Discharge Summary 2
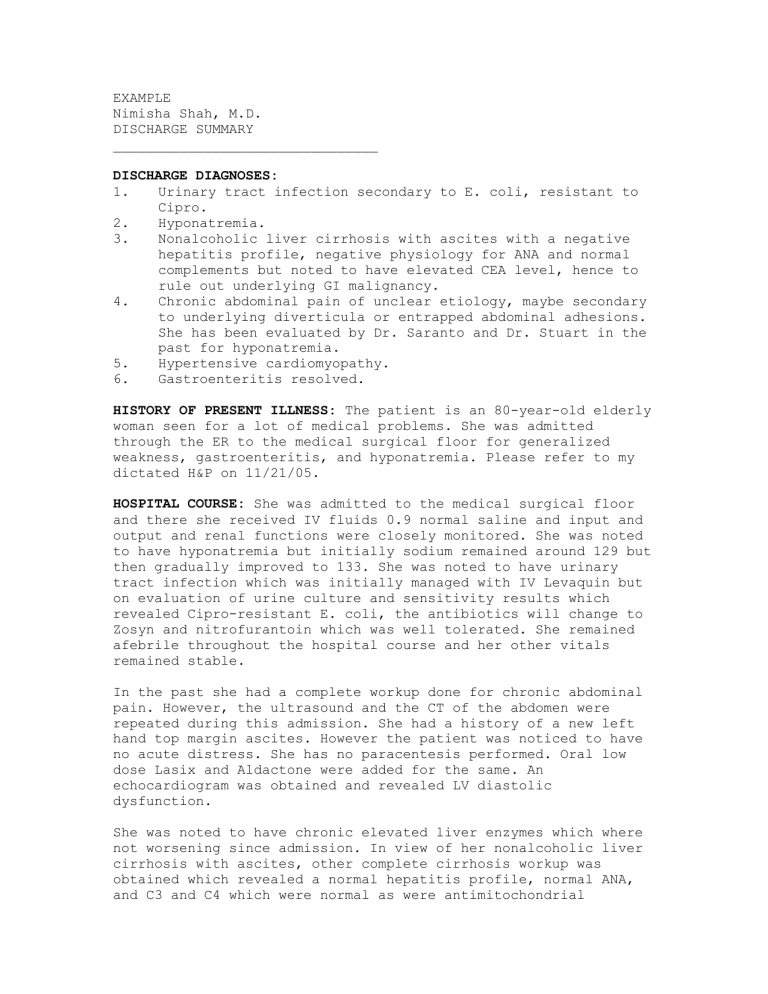
EXAMPLE
Nimisha Shah, M.D.
DISCHARGE SUMMARY
________________________________
DISCHARGE DIAGNOSES:
1. Urinary tract infection secondary to E. coli, resistant to
Cipro.
2. Hyponatremia.
3. Nonalcoholic liver cirrhosis with ascites with a negative hepatitis profile, negative physiology for ANA and normal complements but noted to have elevated CEA level, hence to rule out underlying GI malignancy.
4. Chronic abdominal pain of unclear etiology, maybe secondary to underlying diverticula or entrapped abdominal adhesions.
She has been evaluated by Dr. Saranto and Dr. Stuart in the past for hyponatremia.
5. Hypertensive cardiomyopathy.
6. Gastroenteritis resolved.
HISTORY OF PRESENT ILLNESS: The patient is an 80-year-old elderly woman seen for a lot of medical problems. She was admitted through the ER to the medical surgical floor for generalized weakness, gastroenteritis, and hyponatremia. Please refer to my dictated H&P on 11/21/05.
HOSPITAL COURSE: She was admitted to the medical surgical floor and there she received IV fluids 0.9 normal saline and input and output and renal functions were closely monitored. She was noted to have hyponatremia but initially sodium remained around 129 but then gradually improved to 133. She was noted to have urinary tract infection which was initially managed with IV Levaquin but on evaluation of urine culture and sensitivity results which revealed Cipro-resistant E. coli, the antibiotics will change to
Zosyn and nitrofurantoin which was well tolerated. She remained afebrile throughout the hospital course and her other vitals remained stable.
In the past she had a complete workup done for chronic abdominal pain. However, the ultrasound and the CT of the abdomen were repeated during this admission. She had a history of a new left hand top margin ascites. However the patient was noticed to have no acute distress. She has no paracentesis performed. Oral low dose Lasix and Aldactone were added for the same. An echocardiogram was obtained and revealed LV diastolic dysfunction.
She was noted to have chronic elevated liver enzymes which where not worsening since admission. In view of her nonalcoholic liver cirrhosis with ascites, other complete cirrhosis workup was obtained which revealed a normal hepatitis profile, normal ANA, and C3 and C4 which were normal as were antimitochondrial
antibody and alpha-fetoprotein but the CEA levels were elevated.
Hence, we are waiting for GI consult to repeat endoscopy to rule out underlying VI malignancy. The patient was still noted to have mildly reduced endurance, needing physical therapy, occupational therapy and IV antibiotics and she was considered a candidate for
TLC.
Her condition at the time of transfer was stable.
INSTRUCTIONS ON TRANSFER TO TLC:
1. Transfer to TLC on cardiac hepatic diet.
2. Physical therapy and occupational therapy evaluations.
3. Amiodarone 200 mg 1 p.o. b.i.d.
4. Protonix, 40 mg 1 p.o. daily
5. Diovan 80 mg 1 p.o. daily
6. Lasix 20 mg p.o. daily
7. Aldactone 25 mg 1 p.o. b.i.d.
8. Synthroid 112 mcg 1 p.o. t.i.d.
9. Multivitamin 1 p.o. daily
10. Nitrofurantoin 100 mg 1 p.o. b.i.d.
11. Zosyn 3.375 gm IV every 6 hours
12. Reglan 10 mg p.o. t.i.d. as needed
13. IV fluids, D5 half-normal saline at 30 mL per hour
14. Tylenol p.r.n.
15. Repeat CMP and CBC on December 1, 2005 and twice a week.
16. GI consultation with Dr. Stuart requested.