In Patients with Gastroesophageal Reflux Disease is Esomeprazole
advertisement

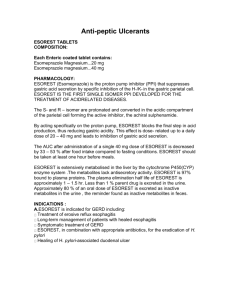
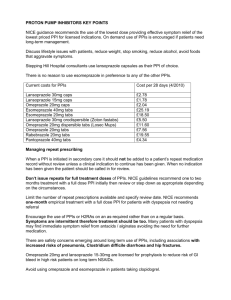
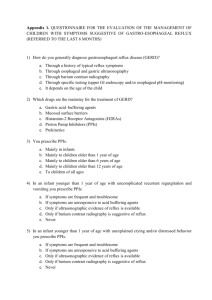
In Patients with Gastroesophageal Reflux Disease is Esomeprazole the most Effective Proton Pump Inhibitor to Induce and to Maintenance of Mucosal Healing? A Systematic Review and Meta-Analysis Ana Lopes (ana_cplopes@hotmail.com); Andreia Pinto (muifilipa@hotmail.com); Catarina Melo (clmelo@sapo.pt); Diogo Dias (diogo.diaz@hotmail.com); Isabel Saavedra (ixabeu_xaavedinhah@hotmail.com); João Matias (joaomatias1@gmail.com); Mariana Ferreira (yellowg_2@hotmail.com); Mariana Mangas (mariana_mangas@hotmail.com); Paula Neves (paula_lotrfan@hotmail.com); Rita Sapage (rita.sapage@hotmail.com); Rui Coelho (rui_pc_coelho@hotmail.com); Teresa Caridade (teresacaridade@msn.com); Teresa Tavares (teresa_tavares5@hotmail.com) Doctor Mário Dinis Ribeiro, Class 16 ABSTRACT Introduction and Aim: Gastroesophageal reflux disease (GERD) is a chronic disease, which impairs quality of life and has a high tendency to relapse, requiring a long term treatment strategy. The pharmacological management of patients with GERD aims both to provide oesophageal healing and induce symptom relief. Proton pump inhibitors (PPIs) are the current mainstay therapy, with Esomeprazole being the most recent. Several studies focus potential discrepancies in efficacy among the different PPIs used for treatment of GERD. The aim of this work is to compare efficacy of esomeprazole in inducing and maintenance of mucosal healing in GERD patients, relatively to other PPIs (omeprazole, lansoprazole, rabeprazole and pantoprazole). Methodology: A systematic review and a metanalysis of RCT studies are performed. MEDLINE, SCOPUS and ISI Web of Knowledge controlled trials register were searched up to December 2007. Clinical trials focused on Human adults treated with PPIs were selected.The primary outcome of interest was inducing mucosal healing to a specific PPI. Information on study design, participant characteristics, interventions, and results were also extracted. Results: 12 trials were eligible in this study. 6 studies compared esomeprazole 20 mg with omeprazole 20mg, lanzoprazole 15mg, rabeprazole 10mg and pantoprazole 20mg; while other 6 compared esomeprazole 40mg versus omeprazole 20mg, lanzoprazole 30mg and pantoprazole 40 mg. A meta-analysis of mucosal healing of esomeprazole 40mg compared with standard dose PPIs, at 8 weeks, gave a relative risk (RR) of 1.57 and a 95% Confidence Interval (CI): 1.41 - 1.76. To esomeprazole 20mg, at 24 weeks, the results were the following: RR 1.75; 95% CI 1.49 – 2.04. Conclusions: As compared with other PPIs, esomeprazole appears to be the most effective Proton Pump Inhibitor in inducing and maintenance of mucosal healing. KEY-WORDS: Gastroesophageal Reflux Disease, Bile Reflux, Esophageal Motility Disorders, esomeprazole, systematic review, esophagitis, Proton Pump Inhibitor. INTRODUCTION Gastroesophageal reflux disease (GERD) is a prevalent and chronic condition in which reflux of the stomach contents into the oesophagus causes a range of troublesome symptoms (including heartburn and acid regurgitation) and complications 1. Such symptoms can cause marked disruption of physical, social and emotional well-being 2, 3 with possible long-term complications of GERD including reflux oesophagitis, haemorrhage, stricture, Barrett’s oesophagus and adenocarcinoma of the distal oesophagus 1, 4. Heartburn, the most characteristic symptom of GERD, affects an estimated 20–40% of Western populations, with approximately 7% experiencing daily symptoms 5. In Portugal 35% of Portuguese adults refer GERD symptoms6. The prevalence of the disease tends to be underestimated, with unrecognised GERD occurring in >50% of patients seen in general practice for unrelated conditions 5. In fact, GERD is the most common condition encountered by pediatric and adult gastroenterologists. The pharmacological management of patients with GERD aims to provide symptom relief, improved quality of life and protection from long-term complications 7. A number of drugs are registered for GERD treatment, mainly: antacids, alginic acid, Histamine H2-receptor antagonists, prokinetics, sucralfate and proton pump inhibitors. Proton pump inhibitors (PPIs) are the mainstay of medical therapy in gastroesophageal reflux disease. The site of action of the PPIs is the gastric acid pump (H+/K+ ATPase), which is the final common pathway for acid secretion in the stomach. PPIs are a highly effective therapy for GERD and its complications, and are the agents of choice for the suppression of gastric acid production 5. They produce significantly faster and more complete relief of heartburn symptoms than H2RAs, as well as healing erosive GERD significantly faster and with higher rates after 4 and 8 weeks of treatment 5. PPIs also have more convenient dosing than most H2RAs; the approved standard dose of PPIs for GERD treatment being once-daily. In addition to symptomatic relief of heartburn, PPIs heal esophageal mucosal injury and reduce the need for frequent dilatation in patients with peptic stricture. PPIs are highly selective and effective in their action and have few short- or long-term adverse effects 7. Currently, five PPIs are available on the market: omeprazole, lansoprazole, rabeprazole, pantoprazole, and esomeprazole. Although all PPIs have the same general mechanism of action, the nature of the pyridine and benzimidazole substituents may confer physical and chemical differences and differ in their clinical pharmacology. Esomeprazole, the S-isomer of omeprazole, is the new-generation PPIs and it has been suggested it has superior pharmacologic and clinical effects compared with its racemic parent compound. Moreover, some authors suggested that its administration offers several pharmacokinetic advantages relatively to first generation PPIs. In subgroups, such as severe esophagitis, esomeprazole may be more efficient than others PPIs 8. Quite the opposite, others authors demand advantages in the use of old PPIs. Glatzel and colleagues demonstrate that pantoprazole 40 mg was at least as effective as esomeprazole 40 mg for relieving GERD symptoms and during the post treatment phase, patients on pantoprazole had a significantly lower risk to relapse and experienced significantly fewer symptom episodes 9. In fact, despite PPI increasing use, up to 40% of patients are not fully satisfied with their antireflux therapy 8. Recent data on efficacy and safety are reviewed and causes of failure are discussed. Several randomized studies dated until December 2007, have shown marginal differences in efficacy between various proton pump inhibitor regimens. While reports of treatment efficacy from clinical trials and qualitative reviews can guide clinical decision-making, metanalysis reviews allow for an objective assessment of the overall magnitude of treatment effects across a number of tests of treatment efficacy 10. Currently, there are only eighteen metanalyses about GERD, and only a few guide PPI treatment recommendations. Although all PPIs have the same general mechanism of action, they have physical and chemical differences; differences between them should be considered when choosing a treatment regimen. RESEARCH QUESTION In patients with Gastroesophageal Reflux disease is Esomeprazole the most efficient Proton Pump Inhibitor to induce and maintain mucosal healing? AIM The aim of this work is to use a systematic review to compare the efficacy of esomeprazole in inducing and maintenance of mucosal healing in GERD patients, relatively to oldest PPIs, omeprazole, lansoprazole, rabeprazole and pantoprazole. PARTICIPANTS AND METHODS The systematic review is a gliding revision to answer to a specific question and it uses explicit and systematic methods critically to identify, select and to evaluate the studies. It also collect and analyze the data of these enclosed studies in the revision. This method involves some different stages: 1- Literature Search Strategy An extensive literature search was conducted in PubMed, ISI Web of Knowledge and SCOPUS from the first available year to December 2007. Searches were made using the following queries, respectively to databases PubMed, ISI Web of Knowledge and SCOPUS: (gastroesophageal "Gastroesophageal reflux OR Reflux"[Mesh non-esophagitis ] OR GERD OR NERD OR reflux esophagitis disease OR) AND (regurgitation OR heartburn) AND (randomized controlled trial[Publication Type ] OR (randomized[Title/Abstract ] AND controlled[Title/Abstract ] AND trial[Title/Abstract ])) AND (omeprazole OR "Omeprazole"[Mesh ] OR pantoprazole OR "pantoprazole"[Substance Name ] OR rabeprazole OR "rabeprazole"[Substance Name ] OR lansoprazole OR "lansoprazole"[Substance Name ]) AND (esomeprazole OR "Omeprazole"[Mesh ]) NOT ("Barrett esophagus" [ Mesh ]) ((gastroesophageal reflux OR GERD OR NERD OR non-esophagitis reflux disease OR esophagitis) AND (regurgitation OR heartbun) AND (omeprazole OR pantoprazole OR rabeprazole OR lansoprazole) AND (esomeprazole) NOT (Barrett Syndrome)) ((gastroesophageal reflux OR gerd OR nerd OR non-esophagitis reflux disease OR esophagitis) AND (regurgitation OR heartbun) AND (omeprazole OR pantoprazole OR rabeprazole OR lansoprazole) AND (esomeprazole) AND NOT (barrett syndrome)) AND (EXCLUDE(DOCTYPE, "re") OR EXCLUDE(DOCTYPE, "cp")) 2 - Study Inclusion and exclusion Criteria Each study selected for inclusion was original articles and clinical trials, focused on Human adults (18 – 75 years) that were treated only with PPIs. Additionally, exclusion criteria were: previous articles to the launching of esomeprazole, articles published from December of 2007, studies in pregnant, studies in people with other illnesses beyond GERD. 3- Extraction and Data Processing When analyzing each article, the type of study, methodology adopted, it aims and results, and the type of PPI used were data considered. The number of initial participants of the study and the amount of people who had abandoned it (as well as the reasons that had taken them to live) was listed. The characteristics of the participants, as the ethnia, age, sex and physiological state (example, gestation, menopause), their daily habits, their symptoms and the other medication taken (beyond PPI) were also data analyzed. Two reviewers code all studies for intervention and statistical information; all of the intervention and outcome data was compared for consistency. 4 - Quality assessment A quality evaluation was done to explain the difference of results between the studies and the reason why they are excluded (quality scales). To do this CONSORT statement was used, which is an evidence-based, minimum set of recommendations for reporting RCTs. CONSORT statement comprises a 22-item checklist and a flow diagram, along with some brief descriptive text. The checklist items focus on reporting how the trial was designed, analyzed, and interpreted; the flow diagram displays the progress of all participants through the trial. 5 - Statistical Analysis Data collected was analyzed and submitted to Statistical Package for Social Sciences (SPSS). SPSS is a modular, tightly integrated, full-featured product line for the analytical process-planning, data collecting, data access, data management and preparation, data analysis, reporting, and deployment. In addition to statistical analysis, SPSS allow data management (case selection, file reshaping, creating derived data) and data documentation. In addition Review Manager (RevMan), a specific software for metanalysis, was used. RevMan allows to enter protocols, as well as complete reviews, including text, characteristics of studies, comparison table, and study data. It can perform meta-analysis of the data entered, and present the results graphically. This software allows to calculate the relative risk (RR) with 95% confidence intervals (95% CI), where a confidence interval that crosses the value 1.00 indicates no statistically significant difference in treatment effects. A value >1.00 shows a benefit to Esomeprazole while a value <1.00 shows a benefit for the comparator PPI. 5.1 - Analysis of data, heterogeneity and setbacks of publication Concluding on measures of effect (average, relative risk...), applying a quantitative synthesis of evidence through the goal-analysis, identifying heterogeneities causes that cannot be explained by the variability of the sample. RESULTS Study selection Figure 1. Results of a search on Pubmed, ISI Web of Knowledge and SCOPUS for RCT comparing Esomeprazole with other PPIs. Figure 1 shows the process of study selection. Using the queries defined previously to databases Pubmed, ISI Web of Knowledge and SCOPUS, 158, 35 and 57 articles were available, respectively, becoming a total of 250 articles. Of these, initially 28 articles had been excluded as duplicates and after a pre-selection 115 articles were excluded because did not fulfill the explicit requirements of inclusion criteria, mainly because clinical trials didn’t compare Esomeprazole with other PPI. From the 99 included, 33 articles were not found published in full. After this pre-selection, the abstract of each one of the 66 articles was read and selected, in accordance with the exclusion and inclusion criteria, by two elements of the group (reviewers). This process resulted in the reduction of the included article number to 12. Study characteristics The 12 articles selected were considered to be of sufficient quality to have data extracted for inclusion in the analyses. Six studies compared esomeprazole 20 mg with different doses of omesoprazole, lanzoprazole, rabeprazole and pantoprazole. Other six studies comparing esomeprazole 40 mg with distinct doses of omeprazole, lanzoprazole and pantoprazole were eligible for this systematic review (Table 1). Eighteen different outcomes were measured across the domains of interest. Remission rate was the domain from which mucosal healing was most frequently determined. Table 1. Characteristics of RCTs reporting on the use of PPIs for prevention of mucosal healing. Comparation group Number of participants Age of participants (min-max) Duration of treatment (weeks) Dose of other PPI (mg/day) Results (Esomeprazole/PPI) (%) 1960 - 8 20 90/87 1391 >18* 24 15 85/75 774 [18,80] 24 15 93/88 134 [25,65] 4 10 88/96 236 [39;57] 24 20 79/68 1452 >19* 24 20 Esomeprazole 20mg vs. omeprazole vs. lansoprazole vs. rabeprazole vs.pantoprazole Kahrilas PJ et al 200011 Lauritsen K et al 2003 12 Tsai HH et al 2004 13 Fock KM et al 2005 14 Scholten T et al 2003 15 Goh KL et al 2007 16 85/84 Esomeprazole 40mg vs omeprazole Chen CY et al 48 [36,72] 8 2005 17 Richter JE et al 2425 [18,75] 8 2001 18 Schmitt C et al 1946 [18,75] 8 2006 19 vs lansoprazole Fennerty MB et 4015 [18,75] 8 al 2005 20 Castell DO et al 5241 [18,75] 8 2002 21 vs pantoprazole Labenz J et al 3170 50,6** 8 2005 22 * in these studies, the maximum value was not fixed. ** in this study, the mean of the ages of the participants was the variable considerate. 20 72/50 20 94/84 20 87/86 30 78/73 30 93/89 40 92/89 Data analysis Data for standard dose PPIs were combined and compared with esomeprazole. To analyze the feature “healing”, studies with treatment duration of 8 weeks were considered. The feature “maintenance” was examined in the studies of 24 weeks. Because the reduced number of articles that compare esomeprazole 20 mg vs. old PPIs during 8 weeks (only one), and the inexistence of studies that compare esomeprazole 40 mg vs. old PPIs in a treatment of 24 weeks, theses analyzes were not done. Relative efficacy of Esomeprazole 40 mg in Healing To discuss healing, Esomeprazole 40 mg was compared with Lanzoprazole, Omeprazole and Pantoprazole in treatment duration of 8 weeks (Fig. 2). Six studies were considered and RR ranged between 1.10 and 2.36. 95% CIs for most studies are extensive, reflecting to some extent the small sample sizes. Analyses show that Esomeprazole is more efficient in mucosal healing although there is only a significant difference when compared with pantoprazole (Fig. 3). Test for heterogeneity is statistical significative (p<0.00002) which may be for the reason of the reduced number of articles analyzed (Fig. 2). Figure 2. Relative risk (RR with 95% confidence intervals) of mucosal healing of Esomeprazole 40 mg vs. standard doses of old PPIs. Relative efficacy of Esomeprazole 20 mg in Maintenance Esomeprazole 20 mg was compared with Lanzoprazole and Pantoprazole (Fig. 3). Four studies were compared and RR ranged between 1.21 and 3.06. 95% CIs for most studies are extensive, reflecting to some extent the small sample sizes. In this analyze test of heterogeneity is statistical significative, p=0.00001 (Fig. 3). This result may result of the limited number of articles evaluated. Results obtained with RevMan show that Esomeprazole is more efficient in maintenance of mucosal healing. Results, when compared with Lanzoprazole, are that Esomeprazole is statistically significative more effective in the maintenance of mucosal healing. There are no statistical significative differences between esomeprazole and pantoprazole, however the new generation PPI tends to be better. Figure 3. Relative risk (RR with 95% confidence intervals) of mucosal maintenance of Esomeprazole 20 mg vs. standard doses of old PPIs. . DISCUSSION GERD is a major healthcare problem in the adult population and has a significant negative impact on patient quality of life and long- term complications. A number of PPIs have been approved for the treatment of these conditions. Esomeprazole is the most recent PPI and its efficacy has been object of many discussions. Some authors support it superiority relatively to older PPIs whereas others demand advantages in the use of older PPIs. These discrepancies lead us to analyse and compare the efficacy of esomeprazole in inducing and maintenance of mucosal healing in GERD patients relatively to omeprazole, lansoprazole, rabeprazole and pantoprazole. This meta-analysis showed a significant benefit in favour of esomeprazole at 8 and 24 weeks relatively to pantoprazole and lansoprazole, respectively. Comparatively to omeprazole, results are not statistical significative but apparently there is a tendency to esomeprazole be more effective in healing of mucosal healing. Unfortunately there are no articles comparing rabeprazole and esomeprazole in the healing and maintenance of mucosal healing. However, it should be noted that a previous review demonstrated no significant difference with rabeprazole 20 mg compared with omeprazole 20 mg at 4 weeks (RR 1.00; 95% CI: 0.87, 1.14; P ¼ 0.95) or at 8 weeks (RR 0.98; 95% CI: 0.91, 1.05; P ¼ 0.55) 23. A few systematic reviews about PPIs have been published, being the last one available in 2006 24. This research only analyzed six articles; therefore this review includes more information. A potential limitation of this research is that it doesn´t analyze 33 articles that have been selected because they were not found published in full. However, this review demonstrates the same results that last ones. This fact and the results obtained lead us to consider that these articles will not change the results obtained. Esomeprazole seems to be the most efficient Proton Pump Inhibitor to induce and maintain mucosal healing. Another restriction of this review is that it doesn’t analyse esomeprazole 40mg at 24 weeks of treatment and either 20 mg at 8 weeks, due to the inexistence and reduced number of articles describing it, respectively. This systematic review should be viewed as promising evidence of Esomeprazole superiority, and suggests that it is perhaps reasonable to use this PPI in routine care because of its efficiency in healing and maintenance of mucosal injury. CONCLUSION Esomeprazole appears to be the most efficient Proton Pump Inhibitor to induce and maintenance of mucosal healing. Once GERD is a chronic and prevalent disease that induces so many long-term complications this result will be of extreme importance because it will allow to provide symptom relief, improved quality of life and protection from long-term complications for GERD patients. REFERENCES 1 Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R (2006). Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidencebased consensus. Am J Gastroenterol. 101(8):1900-20. 2 Wiklund I (2004). Review of the quality of life and burden of illness in gastroesophageal reflux disease. Dig Dis. 22: 108–14. 3 Wiklund I, Carlsson J, Vakil N (2006). Gastroesophageal reflux symptoms and well-being in a random sample of the general population of a Swedish community. Am J Gastroenterol. 101: 18–28. 4 Vakil N (2006). The frontiers of reflux disease. Dig Dis Sci. 51(11):1887-95. 5 Pettit M (2005). Treatment of gastroesophageal reflux disease. Pharm World Sci. 27(6):432-5. 6 Ramakrishnan A, Katz PO (2003). Overview of medical therapy for gastroesophageal disease. Gastrointest Endosc Clin N Am. 13: 57–68. 7 Go MF (2006). Drug Injury in the Upper Gastrointestinal Tract: Nonsteroidal AntiInflammatory Drugs. Gastrointest Endosc Clin N Am. 16(1):83-97. 8 Gibbons TE, Gold BD (2003). The use of proton pump inhibitors in children: a comprehensive review. Paediatr Drugs. 5(1):25-40. 9 Coron E, Hatlebakk JG, Galmiche JP (2007). Medical therapy of gastroesophageal reflux disease. Curr Opin Gastroenterol. 23(4):434-9. 10 Glatzel D, Abdel-Qader M, Gatz G, Pfaffenberger B (2006). Pantoprazole 40 mg is as effective as esomeprazole 40 mg to relieve symptoms of gastroesophageal reflux disease after 4 weeks of treatment and superior regarding the prevention of symptomatic relapse. Digestion. 74(34):145-54. 11 Kahrilas PJ, Falk GW, Johnson DA, Schmitt C, Collins DW, Whipple J, D'Amico D, Hamelin B, Joelsson B (2000). Esomeprazole improves healing and symptom resolution as compared with omeprazole in reflux oesophagitis patients: a randomized controlled trial. The Esomeprazole Study Investigators. Aliment Pharmacol Ther. 14(10):1249-58. 12 K, Devière J, Bigard MA, Bayerdörffer E, Mózsik G, Murray F, Kristjánsdóttir S, Savarino V, Vetvik K, De Freitas D, Orive V, Rodrigo L, Fried M, Morris J, Schneider H, Eklund S, Larkö A; Metropole study results. Esomeprazole 20 mg and lansoprazole 15 mg in maintaining healed reflux oesophagitis: Metropole study results. Aliment Pharmacol Ther. 17(3):333-41. 13 Tsai HH, Chapman R, Shepherd A, McKeith D, Anderson M, Vearer D, Duggan S, Rosen JP (2004).Esomeprazole 20 mg on-demand is more acceptable to patients than continuous lansoprazole 15 mg in the long-term maintenance of endoscopy-negative gastro-oesophageal reflux patients: the COMMAND Study. Aliment Pharmacol Ther. 15;20(6):657-65. 14 Fock KM, Teo EK, Ang TL, Chua TS, Ng TM, Tan YL (2005).Rabeprazole vs esomeprazole in non-erosive gastro-esophageal reflux disease: a randomized, double-blind study in urban Asia. World J Gastroenterol. 28;11(20):3091-8. 15 Scholten T, Gatz G, Hole U (2003). Once-daily pantoprazole 40 mg and esomeprazole 40 mg have equivalent overall efficacy in relieving GERD-related symptoms. Aliment Pharmacol Ther. 15;18(6):587-94. 16 Goh KL, Benamouzig R, Sander P, Schwan T (2007). Efficacy of pantoprazole 20 mg daily compared with esomeprazole 20 mg daily in the maintenance of healed gastroesophageal reflux disease: a randomized, double-blind comparative trial - the EMANCIPATE study. Eur J Gastroenterol Hepatol. 19(3):205-11. 17 Chen CY, Lu CL, Luo JC, Chang FY, Lee SD, Lai YL (2005).Esomeprazole tablet vs omeprazole capsule in treating erosive esophagitis. World J Gastroenterol. 28;11(20):3112-7. 18 Richter JE, Kahrilas PJ, Sontag SJ, Kovacs TO, Huang B, Pencyla JL (2001) .Comparing lansoprazole and omeprazole in onset of heartburn relief: results of a randomized, controlled trial in erosive esophagitis patients. Am J Gastroenterol. 96(11):3089-98. 19 Schmitt C, Lightdale CJ, Hwang C, Hamelin B (2006). A multicenter, randomized, double-blind, 8-week comparative trial of standard doses of esomeprazole (40 mg) and omeprazole (20 mg) for the treatment of erosive esophagitis. Dig Dis Sci. 51(5):844-50. 20 Fennerty MB, Johanson JF, Hwang C, Sostek M (2005). Efficacy of esomeprazole 40 mg vs. lansoprazole 30 mg for healing moderate to severe erosive oesophagitis. Aliment Pharmacol Ther. 21(4):455-63. 21 Castell DO, Kahrilas PJ, Richter JE, Vakil NB, Johnson DA, Zuckerman S, Skammer W, Levine JG (2002). Esomeprazole (40 mg) compared with lansoprazole (30 mg) in the treatment of erosive esophagitis. Am J Gastroenterol. 97(3):575-83. 22 Labenz J, Armstrong D, Lauritsen K, Katelaris P, Schmidt S, Schütze K, Wallner G, Juergens H, Preiksaitis H, Keeling N, Nauclér E, Eklund S; Expo Study Investigators (2005). A randomized comparative study of esomeprazole 40 mg versus pantoprazole 40 mg for healing erosive oesophagitis: the EXPO study. Aliment Pharmacol Ther. 21(6):739-46. 23 Edwards SJ, Lind T, Lundell L (2001). Systematic review of proton pump inhibitors for the acute treatment of reflux oesophagitis. Aliment Pharmacol Ther. 15: 1729–36. 24 SJ, Lind T, Lundell L. (2006). Systematic review: proton pump inhibitors (PPIs) for the healing of reflux oesophagitis - a comparison of esomeprazole with other PPIs. Aliment Pharmacol Ther. 1;24(5):743-50.