Clinical correlation cirrhosis
advertisement

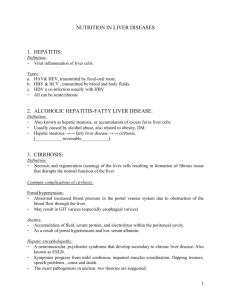
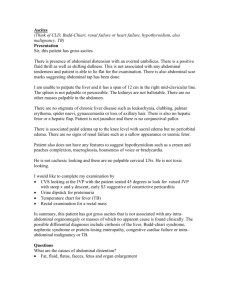
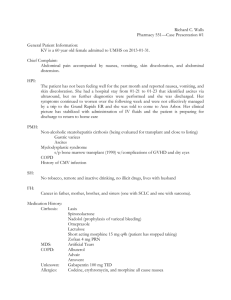
Clinical Correlation #2 4/14/04 Alexa Turner P&S ’04 Massive Ascites Case Goals of this session: To review the pathophysiology of ascites and hepatic cirrhosis To review the relevant physical findings of cirrhosis To place cirrhosis/ascites into a clinical context with a case presentation To introduce a symptom-based approach to thinking about pathophys., i.e., differential diagnosis Pathophysiology review: Ascites is the collection of fluid in the peritoneal cavity Portal-Hypertension related: Serum-ascites albumin gradient (SAAG) >1.1 9 Sinusoidal: cirrhosis (81%), hepatitis, massive liver mets, HCC 9 Post-sinusoidal: right sided CHF, Budd-Chiari Pathophysiology: 9 “Underfill Theory”: portal hypertention→transudation of fluid into peritoneum→↓plasma volume→renal Na retention 9 “Overflow Theory”: hepatorenal reflex→Na retention 9 Peripheral Vasodilation Theory: portal htn→systemic vasodilation (due to release of NO?)→↓effective arterial volume→renal Na retention 9 ↓Plasma oncotic pressure with decreased albumin Cirrhosis is fibrosis and nodular regeneration from hepatocellular injury Etiologies: Alcohol, viral hepatitis, autoimmune hepatitis, metabolic diseases, biliary tract diseases Portal HTN: Varices, melena, splenomegaly, caput medusae, ascites, testicular atrophy, hemorrhoids Liver cell failure: Encephalopathy, scleral icterus, spider nevi, gynecomastia, jaundice, asterixis, anemia, pedal edema, loss of sexual hair, palmar erythema CC: referred by GI clinic for ↑SOB, fluid overload HPI: 62 y/o male with HCV, EtOH cirrhosis, polysubstance abuse with h/o hepatic encephalopathy, ascites. Cirrhosis dx clinically and via US 12/03. Pt. has noted increased weight gain, SOB, ascites, pedal edema and poor response to outpatient diuresis. A few weeks ago 3-4L therapeutic paracentesis performed at outside hospital. Referred by GI to inpatient for therapeutic paracentesis, diuretics, possible TIPS and Liver tx evaluation. Pt. also c/o some fever/chills at home without cough, abdominal pain, melena or hematemesis. ER: Tmax 98.6 BP 108/70 P91 RR20 O2 sat 91% RA→98% on 4L NC PE: 2/6 Systolic ejection murmur, decreased breath sounds B/L, LLQ with erythematous macules PMH: Hep C/EtOH cirrhosis, polysubstance abuse, EGD: varices, ulcer PSH: s/p surgical repair of gunshot wound to face Medications: Lasix, Aldactone, Lactulose, Methadone, Protonix, Lexapro NKDA SH: past IVDA, EtOH (stopped 1y ago), quit smoking FH: N/A PE: afebrile BP 126/46 P 95 RR20 O2 sat 96% 4LNC Gen: calm, comfortable, mild respiratory distress, mild jaundice HEENT: PERRLA, EOMI, anicteric Neck: supple, no JVD CV:S1, S2 regular rate and rhythm, no murmurs/gallops/rubs Lungs: ↓BS on R to mid-lung fields, on L to base Abd: soft, nontender, massively distended with gross ascites, + shifting dullness, + fluid wave Ext: b/l LE edema, chronic venous stasis changes Neuro: A/O x3, mild asterixis noted Labs: K 5.7, BUN/Cr 37/1.2, INR 1.95, AFP 3.6, NH3 74, AST/ALT 70/40 (nl<40), Tbili 4.7 (nl<1.5), Dbili 1.6 alkphos nl. Alb 2.2 (nl >3.4)