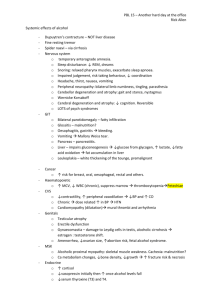
Types of gallbladder disease
advertisement

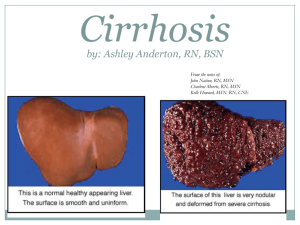
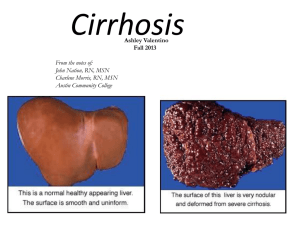
Liver Cirrhosis Defined anatomically as a diffuse process with fibrosis and nodule formation. Child –Turcotte-Pugh classification Clinical parameter 1 --to access severity. 2 3 Bilirubin(mg/dl) <2 2-3 >3 Albumin (g/dl) > 3.5 Ascites None Encephalopathy(grade) None 1-2 3-4 PT (sec prolonged) <4 4-6 >6 OR INR < 1.7 1.7 - 2.3 > 2.3 Prognosis Good 2.8 - 3.5 Easily controlled < 2.8 Poorly controlled Fair poor Class A => 5 - 6, B = >7 - 9, C = >10-15 Symptoms:fatigue, weight loss, anorexia, leg swelling, hemorrhage (nose, gum, GI tract), any Hx of jaundice, hepatitis, drug ingested, blood transfusion in the past and alcohol consumption. Signs 1. Skinvascular spider, purpura, 2. Eyejaundice, K-F ring, anemia 3. Bodygynaecomastia, testicular atrophy, distribution of body hair. 4. ExtremitiesDupuytren’s contracture, palmar erythema, nail changes (clubbing, white nails), peripheral edema. 5. Abdomenascites, dilated veins, liver, spleen enlargement. 6. Neurohepatic encephalopathy, fetor hepaticus, flapping tremor. Diagnosis 1. Anemia (microcystic due to blood loss, macrocystic due to folate deficiency), pancytopenic ( hypersplenism), prolong PT (INR) 2. Biochemistry- elevated Bilirubin, GOT/GPT, ALK-P, reversed AG ratio, low immunoglobulin, hyponatremia, hypokalemic alkalosis. 3. Etiology ; HBV, HCV marker, AFP, smooth muscle, mitochordrial and nuclear antibodies, ceruloplasmin, α1 antitrypsin 4. Endoscopy.(for EV) 5. Hepatic echo , CT 6. Definitive diagnosisliver biopsy. Prognosis factors 1. Aetiology ( alcohol is best) 2. Decompensation due to hemorrhage, infection and alcohol, better. 3. The response to therapy. 4. Jaundice ( esp; persistent) 5. Neurological complication 6. Liver size (large liver better- more functioning cells) 7. Portal venous pressure 8. EV bleeding 9. Biochemical test ( albumin< 2.5, Na+ < 120, ) 10. Persistent hypotension ( SBP < 100) 11. Hepatic histological change Major Complication of Cirrhosis • Portal hypertension ( < 60% of patients, > 10 mmHg) presenting as variceal bleeding, hypersplenism • • • • • • Ascites Hepatic encephalopathy Spontaneous bacterial peritonitis Hepatorenal syndrome Hepatopulmonary syndrome Hepatocellular carcinoma Ascites Accumulation of fluid within the peritoneal cavity. Symptoms:distended abdomen, fullness sensation, and other symptoms of cirrhosis (above). Signs:protruded abdomen, fluid thrill, associated with scrotal edema, umbilical or inguinal herniation, pleural effusion esp; at RT side ( hepatic hydrothorax) and other signs of cirrhosis (above). Laboratory: check serum Na+, K+, HCO3─, CL─, urea, creatine, 24 hr urine volume and Na+ excretion. Diagnostic paracentesis: protein, albumin, glucose, cell count and differential, culture, cytology. In selected case may need to check amylase, LDH, triglycerides, TB culture. Treatment 1. General Measurement of Ascites • • • • • • Education for dietary salt ( 2Gm/d = 88mmol/d ) Fluid restriction of 1- 1.5L if hyponatremia. Bed rest Check serum - urinary electrolyte and renal function. Weigh daily, Measure urinary volume. • Sample ascites • Spironolactone 100-200 mg/day • After 4 days consider to add furosemide 40 g/d (100mg: 40 mg ratio) to Mx400mg: 160 mg, ** check electrolyte. • Stop diuretic if pre-coma (flap) akalosis, azotemia or decrease K+ • Continue monitor weight, increase diuretics as necessary. • Albumin supply 2. Tense ascites Large volume paracentesis and supply I.V salt poor albumin- 6-8 gm/L removed ascites. Patient selection: Child’s B, PT – normal, Platelets > 40x103/mm3, Serum creatinine < 3 mg/dl, urinary Na + > 10 mmol/d 3. Refractory ascites Serial therapeutic paracentesis, TIPS, peritoneovenous shunt and liver transplant. Goal of Treatment • To increase urinary excretion of Na + > 80mmol/d • Random spot urine Na + concentration is > K + concentration can correlates with a 24 hr Na + excretion > 78 mmol/d with approximately 90% accuracy. Spontaneous Bacterial Peritonitis -Suspect Grade B and C cirrhosis with ascites. -Clinical feature may be absent and WBC may be normal. -Ascites protein usually < 1 g/dl. -Others ; sudden rise of fever, chill, generalizes abdominal pain with rebound tenderness and progress of hepatic encephalopathy. Diagnosis Ascites fluid neutrophil count > 250 /mm3 Positive blood culture(E-coli, pneumococcus, streptococcus, Klebsiella) Treatment -Cefotaxime 2 G q 8H 5 days followed by more narrow spectrum therapy after susceptibility results are available. -Prophylaxis with Norfloxacin 400 mg PO qd 5 days a week or Cipro 50 mg PO once a week. Hepatic Encephalopathy A state of disordered CNS function associated with severe acute or chronic liver disease; may be acute and reversible or chronic and progressive. Clinical features Stage 1: euphoria or depression, slurred speech, disordered sleep, asterixis (flapping tremor), mild confusion. Stage 2: lethargy, moderate confusion. Stage 3: marked confusion, sleeping but arousable, inarticulate speech. Stage 4: coma. Differential diagnosis : 1. Alcohol related (intoxication, withdrawl) 2. Drug toxicity (sedatives or psychoactive drugs) 3. Infections ( sepsis, meningitis, encephalitis) 4. Intracranial lesions ( CVA, abscess, tumor) 5. Metabolic ( DKA, electrolyte imbalance, hypoglycemia, uremia) 6. Neuropsychiatric disorders Factors That May precipitate Hepatic Encephalopathy in Cirrhosis Nitrogenous Encephalopathy Non-nitrogenou Encephalopathy 1. 2. 3. 4. 5. 6. 7. 8. Uremia/azotemia GI bleeding Dehydration Metabolic alkalosis Hypokalemia Constipation Excessive dietary protein Infection 1. 2. 3. 4. 5. Sedatives, benzodiazepines Barbituates Hypoxia, hypoglycemia Hypothyroidism Anemia Treatment of Hepatic Encephalopathy 1. Identify and correct the precipitating causes a. Access volume statue and vital sign b. Evaluate GI bleeding c. Eliminate sedatives. tranquilizers or similar drugs d. Perform screening test for hypoxia., hypoglycemia, anemia, hypokalemia, and other possible metabolic or endocrine factors and correct as indicated. 2. Initiate ammonia –lowering therapy a. NG lavage, b. lactulose enema—100 ml in water or N/S 100 – 200 ml (retension enema) oral—20 – 40 ml qid (at least 2 - 4 bowel movement/day) c. Minimize or eliminate dietary protein d. Oral non –absorbable antibiotic to reduce intestinal bacterial counts. - Neomycin (1 – 3 g /day) or Metronidazole (250 mg qid/day) e. Consider flumazenil or other benzodiazepine receptor antagonist 3. Minimize the potential complications of cirrhosis and depressed consciousness a. Provide supportive care with protect airway, hemodynamic and metabolic status. Hepatorenal syndrome A progressive functional renal failure that occurs in patients with severe liver disease. Clinical features worsening azotemia, hyponatremia, progressive oliguria with urinary Na + concentration < 10 mmol/L, hypotension which lack of response to volume challenge. Precipitating factors GI bleeding, excessive diuresis, paracentesis, or drugs (NSAID, ACEI, aminoglycosides). Treatment 1. Effective liver transplantation. 2. Symptomatic correct underlying or precipitating factors as much as possible. (Volume challenge, stop NSAID). Hepatocellular carcinoma An epithelial tumor arising from malignant transformation of the hepatocyte. It is the most common primary malignancy of the liver. Symptoms: abdominal pain, weight loss, abdominal swelling, weakness, jaundice. Signs: hepatomegaly, splenomegaly, hepatic bruit, ascites, jaundice. Laboratory: usually reflect with underlying chronic liver disease, raised Alk-P and AFP. Imaging: Abdominal US, CT, MRI, angiography, laparoscopy, biopsy. Risk factors 1. Major chronic HBV and HCV infection, cirrhosis, aflatoxin B. 2. Minor OC pills, smoking, Wilson’s disease, hemochromatosis, α1 antitrypsin deficiency. Treatment: Choice of a particular therapy must be individualized because no single therapy has emerged as a treatment of choice. 1. 2. 3. 4. Surgery (offers best chance of cure) Liver transplantation TAE ( trans arterial embolization) US-guided PEI (percutaneous ethanol injection), PAI (percutaneous acetic acid injection) and RFA (radiofrequency ablation). 5. Chemotherapy. 6. Radiation