Objectives 6 - U
advertisement

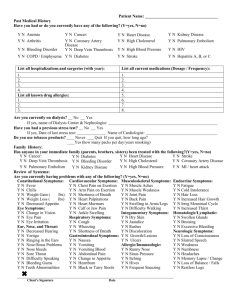
Pathology Lecture 6 Thrombosis, Embolism, and Infarction 1) To understand the principle of thrombus formation and differences between thrombus and post-mortem clot. A thrombus is the formation of a solid mass (tissue-like consistency) of blood within living blood vessels or heart in a noninterrupted cardiovascular system. This involves blood vessel walls, formed elements of blood, and coagulation system. Lines of Zahn, alternating layers of platelet-fibrin columns and red blood cell columns, may also be present. A post-mortem clot involves only the coagulation system, is gelatinous, and made of a plasma mass. 2) To know predisposing factors for thrombosis. 1) Endothelial injury (e.g. atherosclerosis), 2) Altered blood flow (e.g. turbulence, stasis), and 3) Increased coagulability of blood (e.g. trauma, burns, post-partum). 3) To know the outcomes of thrombosis and adverse effects associated with it. Outcomes include: 1) Resolution/dissolution, 2) Embolization, 3) Propagation (enlargement), 4) Organization (with attachment to vessel wall and/or recanalization). Adverse Effects include: 1) decreased vascular flow (partial or total), with ischemia or infarction (ischemic necrosis) of tissue supplied by thrombosed vessel and 2) Embolization to another site. 4) To be familiar with clinical risk factors for thrombosis. 1) Advanced age, 2) Bed rest or other immobilization, 3) Decompensated heart disease, 4) Extensive tissue damage, 5) Malignancy, usually advanced – Migratory thrombophlebitis (Trousseau’s sign), 6) Late pregnancy, post-partum status, and 7) Oral contraceptives. 5) To know the clinical features and possible outcome of venous thrombosis. Venous thrombosis occurs mainly in the large veins of the lower extremities and pelvis. Patients may present with swelling and pain. They may embolize to another area, mainly the lungs. 6) To understand the general and specific mechanisms of embolism. Embolism is the passage and eventual trapping within the vasculature of any of a wide variety of mass objects, the most common of which are fragments of thrombi. 7) To know the settings for, and the potential outcomes of, pulmonary embolism. Pulmonary embolism usually occurs in immobilized postoperative patients and in those with CHF. A venous thrombosis forms in the lower extremities and a fragment breaks away traveling through the heart to the pulmonary arteries. Possible outcomes include: 1) clinically silent (60-80%) – resolution common, 2) sudden death (5%) – “saddle embolism,” 3) Pulmonary infarction (10-15%) or hemorrhage (10-15%) – usually in patients with compromised cardiovascular function, and 4) pulmonary hypertension (2-3%) – usually multiple episodes of small thromboemboli. 8) To be aware of the origin and outcome of arterial emboli. Arterial emboli usually arise from thrombi in the heart (80-85%) or from thrombi overlying atherosclerotic arterial lesions. These usually cause infarction of tissue distal to the site of lodgment (lower extremities, kidney, spleen, etc.). 9) To be familiar with forms of embolism other than thromboembolism. Other types of emboli include: Amniotic fluid embolism (at time of delivery), air (or gas) embolism (decompression sickness), and fat embolism (trauma). Miscellaneous sources of emboli include fragments of atherosclerotic plaques, clumps of inflamed infected tissue and tumor fragments. 10) To know the nature of infarction. Infarction is a localized area of ischemic necrosis secondary to arterial (more commonly) or venous occlusion. 11) To understand the differences between anemic and hemorrhagic infarction, mechanisms of formation of each and examples of sites of each. Anemic infarcts, or white infarcts, involve arterial occlusion in solid tissues forming pale areas of coagulation necrosis (ex. heart, kidneys). Hemorrhagic infarcts, or red infarcts, involve venous occlusion in tissues with dual or overlapping blood supplies and tissues previously congested, or when blood flow returns to an area already necrotic due to arterial occlusion. They usually appear hemorrhagic or purple grossly. Microscopically, they show coagulation necrosis with accompanying hemorrhage (ex. lung, ovary, testis, small bowel. 12) To know the pathologic features (gross and microscopic) of infarction. Grossly, infarcts are usually wedge-shaped (apex towards site of vascular occlusion) and may initially have a darker color than usual but later have a pale (white infarcts) or red to purple (red infarcts) color. Tissue is often more firm than normal. Microscopically, coagulation necrosis is apparent with or without hemorrhage. 13) To be familiar with all information provided in handout on Thrombosis, Embolism, and Infarction. Review handout.