Ascites Management Guidelines for Liver Cirrhosis
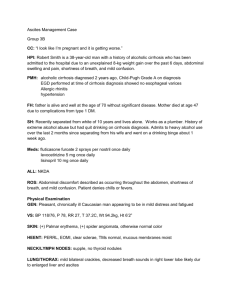
advertisement

This is an official Northern Trust policy and should not be edited in any way Ascites Management Guidelines for Liver Cirrhosis Reference Number: NHSCT/13/658 Target audience: These guidelines are relevant to medical and nursing staff working within Emergency Departments, Gastroenterology and Medical Admission Wards throughout the Trust. Sources of advice in relation to this document: Dr Gerard Rafferty, Consultant Replaces (if appropriate): N/A Type of Document: Directorate Specific Approved by: Policy, Standards and Guidelines Committee Date Approved: 4 March 2013 Date Issued by Policy Unit: 19 March 2013 NHSCT Mission Statement To provide for all the quality of services we would expect for our families and ourselves Ascites Management Guidelines for Liver Cirrhosis Authors: G. Jacob, G. Rafferty, P. Lynch, C. Rodgers, S. Ali, T. McLean. Produced: April 2011 Revised: February 2013 1 Ascites Management Guidelines for Liver Cirrhosis Introduction Ascites management guidelines for liver cirrhosis have been revised to ensure best practice guidance is followed with regard to patient diagnosis using a diagnostic tap and subsequent treatment/patient management. Aim To develop best practice guidance to improve ascites management in patients with liver cirrhosis. Target Audience These guidelines are relevant to medical and nursing staff working within Emergency Departments, Gastroenterology and Medical Admission Wards throughout the Trust. Dietetic staff working within the acute hospital setting also need to be aware of their role in providing dietary advice. Responsibilities It is the responsibility of all relevant staff (medical and nursing) to familiarise themselves with these guidelines and utilise them appropriately within their scope of practice. Dietitians are responsible for providing dietary advice, as appropriate Policy Statement/Actions Diagnostic Tap Diagnostic tap should be performed in all: 1. New onset Type 2 (moderate) or 3 (gross) ascites 2. Hospitalised patients for worsening ascites 3. Complications of cirrhosis such as encephalopathy, hepato-renal syndrome, variceal bleeding, sepsis. Diagnostic tap should be performed in above patients at time of decision to admit using aseptic non-touch technique (ANTT). This should be performed as soon as possible – ideally by medical admission team. Ultrasound (USS) marking not required. 20ml ascitic fluid aspirated using green needle and syringe and fluid is sent for: a) biochemistry (albumin - patients with cirrhosis will have transudate with a SAAG (Serum Ascites Albumin Gradient) of >11 g/L)) b) cytology c) haematology (WBC count) – urgent and chase result d) organisms (blood culture bottles) e) amylase if there is suspicion of pancreatic disease. 2 Large volume paracentesis (LVP) LVP does not require Ultrasound (USS) marking. Large volume ascites not responding to medical therapy or causing respiratory distress or discomfort should be managed by performing total abdominal paracentesis as follows: 1. Have patient empty bladder. 2. Position the patient in the bed with the head elevated 45-90 degrees. This allows fluid to accumulate in lower abdomen. 3. Put on sterile gloves. 4. Sterilize the site with iodine and then alcohol. 5. Place sterile draping towels 6. Inject Lignocaine 2% on to and including the peritoneum 7. A small nick is performed using a #11 scalpel 8. Introduce the catheter assembly of a ‘Bonnano’ catheter through the abdominal wall by using short thrusts at first obliquely up to peritoneum and perpendicularly to penetrate the peritoneum until resistance disappears. If you are in position, fluid should run free after removing the vent plug. 9. Disengage the needle from the catheter hub. Holding the needle to use it as a guide, advance catheter until the suture disc is flat against the skin. 10. Connect the adaptor clamp as directed and secure it by tape to the abdominal wall 11. Finally, connect the drainage bag to the catheter, emptying it as necessary. Observations are recorded every 15 minutes. If there is any evidence of hypotension, the drainage should immediately be stopped by clamping. Up to 10L can be safely drained in one attempt, but up to 22L have been reported to have been drained. Remove the drain after 6 hours or earlier if the fluid has stopped draining to prevent secondary infection. Seal the site with pressure bandage. Patient should lie on the opposite side if there is leakage of fluid and/or a purse string suture applied if necessary. Give 100 ml 20% Human Albumin Solution (HAS) for every 2-3L of ascitic fluid removed. This should ideally be started simultaneously at the beginning of paracentesis to prevent hypotension and hepatorenal syndrome. 3 Spontaneous Bacterial Peritonitis (SBP) An ascitic neutrophil count of >250 cells/mm3 is suggestive of SBP and broad spectrum antibiotics should be administered e.g. Tazocin. Antibiotic therapy should be commenced if there is clinical suspicion of infection even if neutrophil count is <250 cells/mm3. If raised creatinine or rising creatinine then consider IV Human Albumin Solution (Day 1: 1.5g albumin per kg and Day 3: 1g albumin per kg.) Medical Rx 1.Restrict sodium intake to 6g/day (Need dietitian to explain to patient) 2.Start Spironolactone 100mg/day. 3.If no response after 3 days, increase dose of Spironolactone stepwise to a daily dose of 400mg/day and add in Furosemide 40-160mg/day under Consultant/Associate Specialist supervision (monitor U&E daily). 4.Serum sodium 126-135mmol/L: Do not restrict fluids and continue diuretics 121-125mmol/L: a. with normal creatinine: BSG guidelines suggest stopping diuretics b. with high creatinine: stop diuretics and give volume expansion <120 – Stop diuretics and give colloids/0.9% sodium chloride (normal saline) 5. Chronic liver disease patients have high nutritional requirements (25-45 kcal per kg depending on compensated/decompensated and at least 1.2-2g protein per kg. Early assessment and intervention is key to improving outcomes in this group. MUST is unhelpful due to inaccuracy of weight in this patient group. Protein energy malnutrition is common. Other options: • • Transjugular intrahepatic portosystemic shunt (TIPS) Liver transplant Equality, Human Rights and DDA This policy has been drawn up and reviewed in the light of Section 75 of the Northern Ireland Act (1998) which requires the Trust to have due regard to the need to promote equality of opportunity. It has been screened to identify any adverse impact on the 9 equality categories and no significant differential impacts were identified, therefore, an Equality Impact Assessment is not required. Alternative Formats This document can be made available on request on disc, larger font, Braille, audio-cassette and in other minority languages to meet the needs of those who are not fluent in English. 4 Sources of Advice in relation to this document The Policy Author, responsible Assistant Director or Director as detailed on the policy title page should be contacted with regard to any queries on the content of this policy. References: 1. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. Journal of Hepatology 2010 vol. 53 j 397–417. 2. BSG Guidelines on the management of ascites in cirrhosis. Gut 2006; 55; 112. 5