ANATOMY AND FRACTURES OF THE MANDIBLE
advertisement

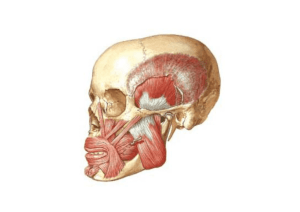
ANATOMY AND FRACTURES OF THE MANDIBLE ANATOMY Mandible interfaces with skull base via the TMJ and is held in position by the muscles of mastication Anatomic units of the mandible Muscles of the mandible – Posterior group Origin Insertion Innervation Action Masseter Inferior 2/3 zygomatic bone & medial surface of zygomatic arch Lateral ramus and angle of mandible Masseteric branch of anterior division of mandibular nerve (V) Elevate and protrude mandible Temporalis Limits of temporal fossa Medial surface coronoid process, anterior surface of ramus down to occlusal plane Two deep temporal branches of mandibular nerve (V), sometimes reinforced by middle temporal nerve Elevates mandible, posterior fibres are the only muscle fibres to retract the mandible Medial pterygoid Pterygoid fossa, mainly medial surface of lateral pterygoid process Medial surface of ramus and angle of mandible Branch from main trunk of mandibular nerve Pulls angle of mandible superiorly, anteriorly and medially Lateral pterygoid Upper head from infratemporal surface of skull, lower head from lateral pterygoid plate Upper head inserts into TMJ capsule, lower head into anterior surface of condylar neck Branch of anterior division of mandibular nerve Lateral movement, protrusion, important in active opening of the mouth Muscles of the mandible – Anterior group Origin Insertion Innervation Action Hypoglossal nerve (XII) Depresses tongue, posterior part protrudes tongue Genioglossus Superior part of mental spine of mandible Geniohyoid Inferior part of mental spine of mandible Body of hyoid bone C1 through hypoglossal nerve (XII) Pulls hyoid bone anterosuperiorly, shortens floor of mouth and widens pharynx Mylohyoid Mylohyoid line of mandible Raphe and body of hyoid bone Mylohyoid nerve, a branch of inferior alveolar nerve (V3) Elevates hyoid bone, floor of mouth and tongue during swallowing and speaking Digastric Anterior: Digastric fossa of mandible Posterior: Mastoid notch of temporal bone Intermediate tendon to body and superior (greater) horn of hyoid bone Anterior: Mylohyoid nerve (V3) Posterior: Facial nerve (VII) Depresses mandible, raises hyoid bone and steadies it during swallowing and speaking Muscles of Mastication OUTER SURFACE Muscles of Mastication INNER SURFACE Muscles of Mastication 4 muscles of mastication Masseter Temporalis Medial pterygoid Lateral pterygoid Supplied by V3, testament to same embryologic origin as the mandible from the 1st branchial arch Masseter Divided into 3 heads Superficial: largest head Arises anterior 2/3rds of the lower border of the zygomatic arch Wide insertion to angle, forwards along lower border and upwards to lower part of ramus Intermediate: Middle 1/3 of the arch Deep: Deep surface of the arch Action: elevator and drawing forward the angle Masseter Intermediate and deep fuse and pass vertically downwards to fuse with ramus Nerve and artery divide muscle incompletely into 3 parts Masseteric nerve (Br of anterior division of V3) runs between deep and intermediate Br of superficial temporal and transverse facial runs between superficial and intermediate Temporalis Arises temporal fossa between inferior temporal line and infratemporal crest Inserts at posterior border of the coronoid process and ascending ramus Upper and anterior fibres elevate the mandible Posterior fibres (horizontal) retract the mandible (only muscles that do so) Medial pterygoid 2 heads: Deep: Larger Medial surface of the lateral pterygoid plate and the fossa between 2 plates Superficial : Tuberosity of the maxilla and pyramidal process of palatine bones Insert lower and posterior part of angle (with masseter) Action: upwards and forwards and medially Lateral pterygoid 2 heads: Superior: Infratemporal fossa Inferior: Lateral surface of the lateral pterygoid Fuse into a short thick tendon that inserts into pterygoid fovea the upper fibres passing into articular disc and anterior part of the capsule Action: side-to-side plus only muscle to open jaw Temporomandibular Joint Articulation Synovial joint between the condyle of the mandible and the mandibular fossa in the squamous part of the temporal bone Both bone surfaces covered with layer of fibrocartilage identical to the disc No hyaline cartilage, therefore an atypical joint Temporomandibular Joint Unique feature of the TMJs is the articular disc. Composed of fibrocartilaganeous tissue Divides each joint into 2: Inferior compartment Superior compartment Temporomandibular Joint Inferior compartment Allows for pure rotation of the condylar head, corresponds to the first 20 mm or so of the opening of the mouth. (opening and closing movements) Superior compartment involved in translational movements sliding the lower jaw forward or side to side Temporomandibular Joint Temporomandibular Joint Atypical synovial joint separated into upper and lower cavities by a fibrocartilaginous disc No hyaline cartilage Capsule attached high on neck of mandible around articular margin, then to transverse prominence or articular tubercle and as far posteriorly as squamotympanic fissure Fibrocartilage attached around periphery to capsule Anteriorly near head of mandible, so mobile Posteriorly near temporal bone, so more fixed Thinner in middle than periphery, crinkled fibres to allow movement and contouring Lateral TM ligament is a stout fibrous band passing from zygomatic arch to posterior border of neck and ramus, blending with capsule Sphenomandibular ligament runs between sphenoid spine and lingula of mandible Tightens with movements away from rest Remains constant tension through range of motion as the lingula is the axis of rotation of the mandible Sensation supplied by auriculotemporal nerve with some supply from nerve to masseter (Hiltons law) TMJ Ligaments 3 ligaments associated with the TMJ: 1) Temporomandibular ligament (Major) is really the thickened lateral portion of the capsule, and it has two parts: an outer oblique portion (OOP) and an inner horizontal portion (IHP) Lower border of zygomatic arch to posterior border of the neck and ramus TMJ Ligaments 2) stylomandibular ligament (minor) separates the infratemporal region from the parotid region runs from the styloid process to the angle of the mandible 3) Sphenomandibular ligament (minor) runs from the spine of sphenoid to the lingula of the mandible TMJ Ligaments The minor ligaments are important in that they define the limits of movements, ie the farthest extent of movements of the mandible. Not connected to joint However, movements of the mandible made past these extents functionally allowed by the muscular attachments BUT will result in painful stimuli TMJ Ligaments TMJ Ligaments Mandibular Forces Nerve Supply Inferior alveolar nerve branch of the mandibular division of Trigeminal (V) nerve, enters the mandibular foramen and runs forward in the mandibular canal, supplying sensation to the teeth. At the mental foramen the nerve divides into two terminal branches: Incisive nerve: supplies the anterior teeth mental nerve: sensation to the lower lip Evaluation - History Always remember ABCs of life along with secondary and tertiary survey Mechanism of injury MVA associated with multiple comminuted # Fist often results in single, non - displaced # Anterior blow to chin - bilateral condylar # Angled blow to parasymphysis can lead to contralateral condylar or angle # Clenched teeth can lead to alveolar process # Physical Exam Occlusion Change in occlusion - determine preinjury occlusion Posterior premature dental contact or an anterior open bite is suggestive of bilateral condylar or angle fractures Posterior open bite is common with anterior alveolar process or parasymphyseal fractures Unilateral open bite is suggestive of an ipsilateral angle and parasymphyseal fracture Retrognathic occlusion is seen with condylar or angle fractures Condylar neck # are assoc with open bite on opposite side and deviation of chin towards the side of the fx. Angle’s classification Class I: Normal Mesial buccal cusp of the upper 1st molar occludes with mesial buccal groove of the mandibular molar Class II: Retrocclusion, mandibular deficiency Class III: Prognathic occlusion, maxillary deficiency, mandibular excess Dental classification of occlusion Angle’s classification (1887) Based on relationship of permanent 1st molars and to a lesser degree the permanent canines to each other Class Molar relation Canine relation I Mesiobuccal cusp of maxillary 1st molar is in line with buccal groove of mandibular 1st molar Maxillary permanent canine occludes with distal ½ of mandibular canine and mesial half of mandibular 1st premolar II Buccal groove of mandibular 1st molar is distal to mesiobuccal cusp of maxillary 1st molar Distal surface of mandibular canine is distal to mesial surface of maxillary canine by at least width of a premolar Buccal groove of mandibular 1st molar is mesial to mesiobuccal cusp of maxillary 1st Distal surface of mandibular canine is mesial to mesial surface of the maxillary canine by at least the width of a Div1 – Overjet Div2 – Lingual inclination III Malocclusion Physical Exam Anaesthesia of the lower lip Abnormal mandibular movement unable to open - coronoid fx unable to close - # of alveolus, angle or ramus trismus Lacerations, Haematomas, Ecchymosis Loose teeth swelling Physical Exam Multiple fractures sites are common: 1 fracture: 50% 2 fractures: 40% >2 fractures: 10% Dual patterns: Angle contralateral body Symphysis and bilateral condyles 15% another facial fracture General Principles of treatment ABCs Tetanus Nutrition Almost all can be considered open fractures as they communicate with skin or oral cavity Reduction and fixation Post-op monitoring for N/V, use of wire cutters Oral care - H2O2 , irrigations, soft toothbrush Aims of Management 1) Achieve anatomical reduction and stabilisation 2) Re-establish pre-traumatic functional occlusion 3) Restore facial contour and symmetry 4) Balance facial height and projection Fracture Frequency Classification of Fractures Open vs Closed Displaced vs non-displaced Complete vs greenstick Linear Vs comminuted Relationship to the teeth Class I: teeth both sides of fracture Class II: teeth one side of fracture Class III: edentulous Favourable vs unfavourable Treatment options No treatment Soft diet Maxillomandibular fixation Open reduction - non-rigid fixation Open reduction - rigid fixation External pin fixation IMF IMF Islet IMF Open reduction - nonrigid fixation External Fixation Principles of fixation Usually one plate with 4 cortices of fixation are required for adequate immobilisation Anterior to mental foramen, 2 levels of fixation are required to overcome torsional forces Unfavourable fractures usually require 2 levels of fixation for stability Fixation along Champy’s line allows better fixation due to the strong buttress structure Condylar fractures Classification Condylar Intra- or extra-capsular subcondylar Watch for intracranial condylar head Condylar heads tend to dislocate anteromedially towards pterygoid plates due to pull from medial pterygoid Indications for open reduction are angulation > 30°, fracture gap > 5mm, lateral override, bilateral fractures of head/neck Risks avascular necrosis of condylar head, facial nerve injury, hypertrophic scarring (10%) Alveolar fractures 3% total fractures, often in combination with other fractures Can often be reduced and fixed with arch bars (can be acrylated) or Essig splints May require monocortical plate fixation Teeth are often insensate and require orthodontic evaluation Gross comminution or loss of blood supply increases the risk of infection and primary debridement of the devitalised segment with soft tissue coverage may be a better long term option Can have compression fractures of alveolus resulting in loosened teeth Miller Grade 1 - < 1mm looseness Miller Grade 2 – 1-3mm looseness Miller Grade 3 - > 3mm looseness and loose superoinferiorly in socket Teeth in fracture line Important in fracture stability when using IMF Less important in fracture stability when plates used to fix fractures Reasons to extract the tooth Severe tooth loosening with chronic periodontal disease Fracture of the root of the tooth Extensive periodontal injury and broken alveolar walls Displacement of teeth from their alveolar socket Interference with bony reduction and reestablishing occlusion Third molars tend to cause the most controversy Third molars that are erupting normally need not be removed unless they are interfering with fracture reduction Impacted third molars can be removed as they are rarely a functional part of the occlusion Removal of third molars unnecessarily leads to increased conversion from closed reduction to open reduction Edentulous mandible No occlusal plane Lack of mandibular height due to atrophy Changed pattern of fracture – body is more common as atrophy is greatest Changed position of inferior alveolar nerve and artery Changed pattern of blood supply – more circumferential than radial Role of recon plates and bone grafting Role of dentures Paediatric mandible Often greenstick fractures that heal within 2-3 weeks 65% mandibular fractures in children < 10yo are in condylar region, 40% in 11-15yo Arch bars are common use to avoid damage to secondary teeth, but primary teeth are conically shaped Acrylic splint secured by circumferential wiring is safe and effective Condyle is the major growth centre of the mandible and has some ability to remodel, and poorly tolerates periosteal stripping Crush of condylar head (esp. < 3y) can lead to altered mandibular growth and TMJ ankylosis secondary to haemorrhage Complications Airway esp with IMF (wire cutters and pre-op education) Infection Delayed and non-union Inadequate immobilisation, fracture alignment Inteposition of soft tissue or foreign body Incorrect technique Inferoir alveolar nerve damage 56%pre-treatment 19% post-treatment Malocclusion TMJ ankylosis esp intracapsular condyle #