This is based
advertisement

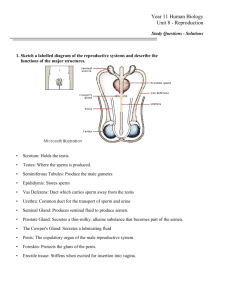
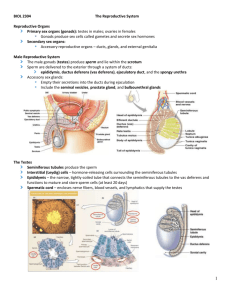
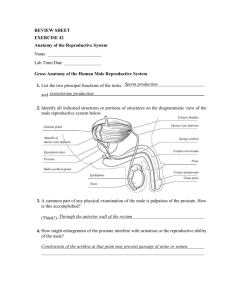
1 The Reproductive Systems Chapter 27 CHAPTER SUMMARY This chapter begins with a brief general introduction to the reproductive systems. The male reproductive system is considered separately from the female reproductive system. In the male reproductive system, the important characteristics of the scrotum, testes, ducts, accessory sex glands, semen, and penis are described. In the female reproductive system, the important characteristics of the ovaries, uterine (Fallopian) tubes, uterus, vagina, vulva, perineum, mammary glands, and the uterine and ovarian cycles are described. Birth control methods are explained. The development of the reproductive systems is portrayed. The effects of aging on the reproductive systems are described. A glossary of key medical terms associated with the reproductive systems is provided. This chapter concludes with a thorough study outline, an excellent self-quiz, critical thinking questions, and answers to questions that accompany chapter figures. STUDENT OBJECTIVES 1. Explain why, although they are very different from each other, both male and female reproductive systems produce gametes. 2. Describe the location, structure, and functions of the scrotum and testes. 3. Explain the principal events of spermatogenesis. 4. Describe the location, structure, and functions of the seminiferous tubules, straight tubules, rete testis, ductus epididymis (within the epididymis), ductus (vas) deferens (as a component of the spermatic cord), ejaculatory duct, and urethra as ducts of the male reproductive system. 5. Describe the location, structure, and functions of the accessory sex glands: seminal vesicles, prostate gland, and bulbourethral (Cowper’s) glands and explain the characteristics of semen. 6. Explain the structure and functions of the penis. 7. Describe the location, structure, and functions of the ovaries. 8. Explain the principal events of oogenesis. 9. Explain the location, structure, and functions of the uterine (Fallopian) tubes, uterus and vagina. 10. Describe the components of the vulva and explain their functions. 11. Explain the structure and functions of the mammary glands. 12. Describe the principal events of the ovarian and uterine cycles. 13. Compare the various kinds of birth control methods and their effectiveness. 14. Describe the development of the male and female reproductive systems. 15. Describe the effects of aging on the reproductive systems. LECTURE OUTLINE A. Introduction (p. 835) 1. Sexual reproduction is the process by which organisms produce offspring by means of germ cells called gametes; when a male gamete unites with a female gamete during fertilization, the resulting cell contains one set of chromosomes from each parent. 2. The organs of the reproductive systems may be grouped by function: i. gonads produce gametes and secrete sex hormones a. testes produce sperm cells b. ovaries produce ova ii. ducts receive, store, and transport gametes iii. accessory sex glands produce substances that protect gametes and facilitate their movement iv. supporting structures assist delivery and joining of gametes and, in females, the growth of the fetus during pregnancy 3. Gynecology is the medical specialty concerned with diagnosis and treatment of diseases of the female reproductive system; although urology is the study of the urinary system, urologists also diagnose and treat diseases and disorders of the male reproductive system. 2 B. Male Reproductive System (p. 836) 1. The male reproductive system includes: i. testes (male gonads), which produce sperm and secrete hormones ii. system of ducts, which stores and transports sperm to the exterior iii. accessory sex glands, which produce secretions that mix with sperm to form semen iv. supporting structures including the scrotum and penis 2. Scrotum: (p. 836) i. the scrotum is an outpouching of the abdominal wall consisting of loose skin and superficial fascia that hangs from the root of the penis ii. externally, it has a median ridge called a raphe which separates the pouch into two lateral portions iii. internally, it has a vertical scrotal septum that divides it into two sacs, each containing a single testis a. the septum consists of superficial fascia and smooth muscle tissue called the dartos muscle - dartos muscle is also found in the subcutaneous tissue of the scrotum - it causes wrinkling of the skin of the scrotum iv. the scrotum provides the testes with an environment that is about 2-3 degrees Celsius lower than core body temperature a. this lower temperature is essential for proper production and survival of sperm b. the cremaster muscle, a continuation of the internal oblique muscle, assists by elevating a testis on exposure to cold and during sexual arousal c. the dartos also contracts in response to cold to help assure the ideal temperature v. the scrotum receives blood from the internal pudendal branches of the internal iliac arteries, the cremasteric branches of the inferior epigastric arteries, and the external pudendal arteries from the femoral arteries; blood drains into scrotal veins that follow the arteries vi. the scrotal nerves are derived from the pudendal, posterior cutaneous of the thigh, and ilioinguinal nerves 3. Testes or testicles: (p. 837) i. the testes are paired oval glands which develop in the posterior portion of the embryo’s abdomen and usually begin their descent into the scrotum through the inguinal canals during the latter half of the seventh month of fetal development ii. the testes are partially covered by the tunica vaginalis a. this serous membrane covers a white fibrous capsule called the tunica albuginea; this capsule has inward extensions called septa which divide each testis into 200 to 300 lobules iii. each lobule contains one to three tightly coiled seminiferous tubules where spermatogenesis occurs a. seminiferous tubules are lined with spermatogenic cells in various stages of development; in order of advancing maturity, they are: 1. spermatogonia (which develop from primordial germ cells) line the periphery of the tubules 2. primary spermatocytes 3. secondary spermatocytes 4. spermatids 5. sperm cells or spermatozoa, located in the lumen b. embedded between the spermatogenic cells are sustentacular or Sertoli cells which extend from the basement membrane to the lumen - tight junctions between these cells form the blood-testis barrier which prevents an immune response against the spermatogenic cells - Sertoli cells perform several important functions: 1. support and protect developing spermatogenic cells 2. nourish spermatocytes, spermatids, and spermatozoa 3. phagocytize excess spermatid cytoplasm 4. control movements of spermatogenic cells and release of spermatozoa into the lumen 5. secrete fluid for sperm transport 6. secrete inhibin which decreases the rate of spermatogenesis c. between the seminiferous tubules are clusters of Leydig cells or interstitial endocrinocytes which secrete testosterone 3 d. spermatogenesis: - spermatogenesis takes about 65-75 days and involves the following sequence of events: 1. diploid spermatogonia, which develop from primordial germ cells, are stem cells which undergo mitosis 2. some of the daughter cells differentiate into diploid primary spermatocytes 3. primary spermatocytes undergo meiosis I which results in the formation of haploid secondary spermatocytes 4. the secondary spermatocytes undergo meiosis II which results in the formation of haploid spermatids which lie close to the lumen 5. spermatids undergo maturation, i.e., spermiogenesis, to form spermatozoa; the release of a spermatozoon from its connection to a Sertoli cell into the lumen is called spermiation - sperm migrate from the seminiferous tubules to the ductus epididymis where they complete their maturation and become capable of fertilizing an ovum; sperm are also stored in the ductus (vas) deferens where they may retain their fertility for up to several months - spermatozoa mature at a rate of about 300 million per day and, once ejaculated, have a life expectancy of about 48 hours within the female reproductive tract - each spermatozoon has several regions: 1. head, which contains the nucleus and an acrosome - the acrosome is a specialized lysosome that contains enzymes which aid penetration into the secondary oocyte (immature ovum) 2. tail, which consists of: - neck, which contains centrioles - middle piece, which contains numerous mitochondria that provide ATP for locomotion - principle piece, which is the longest portion of the tail - end piece, which is the terminal, tapering portion 4. Reproductive System Ducts in Males: (p. 843) i. in the testis, spermatozoa and fluid produced by the Sertoli cells move through the following sequence of ducts: a. seminiferous tubules b. straight tubules c. rete testis d. efferent ducts ii. efferent ducts carry the sperm out of the testis and into the tightly coiled ductus epididymis located within the epididymis (plural is epididymes) a. the epididymis is a cup-shaped organ located along the posterior border of each testis b. the epididymis has: 1. a large superior portion called the head where the efferent ducts join the ductus epididymis 2. narrow midportion called the body 3. smaller, inferior portion called the tail c. the ductus epididymis is lined by pseudostratified columnar epithelium having stereocilia which increase the surface area for reabsorption of degenerated spermatozoa - it is the site where sperm motility increases while sperm are being stored - during ejaculation, the smooth muscle layers in the wall of the ductus epididymis undergo peristaltic contractions to propel sperm into the ductus (vas) deferens iii. the ductus or vas deferens ascends from the tail of the epididymis along the posterior border of the epididymis, passes through the inguinal canal, and enters the pelvic cavity where it travels over the side and then down the posterior surface of the urinary bladder a. the dilated terminal portion of this duct is called the ampulla b. the ductus deferens is lined with pseudostratified columnar epithelium surrounded by three layers of smooth muscle tissue 4 c. it stores sperm and transports sperm from the epididymis into the ejaculatory duct during ejaculation by peristaltic contractions of its muscle layers iv. the ductus deferens delivers sperm to the ejaculatory duct which is located posterior to the urinary bladder a. each ejaculatory duct is formed by the union of the ductus deferens and the duct from the seminal vesicle b. just prior to ejaculation, sperm and secretions of the seminal vesicles are ejected from the ejaculatory ducts into the prostatic urethra v. the male urethra is a passageway for semen and urine; it consists of three regions: a. prostatic urethra passes through the prostate gland b. membranous urethra passes through the urogenital diaphragm, a muscular partition between the two ischial and pubic rami c. spongy (penile) urethra passes through the corpus spongiosum of the penis and ends at the external urethral orifice vi. alongside the ductus deferens, as it ascends through the scrotum, are: 1. testicular artery 2. autonomic nerves 3. veins that drain the testis 4. lymphatic vessels 5. cremaster muscle - these structures constitute the spermatic cord - the spermatic cord and ilioinguinal nerve pass through the inguinal canal which extends from the deep (abdominal) inguinal ring to the superficial (subcutaneous) inguinal ring 5. Accessory Sex Glands secrete most of the liquid portion of semen: (p. 847) i. two seminal vesicles or seminal glands: a. they are convoluted pouchlike structures located posterior to and at the base of the urinary bladder, and anterior to the rectum b. they secrete an alkaline, viscous fluid that contains fructose, prostaglandins, and clotting proteins c. this fluid is injected via two ducts into the ejaculatory ducts and it accounts for about 60% of the volume of semen ii. single prostate (gland): a. it is a doughnut-shaped gland located inferior to the urinary bladder and it surrounds the prostatic urethra b. it secretes a milky, slightly acidic fluid that contains several acids and several enzymes c. these secretions enter the prostatic urethra via many prostatic ducts and account for about 25% of the volume of semen iii. two bulbourethral or Cowper’s glands: a. they are pea-size glands located beneath the prostate gland on either side of the membranous urethra within the urogenital diaphragm b. they secrete an alkaline fluid that contains mucus into the spongy urethra via two ducts 6. Semen: (p. 847) i. semen is a mixture of sperm and seminal fluid, the secretions of the seminiferous tubules and accessory sex glands ii. it has the following notable features: a. the average volume that is ejaculated is 2.5 to 5 ml b. the average number of sperm cells is 50 to 150 million sperm per ml c. it provides sperm with a transportation medium and nutrients d. it has a slightly alkaline pH of 7.2 to 7.7 which neutralizes the acidic environment in the male urethra and the vagina e. it contains an antibiotic called seminalplasmin that destroys certain bacteria 5 7. Penis: (p. 848) i. the urethra of the penis delivers semen into the vagina (and excretes urine) ii. it consists of three regions: a. root of the penis, which consists of three major components: - bulb of the penis is the expanded base of the corpus spongiosum penis; it is attached to the inferior surface of the urogenital diaphragm and is enclosed by the bulbocavernosus muscle - crura of the penis are the separated and tapered portions of the corpora cavernosa penis; each crus is attached to the ischial and inferior pubic rami and surrounded by the ischiocavernosus muscle b. body of the penis, which contains three cylindrical masses of erectile tissue covered by fibrous tissue called the tunica albuginea; the three cylindrical masses are: - two dorsolateral corpora cavernosa penis or corpora cavernosa - one smaller midventral corpus spongiosum penis or corpus spongiosum which contains the spongy urethra - sexual excitation causes large volumes of blood to enter their blood sinuses, resulting in erection which is a parasympathetic reflex - prior to ejaculation, emission discharges a small volume of semen - ejaculation, the propulsion of semen from the urethra to the exterior, is a sympathetic reflex c. glans penis, which is the slightly enlarged distal end of the corpus spongiosum penis - the margin of the glans penis is the corona - the distal urethra enlarges within the glans penis and forms a terminal slitlike opening, the external urethral orifice - encircling the glans penis is the loosely fitting prepuce or foreskin iii. The weight of the penis is supported by the fundiform ligament and the suspensory ligament of the penis. iv. the penis receives blood from the internal pudendal and femoral arteries; blood drains into corresponding veins v. the penis is innervated by branches of the pudendal and ilioinguinal nerves; parasympathetic stimulation results in erection whereas sympathetic stimulation results in ejaculation C. Female Reproductive System (p. 851) 1. The female reproductive system includes: i. ovaries, which produce secondary oocytes (cells that develop into mature ova only after fertilization) and several hormones ii. uterine (Fallopian) tubes or oviducts, which transport secondary oocytes and ova to the uterus iii. uterus, in which embryonic and fetal development occur iv. vagina, which leads from the exterior to the uterus v. vulva or pudendum, the external genital organs vi. mammary glands, which produce milk 2. Ovaries: (p. 852) i. the ovaries are homologous to the testes ii. the ovaries are located in the pelvic cavity, one on each side of the uterus iii. each ovary is held in position by a series of ligaments: a. broad ligament of the uterus attaches to each ovary by the mesovarium b. ovarian ligament anchors each ovary to the uterus c. suspensory ligament attaches each ovary to the pelvic wall iv. each ovary has a hilus where blood vessels and nerves enter/exit and along which the mesovarium is attached v. histology; each ovary consists of the following components: a. germinal epithelium which covers the surface of the ovary b. tunica albuginea, a capsule of dense connective tissue located under the germinal epithelium c. ovarian cortex which consists of dense connective tissue and contains ovarian follicles 6 d. ovarian medulla which consists of loose connective tissue and contains blood vessels, lymphatics, and nerves e. ovarian follicles, consisting of oocytes in various stages of development and their surrounding epithelial cells; the latter are called follicular cells when they form a single layer, and are called granulosa cells when they form several layers f. mature (Graafian) follicle, a large fluid-filled follicle which will rupture and expel a secondary oocyte in a process called ovulation g. corpus luteum, a remnant of the mature (Graafian) follicle that has ruptured; it secretes several hormones until it degenerates into a mass of fibrous tissue called a corpus albicans vi. the ovaries receive blood from the ovarian arteries, which anastomose with branches of the uterine arteries; blood drains into the ovarian veins vii. the ovaries are innervated by vasomotor sympathetic and parasympathetic nerve fibers viii. oogenesis: a. the formation of gametes in the ovaries occurs via oogenesis b. oogenesis involves meiosis: 1. meiosis I - diploid oogonia, which develop from primordial germ cells, divide mitotically during early fetal development to produce millions of germ cells; before birth, many of the latter degenerate via atresia - a few develop into larger cells called primary oocytes that enter prophase of meiosis I during fetal development but do not complete this phase until after puberty - at birth 200,000 to 2,000,000 oogonia and primary oocytes remain in each ovary, of which about 40,000 remain at puberty and only 400 will mature and ovulate during a woman’s reproductive years; the remainder will undergo atresia - each primary oocyte is surrounded by a single layer of follicular cells; the entire structure is called a primordial follicle - periodically, several primordial follicles start to grow and become primary follicles that are initially surrounded by a layer of follicular cells and subsequently by 6-7 layers of granulosa cells - as the follicle grows, it forms a clear glycoprotein layer called the zona pellucida between the primary oocyte and the granulosa cells - the innermost layer of granulosa cells is called the corona radiata; the outermost granulosa cells form the theca folliculi - the theca differentiates into the theca interna and the theca externa - the granulosa cells begin to secrete follicular fluid into a cavity called the antrum within the follicle; the follicle is now called a secondary follicle - during childhood, primordial and developing follicles continue to undergo atresia - after puberty, under the influence of gonadotropic hormones, meiosis I resumes each month in several secondary follicles but only one will reach maturity; the diploid primary oocyte completes meiosis I to form two hapoid cells: - small first polar body - large secondary oocyte, which proceeds to the metaphase stage of meiosis II - the follicle in which this occurs, called a mature (Graafian) follicle, will soon rupture and release its secondary oocyte in a process called ovulation 2. meiosis II - at ovulation, usually one secondary oocyte (with the first polar body and corona radiata) is discharged into the pelvic cavity and enters the uterine (Fallopian) tube - if fertilization does not occur, the secondary oocyte degenerates 7 - if fertilization does occur, meiosis II resumes and the secondary oocyte divides into two haploid cells: - a larger cell called the ovum (or mature egg) whose nucleus unites with the sperm nucleus, forming a diploid zygote - a smaller cell called the second polar body; the first polar body may also undergo meiosis II to produce two polar bodies - all polar bodies will degenerate - Table 27.1 summarizes the events of oogenesis and follicular development 3. Uterine (Fallopian) tubes or oviducts: (p. 856) i. the two uterine tubes extend laterally from the uterus and transport secondary oocytes and fertilized ova from the ovaries to the uterus ii. the open, funnel-shaped lateral portion of each tube is called the infundibulum and is located close to the ovary iii. the infundibulum is encircled by a fringe of fingerlike fimbriae; one fimbria is attached to the lateral end of the ovary iv. the medial end of the uterine tube attaches to the superior lateral angle of the uterus v. the uterine tube has two main portions: a. lateral two-thirds is the ampulla, which is the widest, longest portion b. medial portion is the isthmus, which is the short, narrow, thick-walled portion that joins the uterus vi. the wall of the uterine tube consists of three layers: a. inner mucosa, which contains: - ciliated columnar epithelial cells which help, via ciliary action, to move the fertilized ovum or secondary oocyte along the tube - secretory cells which may provide nutrition to the ovum b. middle muscularis, which consists of: - inner circular ring of smooth muscle tissue - outer longitudinal region of smooth muscle tissue - peristaltic contractions of the muscularis help move the oocyte or fertilized ovum toward the uterus c. outer serosa, which is a serous membrane vii. after ovulation and entry of the secondary oocyte into the uterine tube, fertilization (if it occurs) typically occurs in the ampulla, resulting in the formation of a zygote; after several cell divisions, the early embryo typically arrives at the uterus about 7 days after ovulation viii. the uterine tubes receive blood from branches of the uterine and ovarian arteries; blood drains into the uterine veins ix. the uterine tubes are innervated by sympathetic and parasympathetic nerve fibers from the hypogastric plexus and the pelvic splanchnic nerves; the fibers are distributed to the blood vessels and muscularis of the uterine tubes 4. Uterus (womb): (p. 858) i. the uterus is the site of the following major events: a. pathway for sperm to enter the uterine tubes b. menstruation c. implantation of an early embryo d. development of the fetus during pregnancy e. labor ii. the uterus is located between the urinary bladder and the rectum, and it resembles an inverted pear iii. the uterus consists of several major regions: a. fundus, the dome-shaped region above the uterine tubes b. body, the major tapering central portion c. cervix, the lower narrow portion that opens into the vagina 8 d. between the body and the cervix is a constricted region called the isthmus - at this location, anteflexion causes the body to project anteriorly and superiorly over the urinary bladder while the cervix projects inferiorly and posteriorly to enter the anterior wall of the vagina at nearly a right angle; a posterior tilting (malposition) of the uterus is called retroflexion e. the interior of the body contains the uterine cavity f. the interior of the cervix contains the cervical canal g. the cervical canal opens into the uterine cavity at the internal os h. the opening of the cervical canal into the vagina is the external os iv. the uterus is held in position by several pairs of ligaments: a. broad ligaments attach the uterus to either side of the pelvic cavity b. uterosacral ligaments attach the uterus to the sacrum c. cardinal (lateral cervical) ligaments extend below the bases of the broad ligaments between the pelvic wall and the cervix and vagina d. round ligaments extend from the uterus to a portion of the labia majora of the external genitals v. the wall of the uterus consists of three layers of tissue: a. outer perimetrium (serosa), which is part of the visceral peritoneum - laterally, it becomes the broad ligament - anteriorly, it covers the urinary bladder and forms a shallow pouch called the vesicouterine pouch - posteriorly, it covers the rectum and forms a deep pouch called the rectouterine pouch (pouch of Douglas) b. middle, thick myometrium - it consists of three layers of smooth muscle tissue and is thickest in the fundus and thinnest in the cervix - during labor and childbirth, coordinated contractions help expel the fetus c. inner, highly vascular endometrium - it consists of two layers: 1. inner stratum functionalis (functional layer), which is shed during menstruation 2. outer stratum basalis (basal layer), a permanent layer that gives rise to a new stratum functionalis after each menstruation - the mucosa of the cervix produces cervical mucus which, among other roles, may play a role in capacitation of sperm cells vi. the uterus receives blood from the uterine arteries which branch progressively to form arcuate arteries (in the myometrium), radial arteries (deep into the myometrium), straight arterioles (in the stratum basalis), and spiral arterioles (in the stratum functionalis); blood drains into the uterine veins 5. Vagina: (p. 861) i. the vagina has several major roles: a. it is a passageway for menstrual flow b. it is a passageway for childbirth c. it receives semen from the penis during sexual intercourse ii. it is located between the urinary bladder and the rectum iii. a recess called the fornix surrounds the vaginal attachment to the cervix iv. it has a mucosa with rugae v. the mucosa stores glycogen which subsequently decomposes into organic acids that create an acidic environment; the acidity retards microbial growth, but is also harmful to sperm cells vi. it has a muscularis composed of smooth muscle tissue that can stretch considerably to accommodate the penis during sexual intercourse and permit birth of a child vii. it has an outer adventitia which anchors the vagina to neighboring organs. viii. the vaginal orifice may be encircled by a thin fold of vascularized mucous membrane called the hymen (an imperforate hymen completely covers the orifice); the hymen is easily torn and destroyed by the first sexual intercourse 9 6. Vulva or pudendum (or external genitals of the female): (p. 862) i. the vulva has several major components: a. mons pubis, which is an elevation of adipose tissue covered by skin and pubic hair; it is located anterior to the vaginal and urethral openings and serves to cushion the pubic symphysis b. labia majora, which are two longitudinal folds of skin that extend inferiorly and posteriorly from the mons pubis; they are covered by pubic hair and contain adipose tissue, sebaceous glands, and sudoriferous glands c. labia minora, which are two smaller folds of skin located medial to the labia majora; they have some sudoriferous glands and many sebaceous glands d. clitoris, which is a small cylindrical mass of erectile tissue and nerves located at the anterior junction of the labia minora; the body of the clitoris is covered by a layer of loose skin called the prepuce; the exposed part of the clitoris is called the glans e. vestibule, which is the cleft between the labia minora; the vaginal orifice occupies most of the vestibule f. the bulb of the vestibule consists of two elongated masses of erectile tissue just deep to the labia on either side of the vaginal orifice ii. the external urethral orifice is located anterior to the vaginal orifice and posterior to the clitoris iii. lateral to the external urethral orifice are the openings of the ducts of the paraurethral (Skene’s) glands which secrete mucus iv. lateral to the vaginal orifice are the greater vestibular (Bartholin’s) glands which open by ducts into a groove between the hymen and labia minora; they secrete mucus v. several lesser vestibular glands also open into the vestibule - Table 27.2 provides a summary of the homologous structures of the female and male reproductive systems 7. Perineum: (p. 863) i. the perineum is the diamond-shaped area medial to the thighs and buttocks of both males and females that contains the external genitals and anus ii. it is bounded anteriorly by the pubic symphysis, laterally by the ischial tuberosities, and posteriorly by the coccyx iii. a transverse line drawn between the ischial tuberosities divides the perineum into: a. anterior urogenital triangle, which contains the external genitals b. posterior anal triangle, which contains the anus 8. Mammary Glands: (p. 864) i. the two mammary glands are modified sudoriferous glands that secrete milk ii. they are located anterior to the pectoralis major and serratus anterior muscles and are attached to them by a layer of dense irregular connective tissue iii. each mammary gland consists of 15 to 20 lobes that are separated by adipose tissue; the size of the breast is determined by the amount of adipose tissue that is present iv. each lobe consists of smaller compartments called lobules v. lobules are composed of connective tissue containing grapelike clusters of milk-secreting glands called alveoli; surrounding the alveoli are myoepithelial cells whose contractions help propel milk vi. when milk is produced, it flows from alveoli into secondary tubules which converge to form mammary ducts vii. mammary ducts deliver milk to lactiferous sinuses where milk may be stored viii. lactiferous ducts deliver milk from the lactiferous sinuses to the nipple, a pigmented projection ix. surrounding the nipple is a circular pigmented area called the areola; the areola has a rough appearance because it contains modified sebaceous glands x. strands of connective tissue called the suspensory ligaments of the breast (Cooper’s ligaments) extend between the skin and deep fascia and support the breast naturally xi. the functions of the mammary glands are milk synthesis, secretion, and ejection, which are collectively termed lactation; milk production is stimulated primarily by prolactin, and milk ejection is stimulated by oxytocin D. Female Reproductive Cycle (Uterine and Ovarian Cycles) (p. 867) 1. The ovarian cycle is a series of events associated with maturation of a secondary oocyte. 2. The uterine (menstrual) cycle is a series of changes in the endometrium. 10 3. The general term female reproductive cycle cycles includes the ovarian and uterine cycles, the hormonal changes that regulate them, and the cyclical changes in the breasts and cervix. 4. The ovarian and uterine cycles are controlled by gonadotropin releasing hormone (GnRH) which stimulates release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). 5. The duration of the female reproductive cycle normally ranges from 24 to 35 days; it may be divided into four events: i. menstrual phase or menstruation or menses a. this phase lasts for roughly the first 5 days of the cycle b. in the ovaries, about 20 secondary follicles begin to enlarge due to accumulation of follicular fluid in the antrum c. in the uterus, the entire stratum functionalis sloughs off resulting in the discharge of menstrual flow through the vagina to the exterior ii. preovulatory phase a. this phase is variable in length but generally lasts from days 6 to 13 in a 28-day cycle b. in the ovaries, one of the developing secondary follicles becomes the dominant follicle and matures into a mature (Graafian) follicle; it continues to enlarge and forms a blisterlike bulge on the surface of the ovary - with reference to the ovarian cycle, the menstrual and preovulatory phases together are termed the follicular phase c. in the uterus, cells of the stratum basalis undergo mitosis to produce a new stratum functionalis - with reference to the uterine cycle, the preovulatory phase is also called the proliferative phase iii. ovulation a. the mature (Graafian) follicle ruptures and the secondary oocyte (with its surrounding zona pellucida and corona radiata) is released into the pelvic cavity b. this event usually occurs on day 14 in a 28-day cycle and is triggered by a surge in LH secretion c. the remnants of the mature follicle develop into a corpus hemorrhagicum and subsequently into a corpus luteum which secretes progesterone, estrogens, relaxin, and inhibin iv. postovulatory phase a. this phase lasts from days 15 to 28 in a 28-day cycle b. if fertilization does occur, the corpus luteum is maintained by human chorionic gonadotropin (hCG) that is secreted by the chorion of the embryo (until the placenta takes over its hormonesecreting functions) - with reference to the ovarian cycle, this phase is also called the luteal phase c. in the uterus, there is a growth of endometrial glands, vascularization and thickening of the endometrium, and an increase in the amount of tissue fluid; these events occur in preparation for the possible implantation of a developing embryo - with reference to the uterine cycle, this phase is called the secretory phase d. if fertilization does not occur, the corpus luteum degenerates into a corpus albicans; the resulting decline in progesterone and estrogen secretion causes menstruation E. Birth Control Methods (p. 869) 1. The only birth control method that is 100% reliable is total abstinence. 2. Other methods include: (see Table 27.3 for a list of failure rates of several birth control methods) i. surgical sterilization a. vasectomy b. tubal ligation ii. hormonal methods, i.e., using oral contraceptives (“the pill”) and other related methods iii. intrauterine device (IUD) iv. spermicides v. barrier methods a. condom 11 b. vaginal pouch c. diaphragm vi. periodic abstinence a. rhythm method b. sympto-thermal method vii. coitus interruptus viii. induced abortion F. Development of the Reproductive Systems (p. 871) 1. The gonads develop from the intermediate mesoderm as bulges that protrude into the ventral body cavity near the mesonephric (Wolffian) ducts; paramesonephric (Mullerian) ducts develop lateral to the mesonephric ducts. 2. An early embryo contains primitive gonads capable of developing into either testes or ovaries; the presence or absence of the SRY gene on the Y chromosome, which results in the presence or absence of Mullerianinhibiting substance (MIS) and consequently the release or absence of testosterone, determines whether the embryo will develop into a male or female, respectively; at about the eighth week of embryological development, the gonads are clearly differentiated into ovaries or testes. 3. In the male embryo: i. the testes connect to the mesonephric ducts through a series of tubules that become the seminiferous tubules ii. the mesonephric duct on each side develops into: a. epididymis b. ductus (vas) deferens c. ejaculatory duct d. seminal vesicle iii. endodermal outgrowths of the urethra develop into the prostate gland and the bulbourethral (Cowper’s) glands iv. the paramesonephric ducts degenerate 4. In the female embryo: i. the gonads develop into ovaries ii. the distal ends of the paramesonephric ducts fuse to form the uterus and vagina; the unfused portions become the uterine (Fallopian) tubes iii. endodermal outgrowths of the vestibule develop into the greater (Bartholin’s) and lesser vestibular glands iv. the mesonephric ducts degenerate 5. The external genitals in both male and female embryos develop from an elevation called the genital tubercle which consists of: i. urethral groove ii. two urethral folds iii. two labioscrotal swellings 6. In the male embryo, some testosterone is converted into dihydrotestostserone (DHT) which stimulates development of the urethra, prostate and external genitals: i. part of the genital tubercle elongates and develops into a penis ii. the urethral folds fuse to form the spongy (penile) urethra with an external urethral orifice iii. the labioscrotal swellings develop into the scrotum 7. In the female embryo: i. the genital tubercle develops into the clitoris ii. the urethral folds remain open as the labia minora iii. the labioscrotal swellings develop into the labia majora iv. the urethral groove develops into the vestibule 12 G. Aging and the Reproductive Systems (p. 874) 1. Puberty is the period of time when secondary sexual characteristics begin to develop and the potential for sexual reproduction is reached. 2. In females, the reproductive cycle normally occurs once each month from menarche (the first menses) to menopause (the permanent cessation of menses); menopause is often accompanied by a number of symptoms as well as atrophy of the organs that comprise the female reproductive system; cancers of reproductive organs may occur. 3. In males, reproductive capacity does not usually diminish to any significant extent; however, other changes including benign prostatic hyperplasia (BPH) commonly occur; cancer of the prostate gland may sometimes develop. H. Key Medical Terms Associated with the Reproductive Systems (p. 878) 1. Students should familiarize themselves with the glossary of key medical terms.