Venous Gas Embolism
advertisement

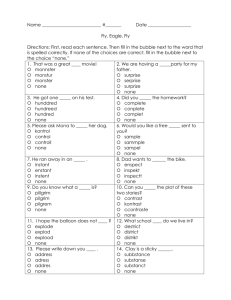
Venous Gas Embolism 4/2/09 FANZCA Notes = ingress of gas into the venous circulation -> embolism into pulmonary circulation -> right heart failure and cardiovascular compromise PATHOPHYSIOLOGY - gas introduced -> travels through right heart -> trapped in pulmonary arteries -> right ventricular HT -> failure - if happens quickly -> failure - if happens gradually -> platelets, fat and neutrophils build up around bubble -> inflammatory reaction -> APO - gas can travel to arterial circulation via PFO and intra-pulmonary shunts (thebesian veins, bronchial vessels) AETIOLOGY Requires 1. source of gas 2. communication between gas and venous system 3. pressure gradient allowing ingress of gas CLINICAL FEATURES - high risk patient: head up with central access, multiple infusion, rapid fluid transfusions under pressure - high risk surgery -> any surgery where the operative field is above the heart and veins are large and held open by connective tissue (gas insufflation procedures, sitting craniotomy, posterior fossa craniotomy, spinal surgery, large bore venous lines, Caesarian section) - lightheadness, dizziness, SOB, chest pain, anxiety, tacypnoea, tachycardia, decreased LOC arrhythmias hypotension apnoea -> hypoxia -> cardiovascular collapse ‘mill wheel’ murmur APO INVESTIGATIONS - sudden increase in ET nitrogen - increased dead space -> sudden fall in ETCO2 - ECG abnormalities; tachyarrhythmias, AV block, right heart strain, T wave changes, ST changes Jeremy Fernando (2011) - increase in CVP increase in PCWP bubbles seen on TOE bubbles heard on praecordial Doppler fall in SpO2 (late sign) CXR; normal -> non-cardiogenic pulmonary oedema PREVENTION - screening for PFO -> transcranial Doppler for IV bubble administration or ECHO - avoid sitting position - reduce the height from operative site to RA - keep CVP full - pressure over jugular veins @ high risk times - PEEP (not in sitting position -> increased likelihood of paradoxical embolism in patients with PFO) - military antishock trousers - meticulous surgical technique - @ insertion or removal of CVL keep RA above site - check lines for bubbles/air DETECTION - capnography praecordial Doppler TOE (most sensitive and specific) ETN2 PA catheter transcranial Doppler praecordial or oesophageal stethoscope CVP clinical signs MANAGEMENT Goals 1. 2. 3. 4. Maintain oxygenation Minimise further air entrainment Reduce size of embolism Overcome mechanical obstruction caused by embolism A – ETT B – FiO2 1.0 C – CPR if required Prevent further Air entrainment - flood field with saline and compress wound edges Jeremy Fernando (2011) - position operative site below RA then supine to for cerebral protection. - load with IVF - increase intrathoracic pressure -> Valsava (decrease VR) Reduce size of embolism - 100% O2 (prevents nitrogenation and therefore expansion of bubble) - aspirated blood with CVL (won’t be effective unless tip in RA) - hyperbaric O2 Overcome mechanical obstruction - if air in RA – left lateral position will hopefully mean bubble travel superiorly allowing RV to empty - inotropes - bypass -> air can be aspirated from PA - admit to ICU/HDU discuss with family and patient document debrief case review and preventative strategies implemented Jeremy Fernando (2011)