Presentation 1
advertisement

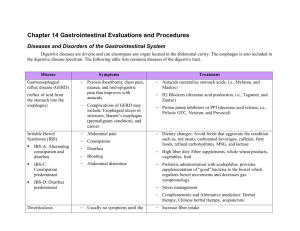
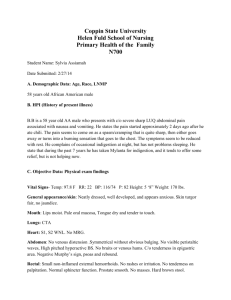
Richard C. Walls Pharmacy 551—Case Presentation #1 General Patient Information: KV is a 60 year old female admitted to UMHS on 2013-01-31. Chief Complaint: Abdominal pain accompanied by nausea, vomiting, skin discoloration, and abdominal distension. HPI: The patient has not been feeling well for the past month and reported nausea, vomiting, and skin discoloration. She had a hospital stay from 01-21 to 01-23 that identified ascites via ultrasound, but no further diagnostics were performed and she was discharged. Her symptoms continued to worsen over the following week and were not effectively managed by a trip to the Grand Rapids ER and she was told to come to Ann Arbor. Her clinical picture has stabilized with administration of IV fluids and the patient is preparing for discharge to return to home care PMH: Non-alcoholic steatohepatitis cirrhosis (being evaluated for transplant and close to listing) Gastric varices Ascites Myelodysplastic syndrome s/p bone marrow transplant (1990) w/complications of GVHD and dry eyes COPD History of CMV infection SH: No tobacco, remote and inactive drinking, no illicit drugs, lives with husband FH: Cancer in father, mother, brother, and sisters (one with SCLC and one with sarcoma). Medication History: Cirrhosis: MDS: COPD: Unknown: Allergies: Lasix Spironolactone Nadolol (prophylaxis of variceal bleeding) Omeprazole Lactulose Short acting morphine 15 mg q4h (patient has stopped taking) Zofran 4 mg PRN Artificial Tears Albuterol Advair Atrovent Gabapentin 100 mg TID Codeine, erythromycin, and morphine all cause nausea ROS: Negative excepting NV, abdominal pain and ascites Physical Exam: 5’6” 77.6 kg obese female Temp 36.7; HR 77; RR 20; BP 100/51; O2 Sat: 97% General physical findings show no appreciable disease, and are markedly improved from admission. Regular rate and rhythm cardiac Abdominal pain remains but does not show rebound or guarding. Patient is alert and oriented x3 with no signs of hepatic encephalopathy. Laboratory Findings: Na K Cl CO2 Ca++ Phos Mg++ BUN SCr CrCl Glucose 135 4.3 104 24 9.3 2.1 (low) 1.6 20 1.1 56.9 88 WBC Plt Hbg HCT MCV RDW 7.8 107 10.7 (low) 28.5 (low) 95.6 20.3 (high) TProtein Albumin AST ALT ALK TBili 5.6 (low) 2.0 (low) 203 (high) 77 (high) 238 (high) 6.3 (high) INR 1.6 Problem List: 1—Abdominal pain Has improved markedly since admission but patient still complains of moderate pressure-like pain in her abdomen. This pain has coincided with nausea, vomiting, and gas. The origin of these symptoms is unclear and ascites are not severe enough to perform diagnostics for possible SBP and an esophagastroduodenoscopy is scheduled. Symptomatic treatment with ondansetron and prochlorperazine as needed have been effective at managing these symptoms to date and I recommend continuing them until a diagnosis can be made. Goal: Resolution of nausea, vomiting, and abdominal pain Recommendation: Continue prn use of ondansetron 4 mg IV q6h and prochlorperazine 10 mg po q6hh until a cause of the symptoms can be identified. Continue omeprazole 20 mg po daily. Switch patient to a bland diet. Continue IV fluid replacement. Counsel patient to eat a low sodium diet and keep fluids <2 L as outpatient to minimize fluid accumulation. Monitoring: Worsening of ascites, frequency of nausea and vomiting, level and frequency of abdominal pain 2—NASH Cirrhosis Patient’s cirrhosis has decompensated and may be involved in patient’s chief complaint. Liver enzymes are high as is total bilirubin, and total protein and albumin are both low. Diagnostics have shown a new portal vein thrombus, but hepatic team does not recommend systemic anti-coagulation. Patient is undergoing transplant evaluation and is only waiting for clearance from her bone marrow transplant physician to be listed for transplant. Goal: Reduction of ascites, prevention of hepatic encephalopathy, prevention of variceal bleeding Recommendation: Continue nadolol 40 mg po daily and omeprazole 20 mg po daily. Agree with physician’s recommendation to increase lactulose to 4x/day to achieve 2 bowel movements a day and that this dose should be continued outpatient. Monitoring Parameters: Mental status changes, albumin, AST, ALT, ALK, bilirubin, INR, ammonia, HR, frequency of bowel movements 3—Acute Kidney Injury Patient’s creatinine was elevated on admission (1.6 compared to a baseline of 0.7) but has been stabilizing with administration of IV fluids. Her SCr is currently 1.1 with a CrCl of 56.9. Injury is likely pre-renal caused by hypovolemia secondary to vomiting and third spacing of fluid. Goal: Return of kidney function to normal, minimize the impact of currently poor renal function on the patient Recommendation: Continue IV fluids and consider albumin if kidney function does not improve on fluids alone or ascites worsen. Continue to hold Lasix and spironolactone until kidney injury resolves to ensure adequate perfusion. Doses of current medications do not necessitate renal adjustment at this time. Monitoring Parameters: BUN, SCr, Is/Os, Na+, K+, CO2, Ca++, Phos 4—Medications without Indication Neither gabapentin nor morphine sulfate have a clear indication. Patient has stopped taking morphine and this seems reasonable given that the pain she’s currently experiencing is probably better suited by managing GI issues and actual causes and morphine could exacerbate the patient’s nausea. Gabapentin has no clear indication and is being prescribed at a very low dose. Given that common side effects of gabapentin such as edema, NV, and mental status changes are all of special concern in this cirrhotic patient, I recommend investigating the necessity of this agent and likely discontinuing it. Goal: Reduction of pill burden, reduction of exposure to unnecessary adverse events Recommendation: Formally discontinue morphine sulfate and investigate the use of gabapentin to see if it is necessary for the patient. Summary: KV is a 60 yo F who presented to UMHS with abdominal pain along with nausea, vomiting, abdominal distension and AKI all of which have improved markedly since admission. Going forward, the patient’s cirrhosis is likely the patient’s biggest concern, and transplant seems necessary at this stage.
![[Physician Letterhead] [Select Today`s Date] . [Name of Health](http://s3.studylib.net/store/data/006995683_1-fc7d457c4956a00b3a5595efa89b67b0-300x300.png)