INFRATEMPORAL FOSSA AND MUSCLES OF
advertisement

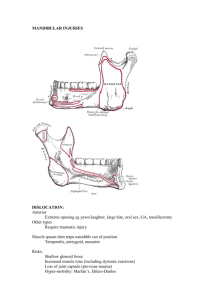
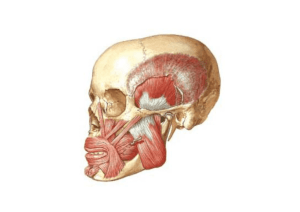
INFRATEMPORAL FOSSA AND MUSCLES OF MASTICATION Learning Objectives By the end of the course students will be able to: 1. Identify the muscles of mastication and give their functions. 2. Define the boundaries and contents of the infratemporal fossa. 3. Identify the branches of the trigeminal nerve and their functions related to mastication and sensation from the face. 4. Identify the chorda tympani nerve and give its function. 5. Describe the structure and function of the temporomandibular joint. 6. Describe the submandibular and sublingual salivary glands and give their innervations. Reference: Moore, Clinically Oriented Anatomy, chapter 7 Particularly relevant Blue Boxes in Moore: ●Inferior Alveolar Nerve Block, p. 927. ●Dislocation of the TMJ, p. 927 TEMPORAL AND INFRATEMPORAL REGIONS INFRATEMPORAL FOSSA (Moore 916-921) Boundaries: The infratemporal fossa is the area in the skull below the zygomatic arch. It is bounded anteriorly by the maxilla, laterally by the ramus of the mandible, medially by the lateral pterygoid plate and superiorly by the sphenoid bone. The major artery in the infratemporal fossa is the maxillary artery, a branch of the external carotid (remember SALFOPSMAX). Nerves in the Infratemporal Fossa (Moore 921; Netter 45): Mandibular Division of Trigeminal Nerve - V3 (Netter 45) General Description -- passes through foramen ovale to infratemporal fossa. Motor root -- innervates the four muscles of mastication (temporalis, masseter, medial pterygoid, lateral pterygoid), mylohyoid, anterior belly of digastric, tensor veli palatini, and tensor tympani. Sensory root -- innervation to temporal region, anteriorsuperior ear, external acoustic meatus, general sensation for anterior 2/3 of the tongue, mucous lining of cheek, lower teeth and gingiva, sensory to lower jaw. Pathways of V3 After passing through foramen ovale into the infratemporal fossa, V3 forms a trunk with the following branches: 1. Meningeal branch - returns to cranial cavity through foramen spinosum with middle meningeal artery; distributes with this artery to the dura mater. 2. Medial pterygoid nerve -- nerve to this muscle; also branches to tensor veli palatini and tensor tympani. Main trunk then divides into: A. Anterior Division - mainly motor; one sensory branch (buccal nerve). 1. Masseteric nerve - nerve to masseter muscle; also branch to temporo-mandibular joint. 2. Deep temporal nerves -- anterior and posterior branches to temporalis muscle. 3. Nerve to lateral pterygoid -- nerve to this muscle. 4. Long Buccal nerve - pierces buccinator to provide sensory innervation to the inside cheek, and gingiva. (NOTE: buccal branches of Facial Nerve - VII, provide motor innervation to the buccinator muscle). B. Posterior Division - mainly sensory; one motor branch (mylohyoid nerve.) 1. Auriculotemporal nerve -- two roots encircle the middle meningeal artery. The nerve then passes to the temporal region accompanying the superficial temporal artery. Its branches are: a) parotid, b) articular branches to T.M. joint, c) anterior auricular, d) external acoustic meatus, e) terminal branch is superficial temporal. 2. Lingual nerve -- sensory innervation for anterior 2/3 of the tongue; joined high in infratemporal fossa by chorda tympani nerve (branch of Facial Nerve VII); emerges through petrotympanic fissure. Chorda tympani carries parasympathetic preganglionic fibers to submandibular ganglion -- synapse with post-ganglionic fibers to submandibular and sublingual glands. Chorda tyrnpani also carries taste fibers for the anterior 2/3 of the tongue. 3. Inferior alveolar nerve -- enters the mandible through the mandibular foramen as it passes along the mandibular canal; it gives inferior dental branches to inferior teeth. Mental nerve passes out the mental foramen to supply the chin and lower lip; inferior alveolar nerve continues in the canal to innervate the lower incisors. Mylohyoid nerve passes along the mylohyoid groove; it supplies motor innervation to mylohyoid and anterior belly of digastric muscles. Mylohyoid nerve arises just before the inferior alveolar nerve passes into mandibular foramen. MUSCLES OF MASTICATION (Moore 921) The Primary Muscles of Mastication: All are innervated by the mandibular (motor) division of the trigeminal nerve V3 (Netter 54, 55). The nerve to the medial pterygoid comes off the trunk of the mandibular nerve, while the other motor nerves to the muscles of mastication arise from the anterior division of the trunk. (Netter 45) 1. Temporalis Muscle Innervation - Anterior and posterior deep temporal nerves. Origin-Temporal fossa; it is a large fan-shaped muscle. Insertion - The fibers converge to pass medial to the zygomatic arch and terminate in a tendinous insertion onto the anterior and posterior aspects of the coronoid process. The terminal portion of the insertion on the anterior aspect of the ramus extends inferiorly into the retromolar triangle, extending below the occlusal plane. Action - The fibers of the muscle may be divided into three portions: i.e., anterior fibers (powerful elevators of the mandible); middle fibers (elevators and retractors of the mandible); and posterior fibers (retracts the mandible). 2. Masseter Muscle Innervation - Masseteric nerve which enters the deep side of the muscle from the infratemporal fossa by passing through the mandibular notch. Origin - Both superficial and deep. The superficial portion arises from the inferior border of the zygomatic bone. If well developed, it may also arise from the zygomatic process of the maxilla. The superficial fibers end on the zygomatic bone and do not pass the zygomaticotemporal suture. The deep portion arises from the entire length of the zygomatic arch -- from the zygomatic process of the maxilla to the anterior slope of the articular eminence. Insertion – Superficial portion inserts into the lower half of the lateral surface of the ramus. The deep portion inserts above the superficial fibers into the lateral aspect of the coronoid process and the upper part of the ramus. Action - The muscle acts as a powerful elevator of the mandible. The deep fibers assist in elevation, but also act to retract the mandible during the closing movement. 3. Medial Pterygoid Innervation - Medial pterygoid nerve. Origin - Medial surface of the lateral pterygoid plate, the pyramidal process of the palatine bone and the maxillary tuberosity. Insertion - Medial surface of the ramus and angle of the mandible. It forms a “mandibular sling” with the masseter muscle. Action - Assists the masseter in elevating the mandible. Alternate contraction of the medial pterygoids may cause a “grinding” action. 4. Lateral Pterygoid Innervation - Lateral pterygoid nerve. Origin - Dual. Upper portion originally called the sphenomeniscus muscle. It arises from the infratemporal crest and surface of the greater wing of the sphenoid bone. Lower portion arises from the lateral surface of the lateral pterygoid plate. Insertion - Upper portion has some fibers inserting into the meniscus. The bulk of these fibers blends with the lower portion and inserts into the ptergoid fovea. Lower portion inserts into pterygoid fovea. Note: In many instances, no fibers of the lateral pterygoid muscle attach to the meniscus. Action - The lower fibers protrude the mandible when acting bilaterally. Acting unilaterally, they promote lateral movement of the mandible on the opposite side, since the mandible is a single, horseshoeshaped bone. The lateral pterygoid muscle actually pulls the condyle medially on its own side. Note: The meniscus is attached to the lateral and medial poles of the condylar process, and is carried anteriorly and posteriorly with movement of the mandible proper (see TMJ section). The Accessory Muscles of Mastication These muscles assist in promoting smooth movement of the mandible upon protrusion/retrusion and opening 1. Diagastric Muscle Innervation - Anterior belly (mylohyoid nerve from inferior alveolar branch of V3) Posterior belly (cranial nerve VII-facial). Origin - Anterior belly arises from the intermediate tendon. Posterior belly arises from the mastoid notch medial to the mastoid process. Insertion - Anterior belly into the digastric fossa of the mandible. Posterior belly inserts into the intermediate tendon. Action - With the stylohyoid and infrahyoid muscles fixing the hyoid bone in postion, contraction of the digastric muscle assists in smoothing the lowering and retrusion of the mandible. 2. Geniohyoid Muscle Innervation:_ C1 Origin - Inferior mental spine (gential tubercle). Insertion - Body of the hyoid bone. Action- Aids in retrusion of the mandible. TEMPOROMANDIBULAR JOINT (TMJ) (Moore 916-921) Osteology: The TMJ (Netter 18, 54, 55) is the articulation between the temporal bone and the condyle (head) of the mandible. The temporal bone portion is divided into two parts: the posterior part is the articular fossa (mandibular fossa) and the anterior part is the articular tubercle (eminence). The term “condylar process” refers to the combined head and neck portions of the mandible. At rest, the condyle is positioned in relation to the posterior incline of the articular eminence. The condyle is not located in the roof of the fossa, which is very thin. The translucent roof is not strong enough to withstand pressure from the condyle. Articular Disc (Meniscus): The disc, or meniscus, (Netter 16, 54) lies between the temporal bone and the mandibular condyle. It is composed of dense fibrous connective tissue containing nests of cartilage cell. Therefore, it is defined as fibrous cartilage, although fibrous connective tissue would be more accurate. This disc separates the articular cavity into superior and inferior synovial cavities. The superior surface of the disc moves on the inferior surface of the articular fossa and eminence. The disc is oval-shaped and biconcave (somewhat like a “distorted erythrocyte”). It is attached to the inner aspect of the joint capsule. Anteriorly, the disc is fused to the capsule. Posteriorly, the disc connects with the retrodiscal pad of tissue (a layer of loose vascularized connective tissue). Laterally and medially, the disc is independently bound to the lateral and medial poles of the condyles, and has no direct relation to the capsule. It is this attachment of the disc to the condyle that causes the disc to move in synchrony with the condyle during its excursions. Articular Capsule: The capsule encloses the articular cavity and appears somewhat like a sleeve or collar surrounding the articular elements. It extends from its superior attachment at the margin of the fossa and eminence to its inferior attachment around the neck of the mandible. The capsule consists of an outer, fibrous layer and an inner, lining layer called the synovial membrane. The latter elaborates a lubricating and nutritional synovial fluid. The synovial membrane is highly vascularized. It lines all areas of the joint which are not subjected to pressure. Therefore, the synovial membrane is not present on the articulating surfaces of the temporal bone, condyle and disc. Classification: The TMJ is classified broadly as a diarthrodial joint. All diarthrodial joints are characterized by a covering of cartilage on their opposing surfaces. Although the cartilage is usually hyaline, it is fibrocartilage in the TMJ. All diarthrodial joints are lined by a synovial membrane. Diarthrodial joints are characterized by ligments which surround and stabilize the joint. Diarthrodial joints may or may not have a disc or meniscus. The specifics of classification list the lower joint cavity as ginglymus, or acting as a hinge. This hinge motion is displayed in passive mandibular opening; e.g., during yawning. The upper joint cavity is a freely gliding joint and so, is classified as arthrodial. The classification of the TMJ: ginglymo-arthrodial diarthrosis (diarthrodial) or a slidinghinge joint, which is diarthrodial. Ligaments: There are three ligaments associated with the movements of the TMJ: Stylomandibular - extends from the tip of the styloid process of the temporal bone to the angle of the mandible. This is not a true ligament but merely folded suprahyoid fascia which is a projection of the superficial investing fascia of the neck. Sphenomandibular - forms the spine of the sphenoid bone to the lingula of the mandible. Temporomandibular - a lateral thickening of the articular capsule. This lateral reinforcement is the only major ligamentous stabilization of the TMJ. Nerve Supply: Generally described with the aid of a modified Hilton’s Law - the nerve supply to a joint is through branches of any nerve which courses in the vicinity. The innervation of the TMJ most often described is through the auriculotemporal nerve. This nerve courses deep to the neck of the mandible and then posterior to the joint structures (in front of the ear). The nerve supply to the TMJ, per se, is not motor since the skeletal muscles which move the joint are innervated at locations usually far removed from the joint. The supply to the joint, other than autonomic to blood vessels, is sensory (i.e., pain, proprioceptive), and the receptors are mostly in the capsule and its attached structures. The masseteric nerve often supplies a proprioceptive branch to the TMJ. Blood Supply: The major arterial supply of the TMJ is derived from branches of the superficial temporal and maxillary arteries: Middle temporal and transverse facial, as well as direct branches from the superficial temporal artery. Deep auricular, anterior tympanic, middle meningeal and masseteric branches of the maxillary artery. NOTE: The tendinous fibers of the lateral pterygoid muscle insert through the capsule into the neck of the mandible and into the articular disc. Contraction of the lower head of the latral ptergoid pulls the condyle with it. (See muscles of mastication for further explanation of muscle function.) Any movement of the single, rigid mandible always involves action in both TM joints (double-jointed). Because of this bilateral relationship, the two joints are often referred to as a single unit: the cranio-mandibular articulation. Each TMJ is also “double-jointed” because each has two compartments (upper and lower) with separate actions (arthrodial and ginglymus). TEMPORAL AND INFRATEMPORAL FOSSA STRUCTURE LIST Osteology Temporal bone Zygomatic process Mandibular fossa Nerves Articular tubercle Petrotympanic fissure Trunk of V3 Mandible Otic ganglion Condyle Auriculotemporal Head, neck, fovea Inferior alveolar Mandibular fossa Mylohyoid n. Coronoid process (Long) buccal Ramus, angle, body Anterior and posterior deep temporal Lingula Posterior superior alveolar (from V2) Mandibular foramen Lingual Inferior alveolar canal Mylohyoid groove Chorda tympani (from CN VII) Sphenoid bone Greater wing Pterion Infratemporal crest Foramen ovale Foramen spinosum Lateral pterygoid plate Pterygomaxillary fissure Maxilla Posterior slope Posterior superior alveolar foramina Muscles of Mastication Masseter Temporalis Lateral Pterygoid Medial Pterygoid