Case
advertisement

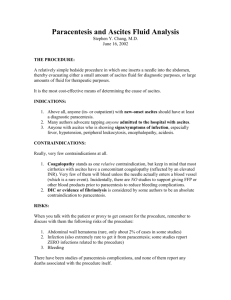
Cirrhosis Management – A Case Based Approach to Disease Management Brenda Appolo PAC, MHS University of Pennsylvania, Perelman School of Medicine Causes of Cirrhosis Hepatitis C Alcohol Hepatitis B Hemochromatosis Wilson’s Disease Alpha-1-Antitrypsin Deficiency • DILI • • • • • • • Primary Biliary Cirrhosis • Autoimmune chronic hepatitis • Primary Sclerosing Cholangitis • Cryptogenic • Non-Alcoholic Steatohepatitis Case • Carl is a 56 M presents to ED with hematemesis • PMHx: – HCV infection dx years prior but IFN unwilling – HTN • SHx: – Blood transfusion age – 2 six packs beer per week; former TOB user; married; FT worker • Exam: – BP 90/60; HR 100; BMI 31; No icterus on exam; Abdomen soft; splenomegaly; +1 pedal edema • Labs – Hg 8.0; Hct 25%; 89k; WBC 7.1 – Glu 136; cr 0.57; AlkPhos 114; T bil 1.4; AST 66; ALT 46; INR 1.3 Portal Hypertensive Bleeding Esophgaeal Varices Gastric Varices Portal Hypertensive Gastropathy Colopathy / Rectal Varices band ligation s/p ligation at 4' bleeding stopped w ethanolamine bleeding stopped w ethanolamine Risk of Esophageal Varices Bleed 35-80 % 25-40 % Cirrhosis 50-70 % Survive Rebleed 70 % 30-50 % Die Esophago-Gastric Varices • Screening and follow up • Primary Prophylaxis Varices diagnosed and what do we do? • Secondary Prophylaxis Varices bled and what do we do to prevent rebleeding? Cirrhosis Upper Endoscopy Small varices (< 5 mm), Child B/C,red wales No varices Repeat Endoscopy in 3 years (well compensated); in 1 year if decompensated NO beta-blocker prophylaxis Non-selective betablocker prophylaxis Titrate to HR of 55-60 Medium or large varices Child Class A,no red wales-beta blockers Child class B/C,red wales-beta blockers OR band ligation If prophylaxis not used-repeat endoscopy in 1-2 years Gacia-Tsao et al Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis AASLD Practice Guideline: Hepatology 2007;46:922-38 Mechanisms of Action of Various Therapies for Varices Treatment Flow Vasoconstrictors (e.g.-blockers) Venodilators (nitrates) Vasoconstrictors + venodilators Endoscopic Therapy TIPS/Shunt Surgery ? Resistance Portal Pressure Case – continued (Carl) • Carl undergoes serial EGD to obliterate varices; placed on beta blocker • Remains IFN unwilling; stopped alcohol • 2 years later presents with increased abdominal girth and dyspnea; wife is concerned about his fatigue and odd behavior this AM • Presents to ED; no imaging on file x 1 yr • Exam – – BP 90/60; HR 62; Weigh > 20lbs since last ED visit; + tense abd; alert and oriented Ascites - SBP Ascites in Cirrhosis : Diagnosis • Physical Exam/Ultrasound: – 1.5 - 3 liters: Shifting dullness – 10 liters: fluid wave • Paracentesis (1% hematoma) – No need for FFP or Platelet transfusion – Helps in differential diagnosis – 20% prevalence of infection at admission – Indication: new onset; admitted to hospital with or without symptoms of abdominal pain, fevers, etc; those who deteriorate during hospitalization Management of Ascites First Line Therapy Second Line Therapy Tense ascites Refractory Ascites 10 % • Repeated Large volume paracentesis (LVP) •TIPS Paracentesis • Liver Transplantation Sodim restriction ( 2 Gm/24 Hrs) and diuretics •Post paracentesis albumin infusion may not be necessary for < 5 liters removed Non-tense ascites •Diuretics: Spironolactone 100 mg/day, furosemide 40 mg/day or bumetanide 1 mg a day. •Uptitrate stepwise to spironolactone 400 mg/day, furosemide 160 mg/day or bumetanide 4 mg/day as long as it is tolerated • Albumin infusion of 6-8 gm/liter of fluid removed is a consideration for repeated LVP Etiology of Ascites Congestive Heart Failure Tuberculosis Other Malignancy Cirrhosis 5% Mixed 100 80 Survival 60 (%) 40 20 1 Onset 2 3 Years 4 5 6 Ascites Survival: Only improved by liver transplant 100 80 After Liver Transplant Survival 60 (%) 40 20 1 Onset 2 3 Years 4 5 6 Ascitic Fluid Analysis ROUTINE OPTIONAL Cell count Glucose TB smear/culture LDH Cytology Albumin Gram Stain Culture (blood-cultures) Total Protein Amylase UNUSUAL Ascitic Fluid Infection • Spontaneous bacterial peritonitis • Monomicrobial non-neutrocytic bacterascites • Culture-negative neutrocytic ascites Spontaneous Bacterial Peritonitis • PMN count > 250 cells/mL • Positive ascites culture • No evidence of intra-abdominal source requiring surgery Secondary Bacterial Peritonitis • PMN count > 250 cells/mL – (total WBC usually > 10,000) – Total Protein > 1 g/dL, elevated LDH, glucose < 50 mg/dL ( 2 of 3 features) • Positive ascites culture – (usually multiple organisms) • Ascites CEA > 5 ng/ml, Alkaline Phophatase > 240 U/L helpful is identifying intra-abdominal surgically treatable primary source of infection Overview of Hepatic Encephalopathy • Encompasses a wide spectrum of neuropsychiatric abnormalities in patients with liver dysfunction • Characterized by – Disturbances in consciousness – Changes in personality and intellectual capacity – High blood ammonia (NH3) levels – Altered neuromuscular activity – EEG abnormalities EEG = electroencephalogram. Abou-Assi et al. Postgrad Med. 2001;109:52-70. Ferenci et al. Hepatology. 2002;35:716-721. Mas et al. J Hepatol. 2003;38:51-58. Treatment Options for HE • Reduction in the nitrogenous load arising from the gut – Bowel cleansing – Nonabsorbable disaccharides (lactulose) – Antibiotics (rifaximin, neomycin, metronidazole) • Drugs that affect neurotransmission (flumazenil, bromocriptine) • Manipulation of the splanchnic circulation (occlusion of portal-systemic collaterals) HE = hepatic encephalopathy. Blei et al. Am J Gastroenterol. 2001;96:1968-1976. Transjugular Intrahepatic Portosystemic Shunt and Surgical Shunts Placement of TIPS Catheter Inferior vena cava Hepatic veins TIPS Left gastric vein Portal vein Superior mesenteric vein Inferior mesenteric vein Indications and Efficacy of TIPS Efficacy Effective Mortality Secondary prevention of Variceal Bleeding Yes No Effect Refractory Cirrhotic Ascites Yes No Effect Efficacy in Absence of Another Therapy Effective Refractory Acutely Bleeding Varices Yes Portal Hypertensive Gastropathy Yes Gastric Antral Vascular Ectasia No Refractory Hepatic Hydrothorax Yes Budd Chiari Syndrome Yes Veno-Occlusive Disease No Etiology of Hepatocellular Carcinoma in the US Other HBV 4% 6% Cryptogenic Alcohol 10 % 12 % 29 % 39 % Marrero JA Hepatology 36;1349-54:2002 HCV + Alcohol HCV Screening for Hepatocellular Carcinoma (HCC) Screening is done with AFP and ultrasound every 6-12 months • All patients with cirrhosis • Hepatitis B - Africans > 20 years - Asian women > 50 years, men > 40 years - Family H/O HCC Guidelines for Diagnosis of HCC Ultrasound findings < 1 cm 1-2 cm > 2 cm Repeat US every 3-6 mo Dynamic CT, contrast US or MRI Dynamic CT, contrast US or MRI 2 tests 1 test Typical = HCC Typical = HCC Atypical = biopsy Atypical = biopsy Typical features of HCC = vascular nodule on arterial phase with washout in delayed phases Bruix J, et al. Hepatology 2005 Current Treatment Options for HCC Surgical • Hepatic Resection • Liver Transplantation Non-surgical • Transarterial Chemoembolization(TACE) • Ablation Therapy (RFA, PEI) •Molecular targeted therapy • Gene Therapy Liver Transplantation for HCC Milan Criteria 1 lesion ≤5 cm 3 or less lesions, none >3 cm + Absence of Macroscopic Vascular Invasion Absence of Extra-hepatic Spread Mazzaferro V, et al. N Engl J Med 1996;334:693–699. Treatment of HCC Surgical Resection vs. OLT vs. Ablation 1 yr 5 yr • Resection – Survival 74–96% 25–72% • Liver Transplantation – Survival 84–90% 69–75% • Ablation (PEI) – Survival 87–98% 29–54% Summary: Complication of Cirrhosis • • • • • Varices Ascites / Refractory Ascites Hepatic Encephalopathy Hepatocellular Carcinoma Synthetic Dysfunction (jaundice, coagulopathy)