6s) = 1 – 5%. Sources of DHA/EPA Mg / 3 oz. Sources of ALA Mg / Tablespoon Cod 134 mg Pumpkin 51 mg Catfish 151 mg Olive Oil 103 mg Haddock 203 mg Walnuts (Black) 156 mg Clams 214 mg Soy 1,230 mg Flounder 426 mg Rapeseed (Canola) 1,300 mg Pollock 460 mg Flaxseed 2,350 mg Flatfish 498 mg Walnuts (English) 2,575 mg Tuna (canned) 733 mg Chia Seed 3,000 mg Salmon 1,825 mg Flaxseed Oil 7,250 mg Fats … 1 Tablespoon: Low O-6: ALA ratio High in MUFAs Dietary Fat Saturated Fatty Acid (SFA) Monounsaturated Fatty Acid (MUFA) Linoleic Acid (omega-6) - PUFA Almond Oil Avocado Canola (Rapeseed) Chia Seed Coconut Oil Cocoa Butter Corn Oil Cottonseed Oil Flaxseed Oil Grape Seed Oil Hemp Oil Margarine – Reg. Olive Oil Palm Oil Palm Kernel Oil Peanut Oil 8.1 % 19.8 % 7.0 % 10.3 % 86.7 % 59.6 % 13.0 % 25.7 % 9.3 % 12.5 % 9.5 % 17.5 % 14.0 % 49.6 % 81.6 % 17.7 % 69.9 % 70.0 % 62.0 % 9.4 % 5.9 % 33.1 % 27.5 % 17.9 % 17.9 % 17.4 % 12 % 49.0 % 72.8 % 37.0 % 5.9 % 45.9 % 17.7 % 10.2 % 19.2 % 18.8 % 1.5 % 2.9 % 52.9 % 51.6 % 15.7 % 68.5 % 55.0 % 31.5 % 9.6 % 8.9 % 1.5 % 31.8 % High in O-6 Alpha Linolenic Acid (omega-3) PUFA < 1.0 % < 1.0 % 9.2 % 57.1 % < 1.0 % < 1.0 % 1.4 % < 1.0 % 57.1 % < 1.0 % 22.5 % 2.0 % < 1.0 % < 1.0 % < 1.0 % < 1.0 % Fats … 1 Tablespoon: Low O-6: ALA ratio High in MUFAs High in O-6 Dietary Fat Saturated Fatty Acid (SFA) Monounsaturated Fatty Acid (MUFA) Linoleic Acid (omega-6) - PUFA Pumpkin Oil Rice Bran Safflower Oil Sesame Oil Soybean Oil Sunflower Oil Vegetable Shortening Walnut Oil Wheat Germ Oil 9.0 % 17.4 % 7.4 % 14.0 % 15.5 % 12.0 % 28.0 % 32.5 % 48.5 % 75 % 40.0 % 22.9 % 83.6 % 44.4 % 52.5 % 35.0 % 12.6 % 41.5 % 50.7 % 3.6 % 24.3 % Alpha Linolenic Acid (omega-3) PUFA 5.5 % < 1.0 % < 1.0 % < 1.0 % 6.6 % 2.9 % 2.0 % 8.8% 18.1 % 22.8 % 25.5 % 52.9 % 50.9 % 10.3 % 5.0 % Beef Fat Chicken Fat Butter Lard (pork fat) 49.6 % 29.9 % 64.6 % 39.1 % 41.9 % 44.9 % 26.5 % 45.3 % 3.1 % 19.7 % 3.5 % 10.2 % < 1.0 % < 1.0 % < 1.0 % < 1.0 % Fats … Optimal Total Cholesterol LDL HDL Triglycerides < 200 < 100 ≥ 40 (≥ 60 ideal) < 150 100 – 129 Near Optimal Borderline High High Very High Ratios: 200 – 239 130 – 159 150 – 199 ≥ 240 160 – 189 200 – 499 ≥ 190 ≥ 500 Total Cholesterol : HDL = < 5.5 -to-1 LDL : HDL = < 2.7 -to-1 • When assessing risk – avoid examining just total cholesterol score: Total Cholesterol (TC) = HDL + LDL + (TG ÷ 5). Example: • HDL = 65 mg/dL; LDL = 125 mg/dL; TG = 125 mg/dL – TC = 215 mg/dL. Fats … Current Beliefs – do you agree? • Cholesterol in foods (e.g., eggs, dairy) elevates cholesterol levels in the body. • Dietary fats do not improve HDL-cholesterol levels – effect of exercise, gender, alcohol. • Saturated fats increase LDL-cholesterol levels = increased CVD risk. • High fat diets increase LDL-cholesterol levels = increased CVD risk. • High HDL-cholesterol levels reduce risk of CVD. • CVD risk is influenced more by HDL- and LDL-cholesterol levels, and less by triglycerides. • High carbohydrate diets improve lipid profiles. Fats … New Research on Lipids: • On LDL-cholesterol levels: o Small (dense) LDL-subtype particles can easily penetrate the arterial wall. o Large, LDL-subtype particles resemble fluffy, cotton balls – too large to penetrate arterial walls – do not increase risk of CVD. o Saturated fats elevate large subtype of LDL-cholesterol. • On HDL-cholesterol levels: o Does elevated HDL cholesterol lower risks for heart disease? o Small risk-lowering effect ONLY. o Eating saturated fats elevates HDL-cholesterol levels. Fats … New Research on Lipids: • On Total Cholesterol : HDL ratios (TC:HDL): o Unsaturated fats replacing saturated fats in the diet DO lower TC:HDL ratios. o Carbohydrates replacing saturated fats in the diet DO NOT change TC:HDL ratios. But, the effect of carbohydrate + unsaturated fat has 2x larger effect on improving TC:HDL ratios than just adding saturated fat to the diet. o Replacing trans-fats with any other fats or a carbohydrate + fat combination does improves TC:HDL ratios. • On Triglycerides: o Carbohydrates added to the diet elevated TG levels – elevated TG are associated with increased CVD and diabetes risk. Fats … New Research on Lipids: • On Medium Chain Triglycerides (MCTs): o Fats are easily absorbed – pass to liver. o Lauric acid increases HDL-cholesterol, but also raises total cholesterol and TC:HDL levels. o Coconut Oil: Highly saturated, but 50-60% MCT (lauric acid) with remaining 40% being long chain, saturated fatty acids. Believed to elevate metabolic rate (60 kcal) with 1 – 2 TBL / day. Believed to have small appetite suppressing effect. Weight Loss Study: • 2 TBL v. soybean oil. • No weight loss difference after 3 months. Heart Health Study: • 20% kcal from coconut oil. • 8% LDL increase (5 weeks) Dementia • • • MCTs convert to Ketones with Alzheimer’s – brain loses capacity to metabolize glucose Ketones provide necessary fuel. No strong evidence with coconut oil. Fats … The A-List Type of Fat Compounds Examples Polyunsaturated Fats • Omega 3’s • ALA with good ratios • Flaxseed Oil, Canola Oil • Almonds & Walnuts Monounsaturated Fats • Lower Risk for CVD • Olive Oil, Canola Oil The Avoid List Type of Fat Trans-fats Compounds • Hydrogenated compounds Examples • Any listed as Trans-fats Highly Saturated Fats • Long-chain saturated fats • Beef, Butter, Lard, Palm Kernel Oil Certain Vegetable Oils • Fats with poor O-6 to O3 ratios • Corn oil, Safflower oil, Sesame oil, Peanut oil • Effect of high carbohydrate diets and lauric acid risk on CVD appear to be uncertain. • Effect of saturated fats on CVD risk appears to be debatable. Your Turn … Think-Pair-Share – Quick Quizlets. • Question 1: Are EPA/DHA and ALA found in foods the same? • Questions 2: Why do we need to monitor our Omega-6 fat intake in relation to creating healthy levels of Omega-3 fats in the body. • Question 3: How can one improve their overall lipid profile? Energy Pathways – Overview FATS - Triglycerides CARBOHYDRATES Fatty Acids + Glycerol Glucose / Glycogen Aerobic Anaerobic The Energy Pathways … The Energy Pathways Aerobic Anaerobic Large Energy Source Produces Energy Slowly Uses all 3 Macronutrients Limited Energy Source Produces Energy Rapidly Uses Carbohydrates Only Time of Maximal Performance 100 90 80 70 60 50 40 30 20 10 0 20 30 40 50 60 70 80 90 100 % Anaerobic % Aerobic 0 10 The Energy Pathways … FATS - Triglycerides CARBOHYDRATES Fatty Acids + Glycerol PROTEIN S Glucose / Glycogen Amino Acids D Deamination E Glycolysis H Glucogenic Lactate I Ketogenic Pyruvate Sarcoplasm Mitochondria B Beta Oxidation A Acetyl-CoA Ketone Bodies G F C Electron Transport Chain Ammonia Krebs Cycle Urine Urea J Macronutrient Fuels … Amino acids classified as Glucogenic or Ketogenic: • Ketogenic: Can only be converted to intermediate products that feed into metabolic pathways to make energy or fats (FFAs). o When and why? o Demand for energy > rate of energy production if carbohydrates are lacking. • Glucogenic: Have ability to be converted to glucose (manufacture of glucose from non-carbohydrate source = Gluconeogenesis). o When and why? o Glucose needed for red blood cells and liver; glycogen depletion in cells; Demand for energy > rate of energy production if carbohydrates are lacking. Ketogenic Glucogenic/Ketogenic Glucogenic 2 L’s: • Leucine (EAA – BCAA) • Lysine (EAA) PITTT: • Phenylalanine (EAA) • Isoleucine (EAA – BCAA) • Threonine (EAA) • Tryptophan (EAA) • Tyrosine (NEAA) – from Phe • Histidine (EAA) • Valine (EAA – BCAA) • 10 NEAA The Energy Pathways … Ketone Bodies Acetoacetate Beta-hydroxybutyrate Fuel – Almost all organs (not liver, not RBC) Acetone Survival during food-deprived periods After 72 hours CHO depletion: • Brain derives ~25% energy from ketones • Can increase to 70% in 6 weeks. Acetone = waste product – excreted via urine/breath. • Produced from acetoacetate breakdown (within 5 hours if not used for energy). • Contributes to some weight loss in ketogenic diets – excreted = 150 – 250 kcal / day via urine / breath (‘fruity’ acetone breath). • Brain = 2 % of body weight (3- 4 lbs.), but consumes 20 % of RMR / up to 25 % of blood glucose. o When brain feeds off ketones v. glucose – alters ratio of glutamate (excitatory NT) to GABA (inhibitory NT) = less brain excitation (epilepsy) / fogginess. Metabolism and Breakfast … Fasted Cardio? Idea – morning workout to burn more fat. • Example: 300 kcal session: • 180 kcal from fat to 240 kcal from fat = 60 more fat kcal. • 3,500 kcal = 1 lb. fat (requires 58 sessions). Fats (60%) Fats (80%) But at what cost??? CHO (20%) Dinner – Carbohydrates • Muscle and liver glycogen filled. • Evening activities – bedtime. • Overnight fast – bodily functions: o Muscle can’t release glucose to blood. o Liver’s role is to maintain blood glucose. CHO (40%) Muscle Liver Muscle Liver Muscle Liver Metabolism and Breakfast … Metabolism and Breakfast Fasted States: • Results = increased cortisol: o Promotes lipolysis (fat breakdown) – needs carb byproduct. o Inhibits glycolysis (carbohydrate breakdown). o Stimulates gluconeogenesis (breakdown of certain proteins). • Outcomes: o Ketone production (incompletely metabolized fats) = sweet smell (not harmful in small quantities – but do compromise lactate buffer. o Possible protein breakdown = ammonia smell. o Elevated cortisol can suppress metabolism. Muscle o Elevated cortisol can damage hippocampus in brain. o Metabolic Survival States Solution – eat some carbs to reduce Cortisol. Liver Liver Your Turn … Think-Pair-Share – Quick Quizlets. • Question 1: Why does the body produce ketones – are they harmful in moderate dosages? • Questions 2: Why would the body need to utilize proteins within the energy pathways? • Question 3: Why is breakfast so important? • Question 4: What science is lacking from the popular concept of fasted, morning exercise? HIIT Solutions True HIIT Solutions New Approaches and Ideas… Duration of Event Event Intensity Primary Energy System 0 – 6 seconds Extremely High Phosphagen 6 – 30 seconds Very High Phosphagen and Fast Glycolytic 30 – 120 seconds High Fast Glycolytic 2 – 3 minutes Moderate Fast Glycolytic and Oxidative > 3 minutes Lower Oxidative Phosphagen System 100% Fast Glycolytic System 75% Percentage Contribution of the Energy Pathway 50% Aerobic System 25% 0% 0 10s 30s 120s Duration of Maximal Performance Exercise New Approaches and Ideas… Fast Glycolytic System CARBOHYDRATES (Glucose/Glycogen) ATP = Energy + ADP + Pi + H+ Glycolysis (ANAEROBIC) Pyruvate Lactate- + H+ AEROBIC RESPIRATION Larger Amounts of Energy Small Amounts of Energy New Approaches and Ideas… Muscle Lactate (Lactate- + H+) cannot remain in muscle (shuts down) Sodium Bicarbonate buffer (NaHCO3) Blood Lactate (Lactate- + H+) lowers blood pH (7.35 – 7.45) Recovery within Blood !!! What about Circuits? New Approaches and Ideas… Trending: HIIT workouts – why? • Weight loss belief – potentially increased caloric burn during session + EPOC (afterburn)? • Time-efficiency* – shorter workouts (e.g., 3x20 sec, 3x / week – Timmons, UK) o Up to 90 % less training volume (amount of work performed) o Up to 67 % lower training time • Improved performance – aerobic and anaerobic improvements (Tabata, 1996) • Improved health* – blood glucose control • Increased metabolism* – fat burning ability * Research focused primarily on HIIT, not HVIT New Approaches and Ideas… Do you Understand? HIIT HVIT Defined by maximal or near maximal performance (movement quality) Defined by some measure of effort (movement quantity) Objectively measured Subjectively measured Example: best 40-yard sprint time (e.g., 5 seconds) Example: Pushing hard possible under fatigue, but 40-yard dash in 7-seconds Work interval shorter than recovery interval Work interval longer or same duration as recovery interval Goal = improve performance (bigger, stronger, faster) Goal = questionable Calories, but at what cost? As intensity drops, so does kcal burn rate New Approaches and Ideas… Maximal 60-sec Performance (N=8) Work Interval Recovery Workout 1 (HIIT) Workout 2 (HVIT) Mean: 320 watts Mean: 320 watts 5 Intervals (1-to-3 ratio) 60-sec @ 288 watts (90%) 10 Intervals (1-to-1 ratio) Interval 1 – 2 @ 288 watts (90%) Interval 3 – 4 @ 233 watts (73%) Interval 5 – 6 @ 192 watts (60%) Interval 7 – 8 @ 160 watts (50%) Interval 9 – 10 @ 135 watts (42%) 180-sec recovery @ 75 watts 60-sec recovery @ 75watts Total Duration 20-min 20-min Calories – work 18.7 kcal / min 10.3 (9-10) – 18.7 kcal / min (1-2) Calories – recovery 7.0 kcal / min 7.0 kcal / min 198.5 kcal 211.6 kcal ? ? 7.8 (subjective) 5.8 (subjective) Total Kcal EPOC Experience New Approaches and Ideas… Work Recovery Recovery Recovery Work Recovery Recovery Recovery Work Recovery What are we supposed to do during recovery intervals? Work Interval Recovery Interval Type II fibers Type I fibers Lactate shuttle Active pump • Transition from Type II fibers (anaerobic ) to type I (aerobic) or change modality? • How? o Stabilization exercises. o Balance and postural control. o Aerobic activities. New Approaches and Ideas… Using Active Recoveries Triset (mini-circuit): • Bb Clean and Press (45-sec). • Db Side Lunges with upward trunk rotations (30-sec each way). • Single Leg Db RDL with bilateral rows (30-sec each way). ~ 165 seconds of work = 1:2 (330 sec recovery) Active (generalized or whole-body) recovery – lactate buffer Active Recovery: • Light Movement – walking (30-sec) + transition (15-sec). • Plank Walk-ups (30-sec) + transition (15-sec). • Rotational Planks (30-sec) + transition (15-sec). • Single-leg Leg Swings and Hip Drivers (3D) (30-sec per leg) + transitions (15 sec). • Turkish Get-ups (30-sec each side) + transition (15-sec). • Light Movement – walking (45-sec). • Prep for next set (30-sec). Tri-set (mini-circuit): • Bb Deadlift (45-sec). • Standing Kb Rear Rotational Presses (30-sec / side). • Multi-planar Kb Goblet Lunges (60-sec). New Approaches and Ideas… VIIT: Variable-intensity interval training • Mixed pursuit of: o High-intensity (performance) intervals – more HIIT intervals = calories + EPOC o Overall improved technique = reduced injury potential o Positive experiences Watch performance – objective work output, technique or decrement in performance Work Recovery Work Recovery Work Recovery Work Recovery Work Recovery New Approaches and Ideas… Watch performance – objective work output, technique or decrement in performance Or consider hybrids: • Variable Interval Training (VIT) / Variable Recovery Training (VRT) • Variable Modality Training (VMT) Work Integrated: Recovery Work Recovery Recovery Recovery Work Recovery 1 2 3 4 5 5-10 min 5-10 min 5-10 min 5-10 min 5-10 min Work 6 Recovery 7 5-10 min 5-10 min Your Turn … Think-Pair-Share – Quick Quizlets. • Question 1: How do the work-to-recovery ratios differ between True HIIT and HVIT workouts (what fitness industry describes as a HIIT workout)? • Question 2: Identify one growing concern associated with HIITstyle training? • Question 3: What is one fundamental difference between true HIIT and a VIIT workout? • Question 4: What unique differentiator exists between a VMT workout and a HIIT workout? Upper and Lower Movement Mechanics Upper Extremity Lower Extremity Movement Mechanics … Shoulder Abduction Frontal Plane Action Application: • Internally rotate the arms and abduct as high as possible – notice end ROM. • Externally rotate the arms and abduct as high as possible – notice end ROM. Difference? • Impingement of greater tuberosity (humerus) against coracoid process (scapula) – space is generally small (~ 5-10 mm). Implications for Movement: • Caution against excess shoulder abduction with internal rotation = bursitis and tendonitis (supraspinatus and biceps long head). • Example: Upright rows, front and lateral raises. Movement Mechanics … Shoulder Abduction Scaption Plane Action Application: • Perform a lateral raise movement with the arms in the frontal plane – notice any resistance to movement? • Perform a lateral raise movement with the arms 30° forward in the frontal plane – notice any resistance to movement? Difference? • With arms 30° forward to frontal plane, greater tuberosity falls in line with highest point of coraco-acromial arch - experiencing least amount of resistance. Implications for Movement: • Perform lateral raises with slight external rotation or forward 30° in frontal plane. • Example: Moving from 3 / 9 o’clock position to 4 / 8 o’clock position for shoulder flexion exercises (press, lat pull-down, lateral raises). Movement Mechanics … Overhead Press Frontal Plane Action Application: • Three heads offer anterior, middle and posterior containment of shoulder (lowered position). • Place index finger and thumb over origin and insertion points of anterior deltoid perform overhead raise movement. Difference? • Observe external rotation of humerus - changes muscle’s orientation. • Arm lowering - no anterior stabilizer to prevent anterior humeral displacement (exacerbated with behind the head presses). Implications for Movement: • Overhead positions – External humeral rotation creates no anterior containment beyond passive structures – need to engage lats as stabilizers. Movement Mechanics … Scapulohumeral Rhythm Force-Coupling Vectors Direction, Magnitude and Timing Movement application? • 180° abduction - scapular and glenohumeral (GH) joint movement ratio = ~ 2to-1. o 2° of GH motion for every 1° of scapular motion (120°-to-60° ratio). • True scapulae movement = 45 – 60° upward rotation coupled with: o 20 – 40° posterior tilt. o 15 – 35° external rotation. o All designed to reduce encroachment into sub-acromial space. Movement Mechanics … Scapulohumeral Rhythm Scaption Plane Action Glenoid fossa (GF) is ⅓ size of the gleno-humeral head (GH) • Golf ball & tee analogy - labrum increases socket depth by 50 %. • Due to GF-GH shape, rotator cuffs (RC) collectively coordinate GF-GH movement: o Compress, depress, stabilize and steer the humeral head within socket constrained within 1-2 mm of center of glenoid fossa (creates ICR). o Also function to clear humerus from acromion process. RC muscles play important role in initiating movement and facilitating humeral inferior glide. Muscle Function Supraspinatus Abduction + compression/depression during arm elevation + slight external rotation (ER). Infraspinatus + Teres Minor ER + compression/depression during arm elevation. Subscapularis Internal rotation (IR) + compression/depression during arm elevation Movement Mechanics … Scapula dyskinesis: • Represents imbalance in stability-mobility relationship. o Ineffective joint positioning; general lack of neuromuscular control of scapulae (altered muscle activation patterns). Causes Inappropriate or deficient training Repetitive trauma (overuse) Improper posture / poor positioning Structural / congenital issues Degenerative changes Shoulder Program Overall Goal • Improve parascapular stability – promote T-spine mobility & movement efficiency Movement Mechanics … Phase One: Promote Thoracic Mobility • Address planes sequentially: o Sagittal Plane 1st – Frontal Plane 2nd – Transverse Plane 3rd – most problematic. Never compromise lumbar stability !! – demonstration • Thoracic Spine Demonstrations: o Supine foam-roller. o Supine arm movement – short-to-long lever (progress to prone – short lever). Examples: Alphabets – “I”, “Y” o Spinal twists with rib-grab. o Thoracic matrix (Gary Gray). Movement Thoracic Lumbar Flexion 30 – 40° 40 – 45° Extension 20 – 30° 25 – 35° Lateral Flexion 20 – 35° 20° Rotation 35 – 45° 10 – 15° Movement Mechanics … Phase Two: Promote ST Stability • Focus: ST position & control (stability), not GH movement o Parascapular muscles best stabilized with CKC exercises (joint compression – muscles function as stabilizers). o Too challenging initially? o Start with OKC exercises o Demonstrations – use supported surfaces (e.g., floor, wall) + kinesthetic feedback ‘feel’ Shoulder Packing (reduce scapular elevation) Reverse Codman’s – short lever (alphabets) Supine Letters – short lever (“I-Y-T-W”, “Wipers”) Retract Depress Movement Mechanics … Exercise Progression (cont.). • Open-chain – elbows bent, and remain below shoulder-level. o Movement in all 3 planes (push/pull, mash and scrub). o Use supported surfaces (e.g., floor, wall) + kinesthetic feedback ‘feel.’ o Reverse Codman’s – short lever (alphabets). o Supine Letters – short lever (“I-Y-T-W”, “Wipers”). • Progress CKC exercises: o Wall presses – 3D shifts and scapular clocks. CKC Presses Scapular Clocks Quadruped Loading – progressions: Move loading positions: • Loading and 3-D weight shifts • 12 o’clock (depression). • Off-set hand position • 6 o’clock (elevation). • Elbow extension • 3 o’clock (retraction). • Lengthen moment arm • 9 o’clock (protraction). • Unstable surfaces Movement Mechanics … Transverse Plane Action Prior to heel strike instant: • Supination = calcaneal inversion to create rigidity in foot for initial contact. During heel strike instant: • Chain reaction dissipate forces upwards, thus impact forces (from heel strike) must be absorbed and dissipated. o Pronation utilizes elastic energy of the longitudinal arch. o Pronation = calcaneal eversion creates spaces between tarso-metatarsal joints to help absorb forces. Demonstrations: 1. Hands on thighs. 2. Glute activation. Mechanics: 1. Internal tibial vs. femoral rotation = valgus stress (ACL). Heel strike – supination Joint Protection: Passive: Deltoid, MCL ligaments Active: Glutes, lateral hip complex Movement Mechanics … Frontal Plane Action Weight transference to stance-leg during gait. • During load response instant – body experiences a weight shift over stance-leg while preserving optimal alignment between the hip, knee and foot. o 1 - 2” lateral hip shift + small hip tilt (~ 4 - 5°). Knee stability is maintained via collaborative actions of: • Stance-side gluteal group + contralateral (opposite) quadratus lumborum. • Muscle weaknesses = increased probability of knee injury. Demonstrations: 1. Hip shift to single-leg with hands on hips. Mechanics: 1. Hip and trunk control to maintain alignment and avoid excessive hip adduction. Quadratus Lumborum Gluteal Group Movement Mechanics … Seated Hip Abduction / Adduction: • Aesthetics v. Function? o Aesthetics – you cannot overcome estrogen’s role of fat deposition in thigh region – more muscle tone may help. o Function: Normal hip abduction = 45° and normal hip adduction = 20°. Machines force angles > 45° = altered pelvic position and lumbar stress. Gluteus medius function – concentric or eccentric? − Lifestyle (e.g., holding child) and knee consequences. − Preferred exercises – balance/core = kcal + function. Movement Mechanics … Sagittal Plane Action Hip flexion = 110 – 120° of flexion an average of ~ 95° needed during bend-and-lift movements. • Individuals exhibit ‘glute-dominant’ or ‘quad-dominant’ patterns. • MUST shift pelvis posteriorly during the downward phase to facilitate adequate hip flexion. Glute Dominant Quad Dominant Muscles Glutes, hamstrings, calves Quads Gender Male generally Female generally 1st 10 - 15° of downward phase = pushing hips backwards (“hip-hinge”) 1st 10 - 15° of downward phase = shearing forces increasing across knee (quadriceps try control anterior tibial translation). Movement Demonstration: 1. Hands over hamstrings with two movements Eccentric Hamstrings pull Women and knee Injuries: 1. ACL injury potential = 4-6 x greater in females vs. males in same sport. 2. ~ 70 % ACL injuries = non-contact (jumping, landing, stopping, directional change). Although tibia is more fixed in closed kinetic chain, the hamstrings help control anterior translation of the tibia Movement Mechanics … Key Areas of Emphasis: • Promote Ankle Mobility Ankle (mobility) Knee (stability) Hips (mobility) • Limitations: o Supination/Pronation – Subtalar joint (talus-calcaneus o Dorsiflexion/Planta flexion – Talocrural joint o Inversion/Eversion – tarso-metatarsal joints (cuboid/navicular) Movement Mortise ROM Dorsiflexion 20° Plantar flexion 45 – 50° Inversion 20° Eversion 10° Ankle (Structure) Mobilization for Mortise: • Stand on elevated platform with strap or elastic wrapped around talus – anchored downward. • Move into dorsiflexion. Movement Mechanics … Ankle (mobility) Knee (stability) Hips (mobility) Key Areas of Emphasis: • Promote knee stability: o Unloaded (body weight) Hamstrings (sagittal) – Knee Flexor or Extender? Gluteus Maximus (transverse plane) Gluteus Medius (frontal plane) – Open- v. Closed-chain? o Progress to Jump-landing mechanics (cheek-to-cheek, nose-over-toes). • Promote hip mobility: Movement ROM Hip Flexion 110 – 120° Hip Extension 10 – 15° Hip Abduction 40 – 50° Hip Adduction 20 – 30° Stability-Mobility – NASM Overhead Squat Stability Mobility Stability-Mobility NASM Overhead Squat Stability-Mobility … • Fundamental trait we all share –move efficiently. o Efficient movement requires appropriate stability, while simultaneously promoting appropriate mobility. Stability Ability to maintain or control joint movement or position. Must Never Compromise Each Other Mobility Arthrokinetics (joint movement) Movement Efficiency Neural Control (software) Possess uninhibited ROM around a joint or body segment Muscle Properties (hardware) Stability-Mobility … Let’s examine walking – from heel strike to toe-off. Stability-Mobility … Foot is highly adaptable: Rigid lever to mobile adaptor. • • • • Calcaneal position at – heel strike (examine your shoe-wear pattern – why?). Calcaneal position at heel strike (supination). Calcaneal position at load response (pronation). Calcaneal position at toe off (supination). Calcaneus = horse… Talus = saddle… Tibia/Fibula = rider… Stability-Mobility … What Happens if the Body Loses / Lacks these Properties? • Step One: Law of Facilitation = ‘Dyskinesis’ o Compensation: Compromised stability to facilitate mobility. o Compensation: Movement into other planes. Example: Seated Leg Extension – why? Example: Bird-dog – why? • Step Two: Loss of stability = injury potential. o Chronic overuse injuries versus acute injuries. Low back – stable ! Knees – stable ! Shoulder girdle – stable ! 80 – 90% of all adults 200,000 ACL injuries/year. 70 – 75% non-contact. 21% of population with 40% persisting < 1 year $100 billion annually $650 million (surgery + rehabilitation) $39 billion annually Stability-Mobility … NASM Overhead Squat Integrated movement between two extremities - bend-and-lift coupled with an overhead reach. • Consider qualifying your client for the overhead squat with an overhead reach FIRST! Instructions: • Stand against support surface (e.g., wall) – try to rest sacrum, shoulders and head (not necessarily feet). • Observe shoulder blade position and back of head – alignment. • Relax arms at sides – observe arm position. Score 1 2 Description Pain indicated and unable to perform the movement. • Shoulders don’t make contact (i.e. shoulders in flexion, anterior tilt, or protraction). • Head does not make contact (i.e., forward head position). • Arms do not lie adjacent to side of body. • Arms are not extended (i.e., elbow extension). Stability-Mobility … Instructions: • Slowly move arms overhead to end-range of motion • Observe quality and quantity of movement in shoulders and back. Score 3 3 4 Description Arms: • Fail to reach 170 – 180° of shoulder flexion. • Arms move into different plane (demonstrations). • Identify bilateral asymmetry in arm movement. Trunk: • Loss of contact of 3 anchor points (head, shoulders, sacrum) from support. • Increased lumbar lordosis – observe ball movement or decreased BP pressure. • Trunk movement in frontal or transverse plane to achieve end-ROM. Completes at least 2 repetitions with good form. Stability-Mobility … Desired Movement? Observe Validate • Identify desired • Explain – demonstrate planes of movement – practice trials • Identify regions of • Observe movement stability and mobility efficiency and throughout kinetic limitations chain Lever (bone) Joint Lever (bone) Educate • Identify where • Coaching / (locations and correcting movement movement breakdown) • Identify why (possible reasons) Lever (bone) What has happened here? What happens to muscles on this side of joint? What happens to muscles on this side of joint? Lever (bone) What needs to be done? Stability-Mobility … NASM Overhead Squat Repetition 1st repetition: • 2nd repetition: 3rd repetition: • • What to Observe Front View Observe the stability of the foot (i.e., evidence of pronation or supination). Observe the alignment of the knees over the 2nd toe. Observe the overall symmetry of the entire body over their base of support (i.e. any evidence of a lateral shift or rotation). • Movement: Feet remain stable (i.e., no movement) – movement is through the ankle. • Observe: Feet during the movement. • Validate: Why would they move? What does this now mean? Feet Turn Out Where are you tight muscles? Ideal Compensation Stability-Mobility … NASM Overhead Squat Repetition 1st repetition: 2nd repetition: 3rd repetition: What to Observe Front View • Observe the stability of the foot (i.e.) evidence of pronation or supination, eversion or inversion. • Observe the alignment of the knees over the 2nd toe. • Observe the overall symmetry of the entire body over their base of support (i.e. any evidence of a lateral shift or rotation). • Movement: Middle of each knee remains directly over your 2nd/ 3rd toe – knees move in the sagittal plane. • Observe: Knees during the movement. • Validate: Why would they collapse inward or fall outward? What does this now mean? Knees Fall Inward Where are your tight muscles? Ideal Compensation Stability-Mobility … NASM Overhead Squat Repetition What to Observe Front View 1st repetition: • Observe the stability of the foot (i.e.) evidence of pronation or supination, eversion or inversion. 2nd repetition: • Observe the alignment of the knees over the 2nd toe. 3rd repetition: • Observe the overall symmetry of the entire body over their base of support (i.e. any evidence of a lateral shift or rotation). • Movement: Hips remains aligned over the feet. • Observe: Hips during the movement – best viewed from behind. • Validate: Why would they shift? What does this now mean? Body Shifts to One Side Where are your tight muscles? Stability-Mobility … NASM Overhead Squat Repetition What to Observe Side (sagittal) View 1st repetition: • Observe whether the heels remain in contact with the floor throughout the movement • Movement: Feet remain stable (i.e., flat on the floor – no heel elevation) – movement is through the ankle. • Observe: Feet during the movement. • Validate: Why would they move? What does this now mean? Heels Lift Off the Floor Where are your tight muscles? Ideal Compensation Stability-Mobility … NASM Overhead Squat Repetition 2nd repetition: • What to Observe Side (sagittal) View Observe for ‘glute’ or ‘quad’ dominance (i.e., downward phase starts by driving knees forward v. pushing hips backwards). o Women = more quad dominant; men = more glute dominant. • Movement: Hips move backwards to initiate the downward movement - the knees move forward once hips have moved backwards • Observe: Timing and presence of forward movement of the knees. • Validate: Why would they move early or perhaps not move? What does this now mean? Knees Move Forward Immediately What is the concern? Compensation Ideal Stability-Mobility … NASM Overhead Squat Repetition What to Observe Sagittal View 3rd repetition: • Observe position of the spine – should remain neutral or flat (sacrum to head) • Movement: Spinal alignment at three points is maintained – head, shoulder blades (thoracic spine) and hips (sacrum) • Observe: Alignment of the spine during the movement. • Validate: Why would it not maintain good alignment? What does this now mean? Back Arches or Bows Upward Where are your tight muscles? Ideal Compensation Stability-Mobility … NASM Overhead Squat Repetition 4th repetition: • What to Observe Side (sagittal) View Observe whether a parallel alignment between tibia and torso is achieved in lowered position (i.e., figure-4 position) v. T-formation. • Movement: Movement: Trunk/arms and tibia achieve a parallel alignment in the lowered positon. • Observe: Alignment between each body segment. • Validate: Why would they not be aligned? What does this now mean? Body Does not Attain Parallel Alignment Where are your tight muscles? Ideal Compensation Stability-Mobility … NASM Overhead Squat Repetition 5th repetition: What to Observe Side (sagittal) View • Observe alignment between torso and arms. • Movement: Trunk and arms maintain a parallel alignment in the lowered positon. • Observe: Alignment between these two body segments. • Validate: Why would they not be aligned? o What does this mean? o Lats and pecs v. posterior complex (traps, rhomboids) Ideal Compensation Corrective Exercise CEX Strategies Corrective Exercise … Systematic process of restoring proper levels of stability and mobility for movement efficiency. Stability Must Never Compromise Each Other Ability to maintain or control joint movement or position. Mobility Possess uninhibited ROM around a joint or body segment Inhibit / Release Lengthen Strengthen (type I fibers) Integrate Myofascial Release Static Stretching Positional Isometrics Integration (Mobility) (Mobility) (Stability) (Integration) Corrective Exercise … Body’s primary communication system. Passive System Skeleton, joints (capsules), ligaments, tendons, and skin that offer support to regulating movement. Neural Control System Movement Actively -passive System Contains inelastic and elastic components that generate force, absorb energy (from outside forces – i.e., deceleration), and harness energy into movement (i.e., absorbing impact forces eccentrically – then utilized for concentric action). Active System Fascial tissue spanning entire body at various levels (i.e., deep, superficial) – capable of resisting unmerited compressive forces, yet also withstand unmerited elongating forces (i.e., strain) – called ‘tensegrity’ (all 4 systems in unison provide human tensegrity). Corrective Exercise … Inhibit What is Fascia? Actively-passive System • Fascial tissue = specialized tissue different from muscle. • Continuous throughout body at multiple levels: o Separates tissue. o Surface area for muscle attachment to bone. o Able to provide stability through tension (stretching/lengthening) v. muscles with compression/contraction. • Contains up to 9x more receptors than muscle – sensitive to mechanical stimuli Corrective Exercise … Inhibit • How does it Function? Mennel’s Truisms. o Meatball-plate analogy. o When joint is NOT free to move – muscles moving joint do not function optimally = dysfunction within muscles . o Muscle function cannot be restored if joints are not free to move. o Myofascial release (MR) focuses on neural-fascial systems – alleviates myofascial trigger points (knots) and areas of hyper-irritability to improve soft tissue extensibility and function. Knot = fibers out of alignment – MR relaxes and aligns fibers. Corrective Exercise … Inhibit Foam Rolling Methodology #1 – Foam Rolling • • • Compression Techniques Methodology #2 – Compression Techniques Identify trigger areas (tender spot). • Roll over segment or 3-6” area of • localized tenderness for approx. 30 sec • (> 30 reps) until discomfort subsides. Little discomfort (not pain) = appropriate (feel good-pain) Perform 1 – 2 sets 1 – 2x per muscle per day Identify trigger areas (tender spot). Apply load (body weight) Move joints or move body over compression points o Sagittal = Roll o Frontal = Mash o Transverse = Scrub Perform up to 10 reps/movement direction 1 – 2x per muscle per day Corrective Exercise … Static (passive) Stretching • Modality: Low-force, longer-duration stretch that slowly increases muscle length. GTO activation Immediate low-grade muscle spindle (MS) activity Inhibits MS activity (temporary increase in muscle tension). Low-grade muscle response quickly decreases (MS desensitization) as stretch duration progresses (first 5 seconds). After 7 – 10 seconds, muscle tension activates GTO response Allows for inelastic tissue stretching (creep / remodeling) Hold for 5 – 50 additional sec Total stretch: 4 x 15-60 sec Principle known as Autogenic Inhibition Corrective Exercise … Ever notice how after ~10 seconds, you feel less resistance within the stretched muscle? • Application: to effectively stretch muscle, you need at least 7-10 seconds just to shut down nerve activity before you can actually apply a stretch load (strain) to the connective (muscle) tissue. o Guidelines: 4 reps x 15 – 60 sec each. • After removing stretch stimulus, MS quickly re-establishes stretch threshold again. o ~ 70 % MS recovery within 1st 5 seconds. • Application: Perform repetitions with minimal recovery between each rep. Static Stretching Turns Off Muscle Activity Corrective Exercise … Muscle Activation Techniques (MAT) Another technique to turn on or turn off muscles • Modality Example: Low-grade isometric contractions (50 % of maximum force for 6 - 15 seconds) reduces MS activity within active muscle (agonist) after contraction and also within opposite (antagonistic) muscle. o In same muscle = Autogenic Inhibition o Example: Activation of glute maximus temporarily inhibits MS after contraction – follow with stretch of that muscle. In opposite muscle = Reciprocal Inhibition. Example: Activation of glute maximus temporarily inhibits MS activity within iliopsoas (hip flexors) – follow with stretch of antagonistic muscle. Important to initiate the stretch immediately following inhibition of the muscle spindle due to its rate of recovery. Corrective Exercise … Strengthen Type I Fibers Type II Fibers Force Production Low-force, longer duration Higher-force, shorter duration Primary Energy Pathway Aerobic Anaerobic Role Stabilizers (tonic) Mobilizers (Phasic) • Located in greater concentrations closer to spine – stabilization role o What type of training is preferred? Higher-force, shorter duration..? Lower-force, longer-duration..? Corrective Exercise … Strengthen Positional Isometrics (PI) Position Frequency Neutral 3 – 5 days/week Sets Minimum 1 Reps Start with 4 Tempo Minimum 4-sec hold Tempo 2-sec rest Intensity Start between 25 – 50 % of maximal intensity. Dose-related Effect Integrate = Foundational Training NASM’s exclusive discount for Evolution Fitness Attendees • 30% off select NASM Certified Personal Trainer (CPT) Packages • 20% off all NASM Specializations Visit NASM Booth 1017 in the FitExpo Hall to receive discount http://www.nasm.org/continuing-education/workshops/conference-sessions *Discount only valid when purchased at NASM’s booth on January 23-24, 2016. Discounts exclude Life Time Academy and Exam Only packages. www.nasm.org Core Essentials in Exercise Science THANK YOU..!! Fabio Comana Fabio.comana@nasm.org For Your Commitment to Excellence www.nasm.org Questions... ?? Core Essentials in Exercise Science