Caval filters.doc - This Is Not A Clinic
advertisement

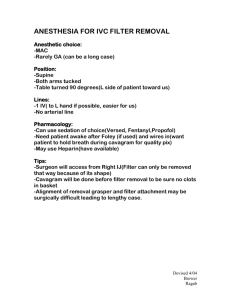
Vena Caval Filters Introduction Vena caval filters (VCFs) are devices prophylactically placed inside patients to prevent deep vein thrombosis (DVT) from becoming pulmonary emboli (PE). The number of VCFs placed in 2003 was about 100,000 1. And the industry estimated that due to percutaneous placement, expanded indications and new “optional” filters, the number would grow at 16% per year 1. Despite this, the quality of research on the true indications and efficacy of VCFs is woefully lacking. This article will give an overview of VCFs, their indications and complications. History The history of PE prevention is very unlike our current treatment methods and is fraught with failed surgical attempts to stop DVT embolization. The idea of caval interruption goes back to the 1700’s but it was not until 1893 that the first surgical ligation of the vena cava was successfully performed to prevent PE 3. The procedure was naturally associated with a high mortality 3. Femoral vein ligation was later popularized in the US in the 1930’s by Homans 3. With single femoral vein ligation a patient was still susceptible to PE from the contralateral leg, and so Ochsiner, Debakey, and O’Neil moved the point of ligation upwards to the IVC 5. By the 1960’s, vena caval ligation carried a mortality of 14% and PE still recurred at a rate of 6% primarily due to the formation of collaterals 3. Harp string grids and IVC plication with sutures were both unsuccessful attempts to overcome the failures of IVC ligation 5. In the 1950’s though, the emphasis had switched from surgical management to medical management with the advent of anticoagulation 3. In the 1970’s the first percutaneous device for vena caval interruption, the Mobin-Uddin Umbrella filter came onto the market 5. It was removed due to thrombotic complications in 1977 but by then the Greenfield filter had already been developed and released in 1973 5. VCFs grew in popularity after the development of the Greenfield filter and many other filters were developed to refine it and overcome its shortcomings. In 2003, the “retrievable” filter was approved, even further expanding the acceptability of these prophylactic devices 4. Vena Caval Filter Design Structural Basis VCFs have seemly chaotic forms (see illustration), but the genius of their design lies in their ability to capture as much thrombus as possible without compromising the blood flow through the vena cava. The original Kimray-Greenfield filter only decreased the cross-sectional area of the IVC by 50% when it was 2/3 filled with thrombus 5. Not only does this allow for better venous return but also allows the fibrinolytic system greater exposure to the emboli and therefore a greater chance to lyse them 5. VCFs have hooks which act to anchor the filter into the vessel wall. Because of this, VCFs have an upper limit on the size of the vessel that they can be placed into. Most VCFs cannot be placed into sections of vessels > 28mm 5. The Bird’s Nest filter is the only filter approved for IVC locations > 30mm 5. Figure 1 Vena caval filters: (a) Stainless steel Greenfield filter, (b) percutaneous stainless steel Greenfield filter, (c) titanium Greenfield filter, (d) Bird’s Nest filter, (e) Simon Nitinol filter, (f) VenaTech filter, (g) Nitinol TrapEase filter, (h) Gu¨nther Tulip filter 5. Types of Filters There are three types of filters: permanent, temporary, and retrievable. Permanent filters are placed with no intention or option of removal at a late date. These were the standard until 2003. Temporary filters are attached to lines outside the body. They are easily placed and easily removed. But they are potentially less effective in preventing PE (I did not read data that directly supported this statement) and because they are attached to outside lines they have a higher infection rate 5. Most interest has focused not so much on temporary filters as retrievable filters 4. Retrievable filters are VCFs that are designed to be both entirely internal and to be removed at a later date barring endothelialization or other complications 3. Retrievable filters have been called by many names including removable, convertible and optional 4. Optional is a name that has stuck as some have proposed that it is harmless to leave these filters in place if they cannot be removed although this has not been sufficiently studied 3,4 . Because these filters must be removed before they become endothelialized they can only be left in for a finite time, usually a maximum of 3 months, depending on the specific filter placed 3. An additional benefit is that these filters can be repositioned if they are misplaced or found to have excessive tilt as long as they have not yet endothelialized 3. The different filter types follow the same basic indications for use 4. Insertion The standard placement of a VCF is at the L3 vertebral body, caudal to the renal veins . This is done to prevent occlusion of the renal veins in the event of complete VCF obstruction or thrombosis 5. The suprarenal IVC also has a shorter length and wider diameter making it more prone to VCF complications 5. 5 Risk Factors of Venous Thromboembolism (VTE) Before discussing the indications of VCF, it is appropriate to discuss the epidemiology of the condition that they are used to prevent. General risk factors for PE include prolonged immobility, recent surgery, pregnancy, estrogen therapy, cancer, and an inherited hypercoagulable tendency 3. But the principle factor that determines a patient’s risk for VTE is their reason for hospitalization 1. Hospitalization for major trauma carries the highest risk for VTE 1. And trauma that includes spinal cord injury (SCI), lower extremity fractures, pelvic fractures, or surgical repair carries an even higher risk within the category of trauma 1. Patients who are critically ill also usually have a moderate to high risk of VTE 1. Also, DVTs that extend into the thigh or pelvis have a higher chance of embolizing to become PEs than do those that do not extend beyond the calf 3. Research Rutherford reported the sad state of VCF research after doing a Medline search covering the years from 1975 to 2000 6. Of the 568 studies found, 65% were retrospective studies or case reports, 12.9% were animal or in vitro studies, and 7.4% were prospective trials 6. Only 16 of the 568 studies involved more than 100 participants 6. Of the 568 studies, only one was a randomized trial 6. Since most data is derived from unrandomized case series with differences in populations, outcomes, duration and follow-up there is little chance for good meta-analysis 5. And by definition, since studies validating the efficacy of VCFs are lacking, there is no good comparison data between VCFs and other prophylactic methods of preventing PE 6. Efficacy The only randomized controlled trial of VCFs has been the PREPIC trial 3. This was an open trial of 400 participants with documented proximal DVT or PE 3. All participants were receiving concurrent anticoagulation 3. The patients underwent a V/Q scan at some time between 8 to 12 days after having a VCF placed 7. At day 12 there were significantly fewer PEs in the VCF group (1.1% versus 4.8%) 5. But the statistical significance only holds if asymptomatic and symptomatic PE are taken together as a group 5. If symptomatic PE are considered alone then the significance is lost (1.1% versus 2.6%) 5. At 2 year follow-up the difference in symptomatic PEs was not significant between the two groups and the recurrence of DVT became significant in the filter group 5,7 . No survival advantage was shown in the filter group, although the study was underpowered to detect a long-term difference in mortality due to PE because the mean age of the study population was 73 years 5. The next best study has been based on the California Patient Discharge Data Set 7. This was a retrospective study of discharge data from all non-federally funded hospitals in California 7. This data showed that the risk of readmission with one year after filter placement was not lower than in the control group 7. Also, a 2-fold increase in the risk of subsequent DVT was noted in patients with VCFs who had had a prior episode of PE 5. Retrievability There has been an increased trend towards retrievable filters due to the possibility of increased incidence of DVT reported in the PREPIC trial 3. But the retrieval of these filters is not always possible. Retrieval rates have been reported to range from 88 to 100% but the true rate is not known 3. The true rate is probably affected by the clinical scenario and the experience of the interventionist 3. There is no good data on the longterm consequence of leaving retrievable filters in place 6. VCF Indications, Use and Alternatives Indications The Indications for IVC filter placement are as follows: 5 A contraindication to anticoagulation and a failure to adequately anticoagulated to prevent recurrent PE are the two strongest indications for VCF placement and yet there is a lack of data for even these two scenarios 3. There is a paucity of evidence and much literature controversy for all other indication 3. Absolute indications for VCF have been defined as thromboembolic complications associated with a contraindication to anticoagulation, documented failure of anticoagulation to prevent PE, or complications of anticoagulation. Most patients undergoing filter placement meet none of these criteria 4. Indications for filter placement have also been based upon the clinical condition of the patient. It has been suggested that filters be placed in patients who could not withstand a PE (such as those with severely compromised cardiopulmonary status) even though they have not yet had a PE. Again, this is an unsubstantiated use. Matching use to Evidence Data from the California Patient Discharge Data Set showed just how much of a mismatch exists between the accepted indications for filter placement and who they are being placed in. The data showed that 45% of the VCFs were placed in patients with DVT alone, 36% were placed for PE, and 19% were placed patients without either DVT or pulmonary embolism 4. The routine use of VCFs has been strongly discouraged because their benefit has not been established and so has neither been compared to their cost 1. The placement of VCFs in trauma patients increased from 3% in the period between 1991 and 1996 to 57% between 1996 and 2001 leading to the Eastern Association for the Surgery of Trauma (EAST) to issue guidelines to limit their use 5. Filter placement also does not treat the patient for PE. The patient must still be prophylactically treated and the underlying cause of increase risk for PE managed appropriately 4. It has also not been shown that VCF themselves are not thrombogenic. Alternatives What are the alternatives to putting in a VCF? The first option is simply to not put one in. There is no evidence that the devices reduce symptomatic recurrent PE or decreases mortality, so not using them is a reasonable option. Another thing that can be done is to confirm that the patient is getting basic mechanical prophylaxis such as IPCs, graduated compression stockings, and venous foot pumps 1. And a patient who develops a recurrent PE while being anticoagulated still has not necessarily entirely failed anticoagulation. An investigation should be made to determined whether or not the patient has been therapeutic on their regimen 5. The patient may also been screened for hypercoagulable syndromes such as antiphospholipid antibody syndrome which may require a higher INR 5. Complications There are many possible complications to VCF placement. These can generally be thought of in two classes, short-term and long-term complications. VCF rates of complication may be as common as massive PE, and are extremely costly 1. Short-term complications include: 1. Recurrent PE 1 2. Inappropriate delay in instituting effective anticoagulation prophylaxis 1 3. Thrombosis at vascular access site 1 4. Filter misplacement 5. Pneumothorax 2 6. Hemorrhage 2 7. Filter misplacement 2 8. Vascular injury or perforation 2 Long-term complications include: 2 1. Recurrent PE 2. Caval occlusion 3. Filter migration 4. Excessive tilt 5. Filter and caval thrombosis 6. Strut erosion 7. Complications related to venous access procedures Filter migration and embolism occur in 2.3% of VCF in retrospective studies 2. Hooks placed on the ends of filter struts have successfully reduced the rates of filter migration, but have subsequently increased IVC penetration 5. Excessive filter tilt occurs in 0 to 56% of filter depending on the definition and type of filter used. Excessive tilt is important because it is a risk factor of PE 2. Filter tilt can be caused by placing a filter in the vicinity of entering veins 2. Entering veins can promote strut instability, which in turn leads to filter tilt 2. Caval thrombosis rates are currently substantially less than in the era of the MobinUddin model, but thrombosis remains a common event after VCF placement and has been reported at rates of 1 to 24% 2. Filter and caval thrombosis can be viewed in two different lights. Either it can be thought of as protective and a sign that the filter is protecting the lung from emboli. Or it can be thought of as the VCF itself being thrombogenic and clotting off 2. Sequelae of IVC thrombosis includes phlegmasia cerulea dolens, recurrent DVT, post-thrombotic syndrome (PTS) and recurrent PE due to thrombi that extend proximal to the thrombosed filter 5. Strut erosion can be shown on a CT scan with contrast as struts penetrating outside of the vessel 2. Strut erosion occurs at high rates and although the majority of them are asymptomatic, it may also lead to ulceration, hemorrhage, and AV fistula 2. Complications may occur in vascular access procedures (such as central line placement and pulmonary wedge catheters) in patients with VCF 2. The guidewires used to place these devices can become entrapped in a VCF 5. And attempts at forceful removal have led to cases of filter displacement or removal 5. Use of straight wires instead of J-tipped reduces the risk of entrapment as does limiting the insertion of guidewires to 18 cm 5. Future Trials A search of clinicaltrials.gov finds two VCF studies currently recruiting participants. The first study is called “Anticoagulation and Inferior Vena Cava Filters in Cancer Patient with a Venous Thromboembolism” and is cosponsored by GlaxoSmithKine. This study will compare anticoagulation with and without an IVC filter in cancer patients with PE or DVT. Patients will be monitored for 90 days for death, PE recurrence or complications of the VCF. The second study is call “PREPIC 2: Prevention of Recurrent Pulmonary Embolism by Vena Cava Interruption”. This study will enroll 400 participants with a symptomatic PE and one risk factor. The arms of the study are anticoagulation alone versus anticoagulation and a retrievable VCF. The follow-up will be for 90 days after filter placement. Outcomes will be death, recurrent PE and complications of the VCF. Any important inadequacy in these current trials is that they do not address the most pressing question about vena caval filters, which is their use in patients who can not be anticoagulated. Summary I may be wrong in my opinion, but I am adamantly against the use of VCFs. I feel that with no data to show reduced recurrence of symptomatic PE and decreased mortality they are unsupported by any evidence. Even if they are proven to be efficacious, they currently have no role in evidence-based medicine. With the enormous number of VCFs placed each year I see no reason that good randomized trials aren’t done to clarify their basic indications and long term efficacy. Instead, the published data on VCFs is flooded with case series supporting the reduced complication rate of one particular VCF over another particular VCF, leaving us with little reliable data at all. References 1. Geerts, William. Prevention of Venous Thromboembolism in High-Risk Patients. Hematology 2006. 2. Joels, Charles. Complications of Inferior Vena Cava Filters. The American Surgeon 2003; 69: 654-659 3. Young, T. Vena Caval Filters for the Prevention of Pulmonary Embolism (Review). The Cochrane Library 2007; Issue 4 4. Comerota, Anthony. Retrievable IVC Filters: A Decision Matrix for Appropriate Utilization. Perspectives in Vascular Surgery and Endovascular Therapy 2006; 18; 1: 11-17 5. Hann, Christine. The Role of Vena Caval Filters in the Management of Venous Thromboembolism. Blood Reviews 2005; 19: 179-202 6. Rutherford, Robert. Prophylactic Indications for Vena Cava Filters: A Critical Appraisal. Seminars in Vascular Surgery 2005; 18: 158-165 7. Streiff, Michael. Vena Caval Filters: A Review for Intensive Specialists. Journal of Intensive Care Medicine 2003; 18: 59-79