Document
advertisement

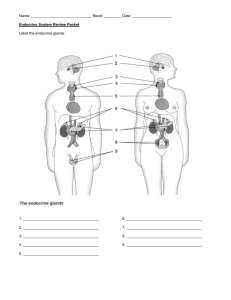
Unit 9 Endocrine System Session 32 Introduction to the Endocrine System Session Outline Introduction 32.1 Organs of the endocrine system 32.2 Features of hormones 32.3 Types of hormones and their modes of action 32.4 Stimulation of hormone secretion Summary Learning Outcomes Introduction The physiological activities of the body are maintained only if the internal environment of the body is kept constant. This is maintained only with the help of two major regulating systems in the body. They are the endocrine system and the nervous system. Compared with other organs of the body, the endocrine organs are small. Endocrine organs are widely scattered throughout the body. Endocrine glands are also called ductless glands as they produce hormones and release it to the blood stream without ducts. They release their hormones into the surrounding tissue fluid or the blood (endo = within; crine = to secrete). The endocrine organ generally has a rich vascular and lymphatic drainage that receives the secreted hormones. Homeostasis (constancy) of the internal environment is maintained by two systems. They are the endocrine system and the autonomic nervous system. The autonomic nervous system brings about very rapid changes, while the endocrine system brings about slow and more precise changes The endocrine system, interacts with the nervous system to coordinate and integrate the activity of body cells. The endocrine system influences the metabolic activities of the body by secretions known as hormones . (The word ‘hormone’ is known to have the meaning ‘to excite’ in Greek). Hormones are secreted by several glands of the body. 1 32.1 Organs of the Endocrine system There are many organs and tissues associated with endocrine function. The hypothalamus is associated with endocrine function and is also a major regulator of the pituitary gland. Hence it will be discussed with the pituitary gland in the next session. The major endocrine organs and their secretions are listed in the table below Endocrine organ Pituitary gland Thyroid gland Hormones secreted Growth hormone, Thyroid Stimulating hormone, Adreno cortico tropic hormone. Follicular stimulating Hormone, Leutinizing hormone, Prolactin, Thyroxine, tri iodo thyronine parathyroid glands Parathormone adrenal (suprarenal) glands pancreatic islets (islets of Langerhans) pineal gland or body thymus gland ovaries in the female testes in the male. Gastro intestinal tract hormone Epinephrine, nor epinephrine, o Insulin, glucogon, sommatostatin. Melatonin Oestrogen, progesterone, testosterone Gastrin, cholecystokinin pancreozymin, secretin These organs are all shown in the diagram below. Figure 32.1 2 Figure 32.1 Endocrine organs of the body 32.1 Self Assessment Questions Can you explain the importance of the endocrine system Can you list the organs of the endocrine system? Can you list the hormones secreted by each endocrine glandsf 32.2 Features of Hormones Hormones are chemical messengers. They have several features. They are briefly explained below. • Hormones are released into the blood and are transported throughout the body. Hormones which are released into the blood have their action in a site away from the point of secretion. Endocrine glands consist of a group of secretory cells surrounded by capillaries. • • At various tissues where the hormones act, the target cells contain specific hormone binding sites within its cellular organelles. When a hormone binds to a hormone binding site in a cell, it stimulates specific responses in a cell. These initiated responses can go on for a few seconds to even days. Therefore the responses activated by the endocrine system are much slower in action. The actions of hormones continue to go on for a prolonged period than those activated by the nervous system. 3 • 32.2 • • Can you briefly outline the main functions of hormones? What are the retroperitoneal organs in the body ? Self Assessment Questions 32.3 Types of hormones and their modes of action There are several types of hormones and they are steroids, peptides and amino acids. Steroid hormones are cortisol, aldosterone and testosterone. Parathormone and insulin are peptides and thyroxine is an amino acid. When hormones reach the target cell via the blood circulation it will only act on cells which have receptors to bind the hormone. Therefore when a hormone reaches a target cell it binds to the hormone receptor. Hormone binding receptors are located in three major sites in a cell. These binding sites are the cell membrane, the cytoplasm and the nucleus. When the hormone binds to the receptor it stimulates a specific physiological action in the target cell. The hormones stimulate several physiological mechanisms within the cell. These are listed below. A hormonal stimulus typically produces one or more of the following changes: 1. Alters the permeability of the cell membrane or the potential of the cell membrane, or both, by opening or closing ion channels 2. Stimulates synthesis of proteins or regulatory molecules such as enzymes within the cell 3. Activates or deactivates enzymes 4. stimulates secretory activity 5. Stimulates mitosis by activating genes The endocrine glands include the pituitary, thyroid, parathyroid, adrenal, pineal, and thymus glands. The hypothalamus, along with its neural functions, produces and releases hormones, so we can consider the hypothalamus as a neuroendocrine organ. In addition, several organs contain specific areas of endocrine tissue and produce hormones as well as exocrine products. Such organs, (eg pancreas, gonads (ovaries and testes)), are also major endocrine glands. 32.3 Self Assessment Questions Can you list the changes that occur in a cell when it is stimulated by a hormone? Stimulation of hormone secretion: Secretion of hormones can be stimulated by three main mechanisms. They are the humoral stimulus, the neural stimulus, and the hormonal stimulus. They are outlined below. 4 (a) Humoral stimulus: Low blood calcium levels triggers the parathyroid glands. The parathyroid gland releases parathyroid hormone. This hormone causes blood Ca2+ levels to rise by stimulating release of Ca2+ from bone (Figure 32.2). In this case the humoral substance is Ca2+. Figure 32.2 Release of hormones by humoral stimulus (b) Neural stimulus: Stimulation by nerve fibers can trigger the release of hormones. As an example when the sympathetic nervous system fibers stimulate the adrenal medullary cells it stimulates the release of catecholamines ( epinephrine and norepinephrine) into the blood ( figure 32.3). 5 Figure 32.3 Release of hormones by neural stimulus (c) Hormonal stimulus: In this method of hormone release a hormone from one endocrine organ stimulates the release of several hormones from several target organs. As an example, hormones released by the hypothalamus stimulate the anterior pituitary to release hormones that stimulate other endocrine organs to secrete hormones (figure 32.4) Figure 32.3 Release of hormones by hormonal stimulus The synthesis and secretion of most hormones are controlled by the hypothalamus and / or the anterior pituitary gland. Therefore the next session will first discuss the hypothalamus and the pituitary gland. 32.4 Self Assessment Questions List the stimuli that activate the secretion of a hormone Can you list an example for each type of secretion? 6 Positive feed back mechanism and negative feed back inhibition- Regulation of secretion of hormones The hormones released by the hypothalamus, pituitary and the target endocrine organ are regulated by negative and positive feed back mechanisms. That is hormones from the hypothalamus may stimulate or may inhibit the secretions from the anterior pituitary gland. The anterior pituitary gland secretes tropic hormones which stimulate the target endocrine glands. Hormones secreted by the target endocrine gland may in turn inhibit the secretions from the anterior pituitary gland and this is called negative feedback mechanism. When hormones from the target organs further stimulate the pituitary gland to secrete even further it is called a positive feed back mechanism. Hormonal rhythms Most endocrine secretions occur in rhythms. When these rhythms of secretion are timed within a 24 hour cycle it is known as a circadian (or diurnal) rhythm. Some of the circadian rhythms known are the sleep wake cycle to time with day and night time, and the secretion of cortisol in the body. 32.5 Self Assessment Questions What is meant by hormonal rhythms? What is the link between the hypothalamus and the pituitary? Can you explain a positive feed back mechanism and a negative feed back mechanism with mples? Summary In this session you learnt about the importance of endocrine glands and their secretions in maintaining homeostasis. Hormones are released into the blood and are transported throughout the body. They have their action in a site away from the point of secretion. Therefore endocrine glands consist of a group of secretory cells surrounded by a rich net work of capillaries. The tissues where a hormone acts is known as the target cell. Target cells contain specific hormone binding sites within its cell. When a hormone binds to a hormone binding site in a cell, it stimulates specific responses in a cell. These stimulated responses can last only for a few seconds or go on for even days. The responses activated by the endocrine system are much slower in action than nervous responses. A hormonal stimulus typically produces several changes in the cell. They alter the permeability of the cell membrane or the potential of the cell membrane, stimulate synthesisof proteins or enzymes, activates or deactivates enzymes, stimulate secretions or stimulate mitosis. The major stimuli that activate secretion of hormones are humoral stimuli, nervous stimuli and endocrine stimuli. 7 Learning outcomes After studying this section you should be able to; Briefly explain the features of a hormone List the endocrine organs in the body and their secretions List the types of hormones and their modes of action Briefly explain the stimuli that bring about secretion of hormones Explain the changes that occur in the target cell when the hormone receptor complex binds to the target cell Briefly explain the negative feed back mechanism and the positive feed back mechanisms that regulate the secretion of hormones with examples 8 Session 33 HypothaIamus and Pituitary gland Session Outline Introduction 33.1 Organs of the urinary system 33.2 Basic structure of the urinary system 33.3 Blood and nerve supply 33.4 Functions of the urinary system 33.5 Regulation of the functions of the urinary system Summary Learning Outcomes Introduction The pituitary gland secretes the largest number of hormones in the body. The Hypothalamus and the pituitary gland together form a special axis which regulates the functions of several endocrine glands in the body. Some of the organs that are regulated by the pituitary are the thyroid gland, the ovary, the testis, and the adrenal gland. Figure 33.1 The structure of the Hypothalamus and the Pituitary gland 9 The hypothalamus and the pituitary gland (hypophysis) both act as one unit. These glands together have the ability to regulate the activity of most of the other endocrine glands. The hypothalamus lies above the pituitary gland and connects to the pituitary gland by a stalk. The pituitary gland is about the size of a pea and lies in the hypophyseal fossa of the sphenoid bone. It is located below the hypothalamus and is attached to the hypothalamus by a stalk. It has three separate parts and each part has its own different type of cells. The anterior Pituitary (adenohypophysis) is composed of glandular epithelium, the posterior Pituitary (neurohypophysis) is composed of nervous tissue from the brain. There is a network of nerve fibres in between the anterior and posterior pituitary is known as the intermediate lobe. The hypothalamus influences the secretion of the pituitary gland by two methods. They are briefly outlined below. The influence of the hypothalamus on the anterior pituitary -The hypothalamus communicated with the anterior pituitary is supplied indirectly with arterial blood that comes from a capillary network in the hypothalamus. This network of blood vessels forms part of the pituitary portal system. The releasing and inhibiting hormones secreted by the hypothalamus respectively stimulate or inhibit the secretions from the anterior pituitary gland. The posterior pituitary- This is formed from nervous tissue. It is composed of nerve cells communicating downwards from the hypothalamic nuclei. These neurone axons form the hypothalamohypophyseal tract. The posterior pituitary hormones are produced in the hypothalamic nerve cells, they are transported along the axons and then stored in vesicles within the axon terminals to be released when required. 33.2 Self Assessment Questions Can you explain the link between the hypothalamus and the pituitary gland? Can you explain the pituitary portal system? What is meant by the hypothalamo hypophyseal tract? Pituitary hormones are secreted by the pituitary gland. They are secreted by the anterior and posterior pituitary gland. The pituitary gland is connected to the hypothalamus by the pituitary stalk (Figure 1.1) 1. Anterior pituitary The hypothalamus secretes releasing hormones that act on the anterior pituitary. The releasing hormones stimulate or inhibit pituitary hormone secretion. The hypothalamus and the anterior pituitary gland are connected by the hypothalamohypophyseal portal system. The hypothalamus secretes the following hormones: 10 • • • • • • • Thyrotropin releasing hormone -TRH Corticotropin releasing hormone- CRH Gonadotropin releasing hormone -GnRH Prolactin releasing hormone -PRH Prolactin inhibitory hormone- PIH Growth hormone releasing hormone- GRH Growth hormone inhibiting hormone -GIH (Somatostatin) Pituitary hormones may act on target organs or stimulate (or inhibit) endocrine glands to produce hormones. Hormones secreted by the anterior pituitary gland and their target endocrine organs /tissues are listed below: 1. FSH (Follicular stimulating hormone) - gonads 2. LH (Leutinizing hormone)- gonads 3. TSH (Thyroid stimulating hormone - thyroid gland 4. ACTH (Adrenocorticotropic hormone)– adrenal gland 5. GH (Growth hormone – liver and other tissue 6. Prolactin –breast Hypophysiotropic hormones The term ‘tropic’, means to stimulate the secretion of hormonally active substances in another endocrine gland, the liver or other tissues. Many of the pituitary hormones act on specific endocrine organs bringing about a release of hormones from them. Anterior pituitary hormones (except prolactin) are tropic hormones. The functional relationship between the hypothalamus and the anterior pituitary gland is summarized in the table below. Hypothalamus Growth Hormone Releasing Hormone Pituitary gland Promotes release of Growth Hormone Growth Hormone Inhibiting Hormone Inhibits release of Growth (Somatostatin) Hormone Inhibits release of Thyroid Stimulating Hormone Thyroid Releasing Hormone release of Thyroid Stimulating Hormone Corticotrophin Releasing Hormone release of AdrenoCorticotrophin Releasing Target organ All body tissues Organs Thyroid gland Thyroid gland Adrenal gland 11 Hormone Prolactin Releasing Hormone release of Prolactin Prolactin Inhibiting Hormone release of Prolactin Leutinising Hormone Releasing release of Follicular Hormone Stimulating Hormone Gonadotrophin Releasing Hormone release of Leuteinising Hormone Breast Breast Ovary and testis Ovary and testis Hypothalamus secretes releasing hormones which stimulate or inhibit hormones in the pituitary. The anterior pituitary releases hormones which will reach the target organ through the blood stream and produce its actions. Anterior Pituitary Hormones The hormones discussed will be briefly out lined as follows. These are synthesis of hormones, transport, mechanism of action, physiological actions, regulation of secretion and disordered physiology of secretion (figure 33.2). Growth Hormone Growth Hormone (GH) is a peptide hormone secreted by the cells of the anterior pituitary. Growth hormone receptors are located on the cell membrane. 12 Figure 33.2 The actions of growth hormone The actions of growth hormone are tabulated in the table above and are briefly described below. Physiological actions of growth hormone 1. Stimulates growth The main function of GH is the promotion of linear growth. At the epiphysis of long bones cartilage formation is increased. The epiphyseal plate widens. It promotes laying down of bone matrix and increases the length of the bone. After growth is completed in adulthood, GH 2. Effects on the metabolism 13 GH has effects on metabolism and regulates the carbohydrate, protein and fat metabolism. GH increase amino acid uptake by cells and protein synthesis in cells. GH reduces the uptake of glucose into the cells. It increases the release of glucose from the liver. Therefore it increases blood glucose concentration. This is known as the diabetogenic effect. GH promotes the use of fat (free fatty acids) to produce energy (energy source). In certain stressful situations of the body it stimulates the production of energy by these methods. Some of these stressful states are mental stress, during fasting, and during hypoglycaemia. 3. Calcium balance GH increases Ca+2 absorption from the gastrointestinal tract and increases Ca+2 excretion from the kidney. A positive calcium balance which facilitates bone mineralization is the main effect of GH on bone. Control of GH secretion GH secretion is controlled by the hypothalamus. Hypothalamus secretes growth hormone releasing hormone (GRH) and Somatostatin . GH impairs glucose uptake into the cells and increases the release of glucose from the liver, increasing blood glucose concentration. Growth hormone secretion is stimulated in hypoglycaemia leading to an increase in blood glucose concentration. GH secretion is increased by various stimuli such as, hypoglycaemia, fasting, exercise and during sleep. GH secretion is decreased by various stimuli such as glucose, and cortisol, Disorders of growth hormone secretion Excess secretion of GH is often due to tumours of the pituitary gland. In children, over secretion of growth hormone stimulates skeletal and soft tissue growth resulting in gigantism. Excess secretion (eg. pituitary tumour ) of growth hormone in adults results in acromegaly. These individuals have enlarged hands and feet prominent protruded jaws, a broad nose, and bitemporal hemianopia . FSH, LH and Prolactin are described in the session on reproductive system 2. Posterior pituitary The hormones vasopressin (ADH) and oxytocin are synthesised by the hypothalamus. As mentioned earlier the hypothalamus controls the secretion of the posterior pituitary via the hypothalamohypophyseal tract, a neural pathway. 14 Physiological action of oxytocin will be described with the reproductive systemn Posterior pituitary hormones Antidiuretic Hormone This is also called vasopressin. It is a peptide hormone and its is synthesized by the hypothalamus, transported by axons (hypothalamo –hypophysial tract) to the posterior pituitary and secreted by the posterior pituitary. The physiological actions of ADH ADH is the principal regulator of serum osmolality. Therefore this is one of the important hormones which play a role in maintaining the internal environment. 1. Retention of water by the kidneys (main physiological action) ADH promotes the insertion of protein water channels (aquaporin) into the luminal membrane of the collecting ducts in the kidney. This results in an increase in permeability of collecting ducts in the kidney to water and a decrease in urine output. ADH increases water reabsorption in the collecting duct. Unlike aldosterone, ADH does not increase Na+ reaborption. Therefore retention of water in excess of solutes occurs resulting in a decrease in plasma osmolality. 2. Vasoconstrictor effect ADH stimulates vascular smooth muscle contraction, leading to an increase in blood pressure, e.g: in haemorrhage Regulation of ADH Secretion ADH secretion occurs in response to various stimuli. 1. Osmotic stimuli When plasma osmolality increases,it Increases ADH secretion. The stimulus activates the osmoreceptors. od occurs in response to an increase in plasma osmolality by stimulating osmoreceptors, located in the hypothalamus (outside the blood brain barrier). Increase in the plasma osmolality and effective osmotic pressure above the normal range (285-290 mosm/kg) increases ADH secretion. 15 When plasma osmolality increases, it stimulates the osmoreceptors in the hypothalamus which then sends impulses to the hypothalamus resulting in secretion of ADH. The steps which maintain the normal plasma osmolality when the plasma osmolality increases are shown in the diagram below (Figure 33.1). 2. Alteration of the ECF Volume ADH secretion is increased when ECF volume is low and decreased when ECF volume is high. Hypotension and hypovolaemia increase ADH secretion. E.g: In haemorrhage A reduction in ECF volume increases ADH secretion, When the ECF volume increases are outlined below (Figure 1.6): 3. Angiotensin II When the ECF volume is low Angiotensin II is secreted. Angiotensin II stimulates ADH secretion from the hypothalamus. 16 Diabetes insipidus When there is deficiency of ADH secretion or when the renal tubules are not responsive to ADH, Diabetes insipidus occurs. This condition results in polyuria ( passage of a large volume of urine ) and polydipsia are seen . Unlike in diabetes mellitus the blood glucose level in these patients is normal. The other hormone secreted by the posterior pituitary gland is the hormone Oxytocin. Since it has major effects on the reproductive system, the important features of oxytocin will be discussed in the session on female reproductive tract Objectives Pituitary Gland Describe the structure of the hypothalamus and the pituitary gland Explain the influence of the hypothalamus on the lobes of the pituitary gland Outline the actions of the hormones secreted by the anterior and posterior lobes of the pituitary gland. List the hormones secreted by the Anterior and Posterior Pituitary glands Explain briefly how the pituitary hormone secretion is regulated by the hypothalamus and the hormonal feedback mechanisms Growth Hormone (GH) Outline briefly the importance of GH Outline the actions of Growth hormone on the target organs Explain briefly the physiological basis of signs / symptoms of hypo and hyper secretion of the hormone in a child and adult Anti Diuretic Hormone (ADH) Outline briefly the importance of ADH List the effects of ADH on the target organs Outline the role of ADH in regulating the volume and osmolality of ECF Enumerate the effects of hypo secretion of ADH. 17 Session 34 Adrenal gland Session Outline Introduction 22.1 Structure of the adrenal gland 22.2 Basic structure of the urinary system 22.3 Blood and nerve supply 22.4 Functions of the urinary system 22.5 Regulation of the functions of the urinary system Summary Learning Outcomes Review Questions References Introduction Adrenal Hormones The adrenal glands a two pyramid shaped organs lying over the upper part of the kidney. They have the shape of a pointed hat. When we are excited, frightened, our heart beat increases, the respiration rate increases, our eyes open wide and the pupils of the eye dilate, and we are even ready to fight, fright and flight. All these responses are brought about by the adrenal medulla. Structures of the adrenal gland Adrenal gland consists of the cortex and the medulla. The medulla secretes catecholamines and steroid hormones. The adrenal medulla secretes catecholamines whilst the cortex secretes steroid hormones, glucocorticoids such as cortisol, mineralocorticoids such as aldosterone and sex hormones. The figure 18 Figure 34 .1 Structure of the adrenal gland 1. Adrenal medulla The adrenal medulla secretions help one to deal with emergencies. 2. Adrenal cortex The hormones secreted by the adrenal cortex have different functions: • Glucocorticoids – play a part in the metabolism of carbohydrates and protein. • Mineralocorticoids - maintains Na+ balance and ECF volume. • Adrenal sex hormones - reproductive function Mineralocorticoids and glucocorticoids are essential for life. Cortisol binds to alpha globulin in plasma and the fluctuations in protein levels affect transport as in the case of thyroid hormones. Physiological actions of glucocorticoids are summarized below: 19 Glucocorticoids have many actions that produce many changes with in cells and all the tissues of the body. They act by acting on the metabolic pathways and both other means outlined below. 1. Increase protein catabolism in tissues. It produces an increase in concentration of amino acids in plasma 2. Mobilize and redistribute fat. 3. Inhibit glucose uptake by cells and promotes gluconeogenesis in the liver. This results in an increase in the level of blood glucose. This is known as the diabetogenic effect. 4. Permissive action Small amounts of glucocorticoids are essential for many metabolic reactions. Eg For gluconeogenic action of glucagons and for glucocorticoids to produce its calorigenic effect. 5. Vasoconstriction - help catecholamines to produce vasoconstriction. This action restores vascular reactivity. 6. Reduction in the number of circulating lymphocyte, eosinophils, basophils 7. Adapt to stress - Glucocorticoids are essential for the body to resist the stress caused by surgical operations, infections and emotional states. 8. Prevent inflammatory changes in the cell. 9. Decrease bone formation Regulation of glucocorticoid secretion Glucocorticoid secretion is regulated mainly by ACTH by a negative feedback inhibitory process. Stressful situations and Corticotrophin Releasing Hormone stimulate the release of ACTH. (This is shown in the Figure 34.2) -++ Releases CRH Hypothalamus ++ -++ Stimulates anterior pituitary Release of ACTH ++ Stimulates adrenal cortex Release of Cortisol 20 Regulation of glucocorticoid secretion. Prolonged treatment with large doses of glucocorticoids inhibits the pituitary gland. This will inhibit the adrenal cortex, resulting in atrophy of the adrenal cortex which can become not responsive to ACTH. This is dangerous if this glucocorticoid treatment is stopped suddenly, as then the cortisol concentration suddenly drops and produces many adverse effects. Disorders of glucocorticoid secretion Increased secretion of plasma glucocorticoid produces the disorder known as Cushing’s syndrome. These effects are in opposite to the normal action of glucocorticoids. They are summarized below. • Increased protein catabolism results in poorly developed muscles, thin skin and subcutaneous and poor wound healing • redistribution of body fat results in thin hands and feet; collection of fat in abdominal wall (pendulous abdomen), moon face, and buffalo hump ( fat deposition in neck) • • Reddish purple striae due to thin skin of the abdomen Diabetes mellitus due to increased gluconeogenesis & decreased peripheral utilization. • • Increase in facial hair and acne – due to the excess secretion of androgens Hypertension- excess glucocorticoids having mineralocorticoid action Osteoporosis- decreased bone formation and increased bone resorption Mineralocorticoids: One of the main mineralocorticoids produced is aldosterone Aldosterone The main function of aldosterone is to regulate mineral metatabolism. Aldosterone acts on the collecting duct of the kidney. It promotes the absorption of Na+ in exchange for K+ and H + from the cells of the collecting duct. Thus it increases salt reabsorption. This mechanism helps to expand the ECF volume. This hormone is most active when the blood volume is decreased (as in hypovolaemic states) such as haemorrage, diarrhoea, and vomiting etc. Aldosterone secretion is increased by: • • • ACTH from the anterior pituitary Renin from the kidney via angiotensin II A rise in plasma K + concentration. 21 Disorders of the aldosterone action Disease conditions can give rise to excess production of aldosterone or deficiency in the secretion from the adrenal cortex. Primary hyperaldosteronism (Conn’s syndrome) Excess production of aldosterone can occur due to an adrenal cortex lesion. This is known as primary hyperaldosteronism or Conn’s syndrome Physiological basis of the signs and symptoms of Conn’s syndrome: In this disorder there is an excess aldosterone lead to Na+ retention and K+ depletion. This results in ECF volume expansion and hypertension. Addison’s disease Hyposecretion of the adrenal cortical hormones results due to primary adrenal insufficiency is referred to as Addison’s disease. In this condition there is defection secretion of all three classes of hormones. Most of the clinical features observed are due to reduction in glucocorticoids and mineralocoticoids. Decreased adrenal androgen secretion would not be evident due to the presence of normal testes and ovaries. Adrenal androgens Dihydroepiandrosterone and androstenedione are the predominant androgens produced by the adrenal cortex. In the female, adrenal androgens are the main source of androgens. This promotes the growth of pubic and axillary hair. The effect of adrenal androgens: • Mascuilinizing effect in the female • Promotes protein anabolism and growth Testosterone from the testis is the most active androgen. Adrenal androgens have less than 20% of activity of testosterone. Adrenal medulla Norepinephrine, epinephrine and dopamine are catecholamines secreted by the adrenal medulla. Apart from the adrenal medulla, norepinephrine is also secreted from the noadrenergic nerve endings. 22 Norepinephrine and epinephrine act via α and β receptors. Actions of norepinephrine and epinephrine: • Glycogenolysis in the liver and skeletal muscle. • Mobilization of free fatty acids from adipose tissue. • Norepinephrine and epinephrine produce an increase in the basal metabolic rate. • Increase in heart rate and force of contraction, mediated via the β 1 receptors. • • Increase in diastolic blood pressure by norepinephrine In contrast epinephrine dilates the blood vessels in skeletal muscles decreasing diastolic blood pressure. Regulation of secretion of epinephrine and norepinephrine Epinephrine and norepinephrine secretion is increased in stressful conditions such as exposure to cold, hypoglycaemia, during sever injury to the body, and hypoglycaemia When the above hormones are secreted in exposure to cold it results in increase in the basal metabolic rate and heat is produced to control body temperature. In hypoglycaemia these hormones increase the blood glucose concentration by activating glycogenolysis. During a stressful situation these hormones provide additional oxygen to tissue by bronchodilation, increasing myocardial contractility, reducing the urine output, and redistribution of blood to the vital organs. Pheochromocytoma Pheochromocytoma is a tumour in the cells that secrete catecholamines in the adrenal medulla. Summary In summary you learnt about the adrenal gland. The gland is divided into the adrenal medulla and the cortex. The adrenal medulla secretes norepinephrine and the adrenal cortex secretes cortisol and aldosterone. The main functions of these hormones were discussed. The effects when these hormones are oversecreted and undersecreted were explained in this session. 23 Objectives Adrenal Gland Adrenal Cortex List the hormones secreted by the adrenal cortex Outline the synthesis and the regulation of secretion of each hormone Briefly outline the effects of glucocorticoids / mineralocorticoids on target cell Organs Give a short account on the physiological basis of signs / symptoms of hypo and Hyper secretion of glucocorticoids / mineralocorticoids Adrenal Medulla List the hormones secreted by the adrenal medulla Outline the • synthesis and the regulation of secretion of hormones • mechanism of action on the target organs • effects on target organs • signs / symptoms / principles of treatment in pheochromocytoma 24 Session 35- Thyroid and parathyroid glands Session 35 Thyroid and Parathyroid Glands Session Outline Introduction 22.1 Organs of the urinary system 22.2 Basic structure of the urinary system 22.3 Blood and nerve supply 22.4 Functions of the urinary system 22.5 Regulation of the functions of the urinary system Summary Learning Outcomes Review Questions References In this session you will discuss the main functions and features of an important gland located in your neck . the thyroid gland. The thyroid gland has a butterfly shape and is located anterior to the thyroid cartilage in the neck. It is an organ essential for life Thyroid hormone The hormones secreted by the thyroid gland are as follows: Thyroxine (T4) Tri iodo thyronine (T3) Functions of thyroid hormone Thyroid hormones maintain the metabolism in the tissues that is best for their normal function. It stimulates O2 consumption of most cells, regulates lipid and carbohydrate metabolism and is necessary for normal growth and maturation. In infants the thyroid hormone is required for normal development of the central nervous system and in children for normal growth and maturation. In adults normal functions of multiple organs and systems occur due to thyroid hormones. Thyroid hormone is not essential for life. However inadequate production results in hypothyroidism and an excess production results in hyperthyroidism. 25 The functional unit The functional unit of the thyroid gland is the thyroid follicle. The thyroid gland is made up of multiple follicles. Each follicle is lined by a single layer of epithelium. The follicle is filled with colloid. Inactive follicles are filled with colloid and lined by flat cells. Active follicles are small and are lined by cuboid columnar cells. Synthesis of thyroid hormone T4 and T3 are derived from the iodine containing amino acid tyrosine. The thyroid cells perform three important functions. Several steps occur in the thyroid follicle during synthesis and secretion of T4 andT3 Uptake and transport of iodine is followed by the uptake of iodide. Iodide is converted to iodine by oxidation. The molecule tyrosine is iodinated and coupled to form the biologically active, T 4 and T3.The bond between the tyrosine residues and the thyroglobulin breaks down thT3 and T4 Transport of thyroid hormone The secreted thyroid hormones are translated and secreted they are bound to plasma proteins. The plasma proteins that bind thyroid hormones are albumin pre albumin and Thyroxin binding globulin (TBG) Thyroid hormones are bound to plasma proteins to maintain a large pool of hormones and for uniform utilization by the target cells.A small amount of thyroid hormones is found in free form. The free hormones are physiologically active and inhibit TSH. Control of thyroid function Thyroid function is regulated primarily by TSH. TSH influences follicle formation and also every step in the pathway of synthesis and secretion of thyroid hormone. Since prolonged TSH stimulation increases the growth of the gland and weight of gland, this gives rise to an enlargement of thyroid gland causing detectable enlargement. This is referred to as a goiter.TSH secretion is in turn regulated by Free T3, T4 and TRH. Free T3 and T4 negatively inhibit TSH secretion. TSH secretion is also inhibited by stress. TRH has a positive feedback effect on TSH secretion. Mechanism of action of thyroid hormone Receptors for thyroid hormones are located in the nucleus. The affinity of receptors for T3 is more than for T4. In order to produce actions the thyroid hormones bind to the receptor and the hormone receptor complex increases gene transcription. 26 The physiological actions of thyroid hormones are summarized below: 1. Calorigenic action T3 and T4 increase the oxygen consumption of tissue by increasing the metabolic rate. Body temperature is slightly increased. 2. Influence on actions of catecholamines Thyroid hormones increase the number of adrenergic receptors in tissues. It also increases the affinity of the adrenergic receptors to catecholamines. However, thyroid hormone does not increase the catecholamine level. 3. Cardiovascular system The thyroid hormone has actions on the myocardium, SA node and the blood vessels. by an ionotropic effect. It increases the contractility of the myocardium. A chronotropic effect on the heart increases the heart rate. The peripheral resistance is reduced by thyroid hormones due to cutaneous vasodilatation. 4. Nervous system Thyroid hormone has actions on the central and peripheral nervous systems. The thyroid hormone produces wakefulness and alertness by activation of the reticular activating system. It increases the excitability of nerves, affecting the reaction time of the stretch reflex. 5. Growth and development is stimulated by facilitating ossification, influences the linear growth of bone. Thyroid hormone promotes tooth development and eruption. 6. It is essential for the development of the brain before and after birth (during infancy). It is required for normal myelination, development of axons, dendrites and synapses mainly during the infancy period. 7. Increases the rate of Carbohydrate absorption from the gastrointestinal tract. 8. It is essential for normal development and function of reproductive glands. 9. It is essential for normal erythropoiesis. Clinical features of disordered secretion of thyroid hormone The effects of thyroid disorders can be explained in terms of disordered physiology. Clinical features of inadequate or excess production of thyroid hormones are described in the paragraphs below. The clinical features in these conditions can be explained by an understanding of the physiological actions of thyroid hormones. Hyperthyroidism Clinical features appearing in hyperthyroidism and its pathophysiological basis are as follows. 27 1. Extra heat production - occurs due to the calorigenic action. Body temperature rises. Cutaneous vasodilation gets rid of the extra heat in the body. leads to warm skin and sweating. Peripheral resistance is decreased. Muscle weakness occurs due to protein catabolism brought about due to the calorigenic effect of thyroid hormones. Ionotropic effect on the myocardium and increases the contractility of the myocardium, the cardiac output is increased. It has a chronotropic effect on the heart, tachycardia and palpitations are produced. Irritability and restlessness are the central nervous system effects the reaction time of the stretch reflex is shortened. This hormone is essential for normal development and function of the reproductive system. Therefore menstrual abnormalities occur in hyperthyroidism. 7. Diarrhoea occurs as a result of increase in frequency of bowel contractions caused by increased thyroid hormone action on gastrointestinal smooth muscles. 8. Osteoporosis occurs due to bone resorption exceeding bone formation. Bone matrix formation is decreased due protein catabolism in this condition. 9. Eye signs Lid retraction - Sclera is seen below the upper eye lid Exophthalmus - Sclera can be seen above the lower eye lid (Figure 1.10). Proptosis - Eye balls are pushed forward in hyperthyroidism (Figure 1.11). Exophthalmus and proptosis are only seen in Graves’ disease. Hypothyroidism Reduction in the secretion of the thyroid hormone may occur before or after birth (acquired). Hypothyroidism occurring before birth is called congenital hypothyroidism and after birth is called acquired hypothyroidism. Clinical features in hypothyroidism – 1. Goiter - diffused thyroid enlargement (Figure 1.12). Deficient thyroid hormone production results in TSH hypersecretion giving rise to a goiter. 2. Physical slowness occurs due to a decrease in basal metabolic rate. 28 3. Syndrome of adult hypothyroidism is called myxedema. Myxedema occurs due to deposition of mucopolysacharides in the subcutaneous tissues. Thyroid hormones inhibit the synthesis of mucopolysaccharides. This results in these complexes accumulating in the subcutaneous tissue - around the eye lids, tongue, vocal cords and in the interstitial spaces resulting in weight gain. mucopolysacharides are deposited and produce the following clinical features Tissue Clinical feature Around eye lids Puffy eye lids Tongue Large tongue, slurred speech Vocal cords Dermis Around nerves Interstitial spaces Low pitch voice Coarse skin Deafness, Parasthesia, Carpel tunnel syndrome Oedema of hands and feet 4. Reduced activity of reticular activating system occurs due to a reduction in the response to catecholamines. This results in slow mentation, lethargy and sleepiness 5. Actions on the SA node Since the thyroid hormone has chronotropic effects on the heart, when the are reduced the heart rate is reduced and bradycardia is produced. hormone levels 6. Thyroxine is required for the normal menstrual cycle. Menstrual abnormalities such as menorrhagia (excessive regular menstrual flow) occur therefore in hypothyroidism. 7. Thyroid hormone removes cholesterol from the circulation. In hypothyroidism the cholesterol concentration is increased leading to an increase risk of ischeamic heart disease. 8. Peripheral nervous system Since thyroid hormone has an influence on the peripheral nervous system, reduced hormones decrease the excitability of nerves. Therefore the reaction time of the stretch reflex is prolonged. 9. Since the thyroid hormone is necessary for normal erythropoesis in hypothyroidism anaemia occurs due to diminished red blood cell production. 10. Thyroid hormone influences the normal functioning of the smooth muscles as well. Therefore hypothyroidism results in constipation. Cretinism Children who are hypothyroid from birth are called cretins (Figure 1.13). The clinical features manifest within a few days from birth. This condition can lead to irreversible brain damage, if untreated and therefore early recognition is important. 29 Pathophysiological basis for the clinical features in cretins as a result of diminished activity of the thyroid hormones are given in the following Table Pathophysiological basis for the relevant clinical features in cretinism Pathophysiological basis Mucopolysacharides deposition around eye lids Mucopolysacharides deposition around Face Mucopolysacharides deposition around Tongue Mucopolysacharides deposition around Vocal cords Mucopolysacharides deposition around Dermis Central nervous system Smooth muscle Maturation of the enzyme glucuronyl transferase Linear growth of bone Tooth development and eruption Brain development Cerebral cortex Clinical feature Puffy eye lids Course ugly features Large tongue, protruding tongue, noisy respiration, feeding difficulties Hoarse cry Coarse skin Sleepiness, uninterested in his surrounding Constipation Prolonged physiological jaundice Short stature, Infantile body proportions Delayed eruption of teeth Delayed milestones Mental retardation Tests of thyroid function are conducted to: • • • Determine the thyroid state of the patient. Determine the cause of the alteration in the state, if any Monitor the progress of the illness with treatment. The following serum tests to determine thyroid function are often done. They are the level of Free T3, Free T4 and TSH. Objectives Thyroid Hormone Outline the factors regulating synthesis and secretion of thyroid hormones Write a brief account on the effects on the target organs Enumerate the signs / symptoms of hypo and hyper secretion in adults / infants 30 Give an account on the usefulness of thyroid function tests in assessing disordered function of the gland Calcium metabolism Introduction To sustain life serum calcium concentration has to be within a constant range. Parathyroid hormone (PTH), Vitamin D (1,25-dihydroxycholecalciferol) and calcitonin play a vital role in regulating serum calcium. The average serum calcium concentration is 2.5 mol. / L (9.5 mg/dl). A certain percentage of serum calcium is bound and another percentage is in the free form. Fifty percent of the serum calcium is free and 40% bound to protein. 10% is complexed with substances like citrate. Free calcium is also called ionised calcium and it is the physiologically active form. The calcium concentration depends on rate of gastrointestinal absorption, renal calcium absorption and excretion, bone mineralisation and demineralization (Figure 1.17). Several physiological processes are dependent on serum calcium. The neuromuscular excitability depends on the serum calcium concentration. When calcium level drops the neuromuscular excitability increases. In alkalosis binding of calcium to protein increases. This will lower the free calcium concentration, producing neuromuscular hyperexcitability. In hyperventilation neuromuscular excitability increases due to alkalosis. Calcium is essential for secretion of many hormones and neurotransmitters. Calcium is essential for clotting of blood in both the intrinsic and extrinsic pathway of clotting. Intracellular Ca++ is a vital second messenger. Calcium is needed for excitation contraction coupling of both skeletal and cardiac muscle. 31 Figure 1.17 Physiological functions of calcium. Therefore in our body serum calcium concentration is regulated accurately. Parathyroid hormone (PTH), Vitamin D (1,25-dihydroxycholecalciferol) and calcitonin are the hormones which maintain serum calcium. The major organs involved in calcium homeostasis are the gastrointestinal system, kidney and the bone. In the gastrointestinal tract calcium absorption occurs via the upper small intestine in the presence of vitamin D. Ninety-eight percent (98%) of the filtered calcium is reabsorbed by the kidney. This occurs by diffusion and carrier mediated transport in the presence of parathyroid hormone and vitamin D. Calcium is also exchanged between bone and plasma; 90% of the calcium is in the skeleton. Bone is formed of matrix (osteoid tissue) and minerals. Structure of bone Bone forming cells are called osteoblasts. Osteoblasts synthesize the bone matrix protein collagen and osteocalcin. After formation of the bone matrix the osteoblasts help in mineralization as well. Bone mineralization is done by secreteing alkaline phosphatase by the osteoblast. This helps in precipitation of calcium in the bone. Osteoblasts that are buried in bone matrix become osteocytes. These are numerous in mature bone. Osteocytes are within bone spaces called lacunae. Lacunae are interconnected with each other via channels called canaliculi. There is an extensive canalicular system connecting the osteocytes and osteoblasts forming a functional syncytium. The previously formed bone is eroded by osteoclasts. Bone fluid is found in lacunae and in the canaliculi. The minerals in bone are exchanged with minerals in ECF. Bone fluid is separated from the extracellular fluid by a layer of osteoblast. 32 Bone remodelling The process of bone formation and break down (resorption) is called bone remodelling. Bone remodelling varies with the age. Until 20 years of age bone formation is more than resorption and after 30yrs bone formation is less than resorption. Parathyroid hormone (PTH) Parathyroid hormone is a polypeptide hormone secreted by four parathyroid glands which are embedded in the thyroid gland. Actions of Parathyroid hormone The main action is to increase the plasma calcium concentration. PTH has direct actions on bone , kidney and an indirect action on the gastrointestinal tract. Actions of PTH on bone PTH acts mainly on the osteoclast and mobilizes Ca++ from bone. It decreases bone fluid Ca++ and increases ECF Ca++. It causes increase in the remodeling process. Initially bone osteoclasts stimulate resorption and subsequently there is bone formation by osteoblasts. Actions of PTH on Kidney PTH increases the Ca++ reabsorption in distal convoluted tubule. PTH also decreases the reabsorption of phosphate. Therefore it has a phosphaturic action. Actions of PTH on gastrointestinal system PTH stimulate the formation of vitamin D. Vitamin D stimulates absorption of Ca++ and PO43-- in the intestine. Therefore PTH indirectly increases Ca++ absorption from the intestine. Regulation of secretion (Figure 1.18) Ionized calcium directly regulates the secretion of parathyroid hormone. Low ionized calcium stimulates the secretion of PTH. PTH by acting on bone mobilizes calcium from bone. PTH by acting on the kidney produces absorption of Ca++ from the distal convoluted tubule. It also synthesises vitamin D giving rise to absorption of Ca++ from the intestine. These effects will bring the ionized calcium back to normal. 33 Vitamin D (1, 25-dihydroxycholecalciferol) Vitamin D is a steroid hormone. Vitamin D is obtained from the diet. It is also synthesised in the skin by 7-dehydrocholesterol. On exposure of skin to sunlight the 7-Dehydrocholesterol is converted to cholecalciferol (Vitamin D3). Vitamin D3 is converted to 25-hydroxycholecalciferol (calcidiol) in the liver. In the kidney 25hydroxyclolecalciferol is converted to the active form 1,25-dihydroxyclolecalciferol. Actions of vitamin D This hormone increases the serum calcium concentration. It also facilitates bone mineralization. Vitamin D act on the gastrointestinal system, kidney and bone. Actions of vitamin D on gastrointestinal system This hormone increases calcium and phosphate absorption from the intestine. The intestinal mucosa contains calcium binding protein called calbindin. Vitamin D increases the synthesis of this calbindin protein. Actions of vitamin D on kidney Vitamin D increases tubular reabsorption of Ca++ and PO4-3. Actions of vitamin D on bone It is essential for normal bone mineralization. It activates osteoblasts to mineralize osteoid tissue. Control of secretion of 1, 25-dihydroxycholecalciferol When plasma calcium is low, PTH secretion is increased and this in turn will increase the synthesis of 1,25-dihydroxycholecalciferol. The opposite occurs when the plasma calcium is high. This is the adaptation of calcium absorption in the intestine. Oestrogen, prolactin and growth hormone increases the circulating 1,25dihydroxycholecalciferol. Hyperthyroidism is associated with decrease in circulating 1,25dihydroxycholecalciferol. 34 Calcium exchange between tissue and plasma. Calcitonin Calcitonin is a polypeptide secreted from the parafollicular cells of the thyroid glande. It is a serum calcium lowering hormone. Calcitonin hormone stimulate bone osteoblast to mineralize bone.This hormone inhibits bone osteoclasts. This also inhibits absorption of Ca++ and PO4-3 from renal tubule. In addition to the above 3 hormones, other hormones also influence the Ca++ homeostasis. Growth hormone increases excretion of Ca++ in urine. It also increases Ca++ absorption from the gastrointestinal tract. However the Ca++ absorption from the gastrointestinal tract is more than the excretion in the urine. Therefore growth hormone produces a positive Ca++ balance. Glucocorticoids increase bone resorption and decrease bone formation by inhibiting protein synthesis. 35 They decrease absorption of Ca++ and PO4-3 from the gastrointestinal tract and increase the renal excretion of Ca++ and PO-34.Therefore Glucocorticoids produce bone osteoporosis. Oestrogens prevent osteoporosis by inhibiting osteoclasts. Thyroid hormone tends to produce osteoporosis because of the protein catabolic effect. Hypocalceamia Hypocalcaemia results from removal of the parathyroid gland (parathyroidectomy). In this condition the PTH and the 1,25-dihydroxycholecalciferol concentrations reduces. PTH deficiency result in reduced renal reabsorption of calcium and 1,25-dihydroxycholecalciferol deficiency result in reduced gastrointestinal absorption of calcium. In hyperventilation alkalosis occurs. Binding of calcium to protein will also lower the free calcium concentration although the total plasma concentration remains normal. Hypocalcaemia increases neuromuscular excitability. This gives rise to carpopedal spasm. Tetany occurs as a manifestation of carpopedal spasm. A characteristic form occurs in the upper limb. Adduction of the thumb, flexion of the metacarpophalangeal joints, extension of the interphalangeal joints, flexion of the wrist and elbow joints (Figure). This is called Trousseau’s sign. The Learner should be able to • list the main functions of calcium in the body • outline the distribution of calcium in the body • name the hormones regulating plasma calcium levels • outline the role of each hormone in homeostasis of plasma calcium enumerate the effects of hypo and hyper parathyroidism on the body • compare / contrast osteomalacia / rickets / osteoporosis in relation to their • aetiology • bony changes • signs / symptoms • treatment methods 36 Session 37- Endocrine pancreas Session 37 Endocrine Pancreas Session Outline Introduction 22.1 Structure of the endocrine pancreas 22.2 Insulin 22.3 Glucogon 22.4 Somatostatin 22.5 Regulation of the function of the endocrine pancreas Summary Learning Outcomes Review Questions References The pancreas gland is closely associated with the gastrointestinal system and has both exocrine and endocrine functions. The endocrine activity of the pancreas is due to the secretions of a group of cells known as the islets of Langerhan. These islet cells form only a very small proportion of the pancreatic gland. A healthy adult has about a million islets in his pancreas. 37.1 The endocrine structure of the pancreatic islets 37.2 The hormones secreted by the Pancreas Hormones secreted by the islets of Langerhan are insulin, glucagon, somatostatin and pancreatic polypeptide. All these hormones are peptide hormones. Insulin Insulin is an anabolic hormone which causes storage of fatty acids, amino acids and glucose. Glucagon is a catabolic hormone which mobilizes fatty acids, amino acids, glucose. Therefore these two hormones are reciprocal in action. Somatostatin inhibits release of other hormones such as insulin, glucagons, and pancreatic polypeptide. It also regulates the secretion of islet cells. Pancreatic polypeptide inhibits gallbladder contraction and pancreatic exocrine secretion. 37 Insulin Insulin is a polypeptide hormone secreted by the beta () cells of the islets of Langerhans. It consists of two peptide chains connected by a connecting peptide (C peptide). Actions of insulin are as follows: The following actions occur within seconds (rapid): It increases transport of glucose, amino acids and K+ in to insulin sensitive cells. (Figure 1.22) There are several glucose transporters in the body. However only the glucose transporter named GLUT4 is stimulated by insulin. This is present in skeletal muscle, cardiac muscle and adipose tissue. Figure 1.22 Insulin dependent entry of substances into tissues. Insulin does not increase the entry of glucose into: • Mucosa of the gastrointestinal system • RBC • Brain • Renal tubular cell The following actions occur within minutes (Intermediate): Insulin stimulates protein synthesis and inhibits protein degradation in the liver and muscle. It stimulates synthesis of glycogen and inhibits glygogenolysis in the liver and muscle. It inhibits gluconeogenesis in the liver. These actions result in decreased glucose output from the liver. It also activates glycolytic enzymes The following actions occur within hours (delayed): 38 Insulin activates lipoprotein lipase and inhibits hormone sensitive lipase. It increases lipogenesis in the liver and adipose tissue. The above actions of insulin have the following actions in various tissues: Insulin increases synthesis of lipids, protein, glycogen in the liver and decrease ketogenesis and gluconeogenesis. Insulin activates the lipoprotein lipase and inhibits the hormone sensitive lipase enzyme. Insulin increases synthesis of lipids in the adipose tissue. Insulin increases synthesis of protein, glycogen in the muscle and decrease protein catabolism and gluconeogenesis. It increases ketone body uptake in the muscle when necessary. Regulation of insulin secretion Glucose is the prime regulator of insulin. When the glucose concentration rises insulin secretion is increased and vice versa. Arginine, leucine and ketoacids stimulate beta cells of the pancreas. Glucagon, catecholamines, thyroid hormone, adrenal glucocorticoids and growth hormone stimulate the secretion of insulin. Glucagon Glucagon is a polypeptide secreted by the pancreatic alpha (α) cells, intestine and brain. Glucagon has the following actions on metabolism: 1. Carbohydrate metabolism Glucagon increases blood glucose levels by stimulating glycogenolysis in liver (not in muscle). Glucagon increases gluconeogenesis in liver from amino acids, lactate , and pyruvate. 2. Lipid metabolism Glucagon increases lipolysis in adipose tissue, because it activates the hormone sensitive lipases. It increases the FFA and ketone bodies in the circulation. 3. Protein metabolism Glucagon increases the break down of protein in the liver. 39 Glucose homeostsis Plasma glucose is maintained at a constant level. Normal plasma glucose concentration is 4.5 5.6 mmol/ L (70 - 110mg/dl). There is a balance between the amount of glucose entering and leaving the circulation. (Figure 1.23) Factors that determine the plasma glucose level are dietary intake, rate of entry of glucose into cells and the glucostatic activity of the liver. Figure 1.23 Interaction of the liver, pancreas and the intestines in glucose homeostasis. Hepatic glucostat Liver functions as a glucostat. It helps to maintain a constant circulating glucose level in fasting as well as in fed state. (Figure 1.24) During fasting, liver glycogen is broken down and glucose is added to the blood stream. In prolonged fasting when glycogen is depleted gluconeogenesis begins by using amino acids and glycerol as substrates. During the fed state glucose is converted to glycogen in the liver. A greater percentage of glucose is converted to fat in the adipose tissue. 40 Figure 1.24 Glucostatic activity of the liver. . Diabetes Mellitus Diabetes mellitus is a disease caused by relative or absolute deficiency of insulin. The disease has two distinct categories namely type 1 diabetes (insulin dependent diabetes mellitus) and type 2 diabetes (non insulin dependent diabetes mellitus). Type I diabetes is common in the younger age group (< 30 years) and results from insulin deficiency. It is an autoimmune condition. Type II diabetes is common in the older age group (> 30 years) and results from insulin resistance. Pathophysiology of diabetes mellitus 1. One of the actions of insulin is to increase transport of glucose to insulin sensitive cells by increasing the number and activity of the glucose transporter named GLUT4. In diabetes mellitus when there is relative or absolute deficiency of insulin, the amount of glucose entering insulin sensitive cells is reduced. 41 Lack of insulin reduces the peripheral utilization of glucose for glycolysis. (Figure 1.25) Reduced uptake of glucose, amino acids and K+ by peripheral tissues in diabetes mellitus. 2. Derangement of glucostatic function of liver In the liver a relative or absolute deficiency of insulin reduces the formation of glycogen due to inhibition of the enzyme called glycogen synthase . Glycogenolysis is increased due to increase in activity of the enzyme phosphorylase. There is increased gluconeogenesis due to an increase in the gluconeogenic substrates such as glycerol, fatty acids, amino acids and the unapposed actions of adrenal steroids and growth hormone. All of the above leads to derangement of glucostatic function of liver. This results in an increase in glucose output from liver. (Figure 1.26) Increase in liberation of glucose from the liver. 42 Therefore due to reduction in peripheral utilization and derangement in the glucostatic function of liver, hyperglycaemia (increase blood glucose concentration) occurs. This condition will give rise to a situation where glucose concentration in the extracellular fluid is more than in the intracellular fluid. The cells are starved in the midst of plenty. Consequences of hyperglycaemia 1) Polyuria This refers to excess urine production. Glucose concentration in the renal tubule is increased and the limit of maximum absorption is exceeded. Then glucose starts appearing in urine. The plasma concentration at which the glucose begins to appear in urine is called the renal threshold. When the glucose concentration in the plasma increases the renal tubule glucose concentration also increases. Since glucose is an osmotically active particle it draws water into the tubule and increases the urine volume. This is polyuria (Figure 1.28) . Figure 1.28 Osmotic diuresis following hyperglycaemia. 43 2) Polydipsia (Figure 1.29) Polydipsia is excessive drinking of water. This due to activation of the thirst mechanism. Polyuria gives rise to loss of the ECF volume resulting in hypovolaemia. Also the tonicity of the ECF will increase. Figure 1.29 Polydipsia following hyperglycaemia. When the tonicity increases the hypothalamic osmoreceptors are stimulated which in turn will act on the thirst centre producing thirst. Due to hypovolaemia the volume receptors acting on the hypothalamus also produce thirst. Another reason is due to hypovolaemia. Angiotensin II secretion is stimulated via renin and this also will give rise to an increase of thirst. 3) Glycosylated haemoglobin (HbAIc) formation Glycocylated haemoglobin is formed by a reaction between the amino acids of beta chain of haemoglobin and glucose. The glycocylation of haemoglobin is dependent on the blood glucose concentration. Half life of glycocylated haemoglobin relates to the life span of red cells (120 days) and glycocylated haemoglobin formation is proportionately increased in hyperglycaemia. 44 Therefore HbAIc measurement will indicate the glycaemia of the preceding 4-6 weeks (Figure 1.30). Figure 1.30 HbAIc measurement indicates the glycaemia of the preceding 4-6 weeks. 2. Effects of intracellular glucose deficiency. Due to break down of protein or fat for energy requirement, weight loss is seen in diabetic patients 3. Derangement of protein metabolism Inhibition of protein synthesis in insulin sensitive cells is due to reduced amino acid entry. There is stimulation of protein degradation. Gluconeogenic substrates (amino acids are formed due to break down of proteins). Increase in gluconeogenesis occurs due to lack of insulin and due to other hormones such as glucagons and glucocorticoids. Blood amino acids increase in the absence of insulin 4. Derangement of lipid metabolism • • • Due to decreased activity of the lipoprotein lipase there is decreased clearing of the VLDL (very low density lipoproteins). Therefore plasma free fatty acid, VLDL and chylomicron concentration is increased. Reduced entry of glucose reduces the synthesis of triglyceride. In the absence of stimulation of hormone sensitive lipase in diabetes, there is break down of lipids. This results in increase in the FFA level in the circulation. FFA are NEFA, UFA. The FFA in the liver is converted to ketone bodies. Ketone bodies are anions of strong acids. Metabolic acidosis occurs. The mechanism of air hunger due to ketone bodies is outlined below: Hospital admissions in diabetes are a common occurrence due to various reasons. Diabetes metabolic emergencies occur in few patients and this is due to several causes namely hyperosmolality in the absence of ketosis and hyperosmolality with ketosis. Both conditions can lead to coma (unrousable unresponsiveness). 45 Hyperosmolar coma In intercurrent illnesses or older patients with diabetes mellitus, ECF glucose concentration is higher than in ICF. Therefore water shifts from brain cells to the extracellular compartment, leading to coma. Coma occurs when effective plasma osmolality reaches about 340 mosm/l. Diabetic ketoacidosis occurs when there is hyperglycaemia and formation of ketone bodies (ketosis). Kussmaul breathing occurs in this condition. Ketone bodies induce vomiting. Polyuria occurs in both situations due to hyperglycaemia induced osmotic diuresis. In hyperosmolar states the fluid and electrolyte depletion is more than in ketoacidosis.The reason is that in hyperosmolar states due to the absence of ketone bodies and symptoms due to ketone bodies (vomiting and Kussmaul breathing). Later in ketosis severe polyuria, nausea, vomiting causes depletion in intravascular volume decreasing renal blood flow. Hypoglycaemia Patients with diabetes mellitus are prone to get hypoglycaemia since these patients use oral hypoglycaemic drugs. Hypoglycaemia leads to dysfunction of the brain. The brain extracts glucose slowly since entry is not helped by insulin. This is because brain cells are very dependent on extracellular glucose, since brain cannot store, synthesize or metabolize substances other than glucose and ketones (Figure 1.31). Figure 1.31 The importance of maintaining a constant blood glucose concentration for functioning of the brain. 46 Therefore several compensatory mechanisms take place to correct hypoglycaemia: Firstly the hepatic glucose output is increased by an increase in glycogenolysis. Hypoglycaemia is a stimulus for glucagon and epinephrine secretion. Hence these two hormones produce this effect. Main counter regulation is by these hormones,which will warn the patient to seek glucose replacement. The effect produced by secretion of epinephrine is summarized below: • Increase in heart rate, palpitations, sweating, weakness and other signs and symptoms due to sympathetic overactivity. The mechanisms operating to compensate hypoglycaemia are outlined: Glucagon hepatic glucose output Epinephrine Glycogenolysis Subsequently growth hormone and cortisol secretion occurs to reduce the utilization of glucose. Growth Hormone Utilization of glucose Cortisol Since the brain is dependent on ECF glucose secondary to hypoglycaemia there is central nervous system dysfunction (neuroglycopaenia).There is confusion, headaches and can lead to coma. Laboratory findings in diabetes mellitus Blood glucose testing Normal fasting plasma glucose value is 4.5 - 5.6 mmol/ L (70 - 110mg/dl. Plasma or serum levels 10-15% are higher than whole blood glucose level. Plasma or serum level is measured since they are not affected by the packed cell volume. Venous blood samples, Capillary blood sample. Samples should be collected in tubes containing NaF which inhibit glycolysis. The enzymic method (glucose oxidase) or colorimetric method (α toluidine) can determine blood glucose concentration. 47 Urine glucose This does not reflect the actual status of diabetes due to many reasons: The bladder urine concentration reflects the blood glucose at the time of urine formation not the time of testing. After the renal threshold, glucose appears in urine and until that time testing urine for glucose will not provide an indication of diabetes. Microalbuminuria When the microalbumin level is higher than normal it indicates development of renal involvement of diabetes (diabetic nephropathy). vi. Endocrine Pancreas Glucagon • outline the regulation of secretion and the main effects on the body Insulin • outline the regulation of secretion • explain the role of insulin in regulating the glucose levels in blood • explain briefly the physiological basis of the signs / symptoms / • complications of diabetes mellitus • list the likely causes of coma in diabetes mellitus • enumerate the likely acid /base / water / electrolyte / biochemical • abnormalities in ketoacidosis and the principles of treatment 48