Agents to Treat Gastric Acidity and Gastroesophageal Reflux (GERD)
advertisement
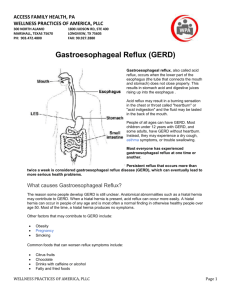
Agents to Treat Gastric Acidity and Gastroesophageal Reflux Disease (GERD) Presented by Abby Roth Overview • Introduction – Symptoms • Causes – Peptic Ulcer Disease • H. pylori • NSAIDs – GERD • Treatments Who is Affected? Gastric acidity and GERD affects people of all ages, races, and gender Symptoms • Heartburn • Regurgitation • Acid Indigestion • Nausea Symptoms Continued • Hoarseness • Sore Throat • Chest Pain • Bad Breath • Dry Cough • Asthma* Symptoms in Children • Vomiting • Coughing • Breathing Problems Acid-Peptic Disorders • Peptic Ulcer Disease –Occurs when there is an imbalance between the mucosal defense factors and the acid and pepsin. Helicobacter pylori Infection • Causes 80% of peptic ulcers • Survives the acid environment by attaching to the sugar molecules that line the stomach wall • Uses the mucus layer as protection H. pylori • Produce large amounts of urease Urease H20 Urea 3 NH3 + CO2 H. pylori • Secret proteins and toxins that interact with the stomach’s epithelial cells • Leads to inflammation and damage NSAIDs • Aspirin, Ibuprofen, Naproxen • Can have an affect at very low doses • Suppresses cylooxygenase-1 • Decrease production of prostaglandins What is GERD? • Condition where the stomach acid/content is pushed back or “refluxed” into the esophagus • Affects 10 million Americans • Approximately 7% have daily symptoms • Link GERD vs. NERD • Patients suffering symptoms are placed in two groups –Non-erosive reflux disease, or NERD –Erosive esophagitis • Erosive esophagitis is characterized by swelling and Inflammation –Barrett’s Esophagus –Precursor to Esophageal Cancer Causes of GERD • Abnormalities with the Lower Esophageal Sphincter, or LES • Stomach Abnormalities –Hiatal hernia –Link Causes • Medications –NSAIDs –Calcium Channel Blockers (high blood pressure, angina) Medications –Anticholinergics (urinary tract disorders) –Beta Adrenergic Agonists (asthma) –Dopamine (Parkinson’s disease) Causes • Food and Drinks – Carbonated beverages – Chocolate – Alcohol – Citrus Fruits – Coffee or Tea – Fatty foods – Containing tomatoes – Mint – Spicy Food Causes • Smoking – Damages mucus membranes – Impairs muscle reflexes in the throat – Increases acid secretion – Reduces LES function and salivation Causes • Obesity • Laying down after a large meal • Eating close to bed time • Exercise Release of Gastric Acid Release of Gastric acid • Histamine stimulates acid release by interacting with the histamine receptor, H2 • Acetylcholine activates the cholinergic receptors • Gastrin is released when food is present in the stomach Treatments • • • • • • • Antacids Alginates Sucralfate Proton Pump Inhibitors Histamine H2-Recptor Antagonists Prokinetics New Treatments Antacids • Quick but short term • Buffer gastric acid, increasing the pH • Neutralize acid by the following reaction Al(OH)3 + 3 HCl AlCl3 + 3 H2O Antacids –Maalox • Al(OH)3 (aluminum hydroxide), Mg(OH)2 (magnesium hydroxide) Antacids • Tums • CaCO3 (calcium carbonate) Antacids –Pepto-Bismol • C7H5BiO4 (bismuth subsalicylate) Antacids –Alka-Seltzer • NaHCO3 (sodium bicarbonate) Alginates • Alginates –Usually combined with an antacid –Forms protective barrier on top of gastric contents –Gaviscon • Sodium Alginate, Sodium Bicarbonate, and Calcium Carbonate –Link Alginates • Polysaccharide found in the cell walls of brown algae • Sodium alginate is the sodium salt of alginic acid Alginic Acid Sucralfate • Reacts with stomach acid to from a cross linked viscous polymer that acts as an acid buffer • Can bind to proteins on the surface of an ulcer to prevent further acid damage • Has been shown to aid in healing by promoting epidermal growth factors and prostaglandins Sucralfate (Carafate) Proton Pump Inhibitors • Proton pump inhibitors (PPIs) – Inhibits the gastric acid pump, H+/K+ ATPase – Are prodrugs PPIs • Diffuse into the parietal cells of the stomach and accumulates • Activated by proton-catalyzed formation of sulfenic acid • This prevents the drug from diffusing out • Activated form then irreversibly binds at the sulfhydryl groups of the cysteins of the H+/K+ ATPase • Link Cysteine PPIs Rabeprazol (Acipex) PPIs Lansoprazole (Prevacid) PPIs Esomeprazole (Nexium) PPIs Omeprazole (Prilosec) Omeprazole/sodium bicarbonate (Zegerid) PPIs Pantoprazole (Protonix) Treatments • Histamine H2-recptor antagonists (H2RAs) • The hormone, histamine stimulates the release of acid by interacting with the histamine receptor, or H2 receptor. • Inhibit acid secretion by competitively and reversibly blocking parietal cell H2receptors • Less potent then PPI’s Agonist vs. Antagonist • An agonist is a drug that produces the same response at a receptor as the natural messenger • An antagonist is a drug which binds to a receptor without activating it, prevent an agonist or natural messenger from binding Histamine H2RAs Cimetidine (Tagamet) H2RAs Nizatidine (Axid) Other H2RAs Famotidine (Pepcid) Ranitidine HCl (Zantac) Treatments • Prokinetics –Increase LES function –Release stomach contents by •Activating serotonin receptors •Acting on dopaminergic receptors Prokinetics Metoclopramide (Reglan, Degan) Prokinetics Domperidone (Motilium, Costi) Prokinetics Cisapride (Prepulsid, Propulsid) Prokinetics • Rarely used because of severe side effects – Fatigue –Tremors –Parkinsonism –Tardive Dyskinesia –Severe cardiac events New Treatments • Cholecystokinin2 receptor antagonists (CCK2) • Potassium competitive acid blockers (P-CABs) Treatments • Cholecystokinin2 receptor antagonists (CCK2) –Block the CCK2 receptors inhibiting acid secretion –Still in clinical trials –Best use in combination with PPI’s CCK2 Itriglumide CCK2 Z-360 Treatments • Potassium competitive acid blockers (P-CABs) – Target H+/K+ ATPase – Ionically binds to the proton pump – Specific for the K+ binding region and prevents acid secretion – Binds reversibly – Still in clinical trials P-CABs Revaprazan P-CABs Soraprazan Treatment for H. pylori • Amoxicillin + clarithromycin + proton pump inhibitor • Metronidazole + clarithromycin + proton pump inhibitor • Bismuth subsalicylate + metronidazole + tetracycline + proton pump inhibitor Assigned Reading • Vesper, J.B. et all, Gastroesophageal Reflux Diesease, Is there More to the Story?, ChemMedChem (2008), 3, 552-559. Homework Questions • What is an antagonist and how do the H2RAs (histamine receptor antagonists) act as one? • Explain the precise biological mechanism whereby prokinetics achieve their effect, including the receptors they act upon. Are they agonists or antagonists? Of which chemical messenger? • What is a prodrug? What causes the PPI’s to become an active drug? • Bacteria in the upper GI tract may play a role in GERD. Explain. References • Bak, Young-Tae. Management Strategies for Gastroesophageal Reflux Disease. Journal of Gastroenterology and Hepatology (2004), 19, S49-S53. • Horn, J. Understanding the Pharmacodynamic and Pharmacokinetic Differences between proton pump inhibitors- focus on pKa and metabolism. AP&T (2006), 2, 340-350. • Pettit, M. Treatment of Gastroesophageal Reflux Disease. Pharm World Sci (2005) 27, 432-435. • Vakil, N., New Pharmacological Agents for the Treatment of Gastroesophageal Reflux Disease. AP&T (2006), 19, 1041-1049. • Vesper, J.B. et all, Gastroesophageal Reflux Diesease, Is there More to the Story?, ChemMedChem (2008), 3, 552-559. • Goodman and Gilman pg 967-980. • Patrick pg 643-671.