THE ENDOCRINE SYSTEM
advertisement
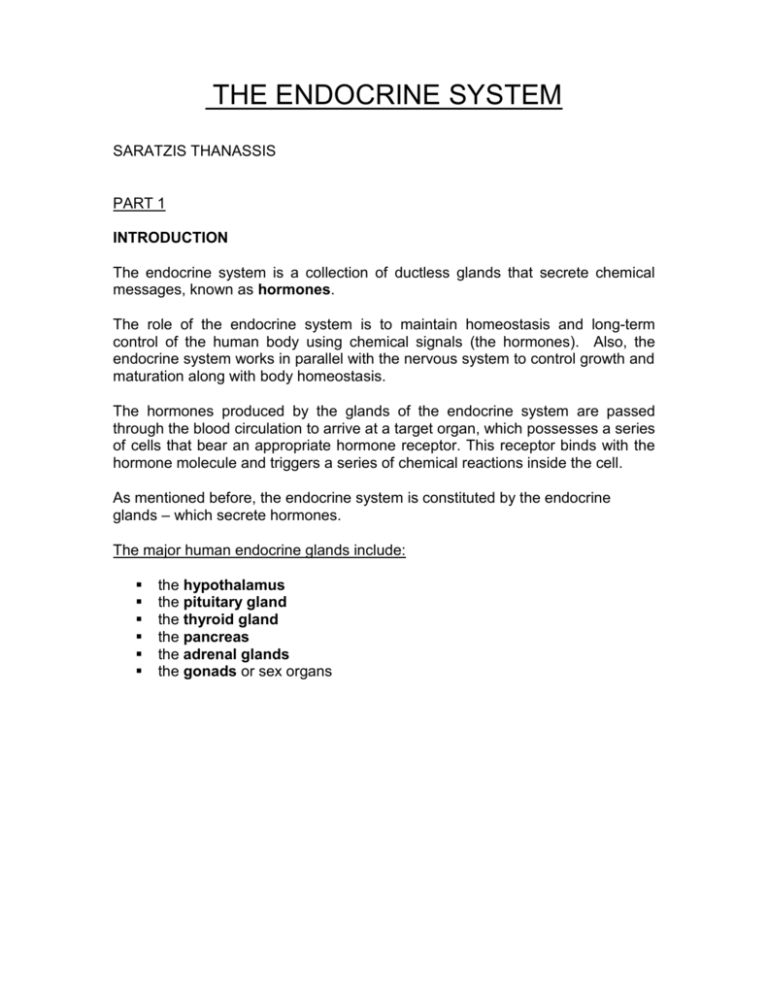
THE ENDOCRINE SYSTEM SARATZIS THANASSIS PART 1 INTRODUCTION The endocrine system is a collection of ductless glands that secrete chemical messages, known as hormones. The role of the endocrine system is to maintain homeostasis and long-term control of the human body using chemical signals (the hormones). Also, the endocrine system works in parallel with the nervous system to control growth and maturation along with body homeostasis. The hormones produced by the glands of the endocrine system are passed through the blood circulation to arrive at a target organ, which possesses a series of cells that bear an appropriate hormone receptor. This receptor binds with the hormone molecule and triggers a series of chemical reactions inside the cell. As mentioned before, the endocrine system is constituted by the endocrine glands – which secrete hormones. The major human endocrine glands include: the hypothalamus the pituitary gland the thyroid gland the pancreas the adrenal glands the gonads or sex organs Gonads The endocrine system in females and males HORMONES A hormone is a messenger molecule synthesized and secreted by a group of specialized cells that constitute an endocrine gland. These glands are ductless, which means that their secretions (hormones) are released directly into the bloodstream and travel elsewhere in the body to target organs, upon which they act. Note that this is in contrast to the exocrine glands, which have ducts for releasing the substances that they produce. Exocrine glands (not part of the endocrine system) secrete products that are passed outside the body. Sweat glands and salivary glands are examples of exocrine glands. There are three general groups of hormones. These are classified as follows – according to their chemical structure: Steroid hormones including prostaglandins which function especially in a variety of female functions and the sex hormones all of which are lipids made from cholesterol. Amino acid derivatives (like epinephrine) which are derived from amino acids, especially tyrosine. Peptide hormones (like insulin) which are the most numerous/diverse group of hormones. Mechanisms of Hormone Action Hormones trigger actions in specific target cells, after binding to an appropriate receptor. Receptors are membrane proteins that bind to hormones. A certain hormone receptor located on a specific target cell can only bind to one type of hormone. More than fifty human hormones have been identified; all act by binding to receptor molecules. The binding hormone causes a change in the shape of the receptor. This alteration of the receptor’s molecule causes the cell to respond to the hormone. There are two different mechanisms of hormone action on all target cells: Steroid and non – steroid hormones Nonsteroid Hormones Nonsteroid hormones (water soluble) do not enter the cell but bind to plasma membrane receptors, generating a chemical signal (second messenger) inside the target cell. Five different second messenger chemicals, including cyclic AMP have been identified. Second messengers activate other intracellular chemicals to produce the target cell response. The action of nonsteroid hormones Images from: http://www.emc.maricopa.edu/faculty/farabee Steroid Hormones The second mechanism involves steroid hormones, which pass through the plasma membrane and act in a two step process. Steroid hormones bind, once inside the cell, to the nuclear membrane receptors, producing an activated hormone-receptor complex. The activated hormone-receptor complex binds to DNA and activates specific genes, increasing production of proteins. The action of nonsteroid hormones Images from: http://www.emc.maricopa.edu/faculty/farabee Maintenance of the hormones homeostasis in the blood When hormone levels reach a certain normal or necessary amount, further secretion is controlled by important body mechanisms to maintain that level of hormone in the blood. This regulation of hormone secretion may involve the hormone itself or another substance in the blood related to the hormone. For example, if the thyroid gland has secreted adequate amounts of thyroid hormones (such as thyroxin) into the blood, the pituitary gland senses the normal levels of thyroid hormone in the bloodstream and gears down its release of thyrotropin, the pituitary hormone that stimulates the thyroid gland to produce thyroid hormones. Parathyroid hormone increases the level of calcium in the blood. When the blood calcium level rises, the parathyroid glands sense the change and decrease their secretion of parathyroid hormone. This turn-off process is called "negative feedback" system. Negative feedback in the thyroxin release reflex Image from: http://www.emc.maricopa.edu/faculty/farabee GLANDS OF THE ENDOCRINE SYSTEM 1. HYPOTHALAMUS – PITUITARY GLAND The pituitary gland (often called the master gland) is located in a bony cavity at the base of the brain. A stalk links the pituitary to the hypothalamus, which controls release of pituitary hormones. The pituitary gland has two lobes: the anterior and posterior lobes. The anterior pituitary is glandular. The hypothalamus contains neurons that control the releases from the anterior pituitary, through seven hypothalamic hormones which are released into a portal system connecting the hypothalamus and pituitary. These hormones cause targets in the pituitary to release various hormones. Anterior Pituitary Hormones produced and released: Growth hormone Thyrotropin Adrenocorticotropin Leutinizing hormone LH Follicle stimulating hormone FSH Prolactin Endorphins Posterior Pituitary Hormones released: Oxytocin Vasopressin Anti – diuretic hormone (ADH) GONADOTROPINS Growth hormone (GH) is a peptide anterior pituitary hormone essential for growth. The hypothalamus maintains homeostatic levels of GH, by the release of GH-releasing and GH-inhibiting hormones. GH-releasing hormone stimulates release of GH. GH-inhibiting hormone suppresses the release of GH. Cells under the action of GH increase in size (hypertrophy) and number (hyperplasia). GH also causes increase in bone length and thickness by deposition of cartilage at the ends of bones. During adolescence, sex hormones cause replacement of cartilage by bone, halting further bone growth even though GH is still present. Too little or two much GH can cause dwarfism or gigantism, respectively. Gonadotropins and prolactin are also secreted by the anterior pituitary. Gonadotropins (which include follicle-stimulating hormone, FSH, and luteinizing hormone, LH) affect the gonads by stimulating gamete formation and production of sex hormones. Prolactin is secreted near the end of pregnancy and prepares the breasts for milk production. The posterior pituitary stores and releases hormones into the blood. Antidiuretic hormone (ADH) and oxytocin are produced in the hypothalamus and transported by axons to the posterior pituitary where they are dumped into the blood. ADH controls water balance in the body and blood pressure. Oxytocin is a small peptide hormone that stimulates uterine contractions during childbirth Hypothalamus receptors also monitor blood levels of thyroid hormones. Low blood levels of Thyroid-stimulating hormone (TSH) cause the release of TSHreleasing hormone from the hypothalamus, which in turn causes the release of TSH from the anterior pituitary. TSH travels to the thyroid where it promotes production of thyroid hormones, which in turn regulate metabolic rates and body temperatures. The location of the pituitary gland . and the hypothalamus Images from: http://www.emc.maricopa.edu/faculty/farabee 2. THYROID GLAND Location of the thyroid gland Isthmus Right lobe Left lobe Image from: F. Netter Atlas of Anatomy – Ciba Geigy The thyroid gland is located in the front of the neck, below the larynx. The small, two-inch gland consists of two lobes, one on each side of the windpipe, connected by tissue called the isthmus. The microscopic structure of the thyroid is quite distinctive. Thyroid epithelial cells - the cells responsible for synthesis of thyroid hormones - are arranged in spheres called thyroid follicles. Follicles are filled with colloid, a proteinaceous depot of thyroid hormone precursor. In the low (left) and high-magnification (right) images of thyroid below, follicles are cut in cross section at different levels, appearing as roughly circular forms of varying size. Images from: http://arbl.cvmbs.colostate.edu/hbooks /pathphys/endocrine/thyroid/ In addition to thyroid epithelial cells, the thyroid gland houses one other important endocrine cell. Nestled in spaces between thyroid follicles are parafollicular or C cells, which secrete the hormone calcitonin. Most of the thyroid tissue consists of the follicular cells, which secrete iodinecontaining hormones called thyroxine (T4) and triiodothyronine (T3). The parafollicular cells secrete the hormone calcitonin. Iodine is essential in order for the thyroid to produce the hormones. Thyroid hormones are poorly soluble in water, and more than 99% of the T3 and T4 circulating in blood is bound to carrier proteins. The principle carrier of thyroid hormones is thyroxine-binding globulin, a glycoprotein synthesized in the liver. Two other carriers of import are transthyrein and albumin. Carrier proteins allow maintenance of a stable pool of thyroid hormones from which the active, free hormones are released for uptake by target cells. The thyroid hormones play an important role in regulating the body's metabolism and calcium balance. The T4 and T3 hormones stimulate every tissue in the body to produce proteins and increase the amount of oxygen used by cells. The calcitonin hormone works together with the parathyroid hormone to regulate calcium levels in the body. Levels of hormones secreted by the thyroid are controlled by the pituitary gland's thyroid-stimulating hormone, which in turn is controlled by the hypothalamus. 3. PANCREAS The pancreas serves two principal functions. Firstly, it acts as a ducted gland, secreting digestive enzymes into the small intestine. It also serves as a ductless gland in that the islets of Langerhans secrete insulin and glucagon to regulate the blood glucose level. The islet cells secrete glucagon, which causes the liver to catabolise stored carbohydrates in order to raise a low glucose sugar level. The islet cells also secrete insulin which causes the liver to take excess glucose out of circulation to lower a high blood glucose level. Image from: http://www.howstuffworks.com Insulin is made and secreted by the beta cells of the pancreatic islets. Insulin is required by almost all of the body's cells, but its major targets are liver cells, fat cells and muscle cells. Insulin serves the following actions: Stimulates liver and muscle cells to store glucose in glycogen Stimulates fat cells to form fats from fatty acids and glycerol Stimulates liver and muscle cells to make proteins from amino acids Inhibits the liver and kidney cells from making glucose from intermediate compounds of metabolic pathways (gluconeogenesis) As shown in this diagram, insulin and glucagon have an opposite effect on liver and other tissues for controlling bloodglucose levels. Together, they regulate the amount of glucose that circulates in the blood. Image from: http://www.howstuffworks.com/diabetes1.htm 4. ADRENAL GLANDS The adrenal glands are situated on top of the kidneys. They consist of the outer cortex and the inner medulla. The medulla secretes epinephrine (also known as adrenaline) and other similar hormones in response to stressors Image from: http://www.nlm.nih.gov/medlineplus/ency/htm such as fright, anger, caffeine, or low blood sugar. The cortex secretes several classes of steroid hormones (glucocorticoids and mineralocorticoids). Despite their organization into a single gland, the medulla and cortex are functionally different endocrine organs, and have different embryological origins. Cells in the adrenal medulla synthesize and secrete norepinephrine and epinephrine. Following release into blood, these hormones bind adrenergic receptors on target cells, where they induce essentially the same effects as direct sympathetic nervous stimulation. The adrenal cortex is a factory for steroid hormones. In total, at least two to three dozen different steroids are synthesized and secreted from this tissue, but two classes are of particular importance: Class of Steroid Major Representative Physiologic Effects Mineralocorticoids Aldosterone Na+, K+ and water homeostasis Glucocorticoids Cortisol Glucose homeostasis and many others Additionally, the adrenal cortex produces some sex steroids, particularly androgens. Like all steroids, adrenal "corticosteroids" are synthesized from cholesterol. The adrenal cortex and medulla Image from: http://a248.e.akamai.net 5. GONADS (SEX ORGANS) The gonads include the female ovaries and the male testes. In addition to producing gametes, the female ovaries and male testes also secrete a number of hormones (sex hormones) Testes Male sex hormones, as a group, are called androgens. The principal androgen is testosterone, which is secreted by the testes. A small amount is also produced by the adrenal cortex. Production of testosterone begins during fetal development, continues for a short time after birth, nearly ceases during childhood, and then resumes at puberty. This steroid hormone is responsible for: The growth and development of the male reproductive structures Increased skeletal and muscular growth Enlargement of the larynx accompanied by voice changes Growth and distribution of body hair Increased male sexual drive Testosterone secretion is regulated by a negative feedback system that involves releasing hormones from the hypothalamus and gonadotropins from the anterior pituitary. Ovaries Two groups of female sex hormones are produced in the ovaries, the estrogens and progesterone. These steroid hormones contribute to the development and function of the female reproductive organs and sex characteristics. At the onset of puberty, estrogens promotes: The development of the breasts Distribution of fat evidenced in the hips, legs, and breast Maturation of reproductive organs such as the uterus and vagina Progesterone causes the uterine lining to thicken in preparation for pregnancy. Together, progesterone and estrogens are responsible for the changes that occur in the uterus during the female menstrual cycle. INTERNET LINKS GENERAL http://www.martindalecenter.com/Medical1_1_EaGa.html#Endo - general information on endocrinology http://training.seer.cancer.gov/module_anatomy/unit6_3_endo_glnds5_go nads.html - a tour of the endocrine system http://www.innerbody.com/image/endoov.html http://www.emc.maricopa.edu/faculty/farabee/BIOBK/BioBookENDOCR.ht ml THYROID GLAND http://arbl.cvmbs.colostate.edu/hbooks/pathphys/endocrine/thyroid/ general information and graphics concerning the thyroid gland http://users.rcn.com/jkimball.ma.ultranet/BiologyPages/T/Thyroid.html thyroid hormones and diseases of the thyroid http://www.endocrineweb.com/thyroid.html - thyroid gland diseases http://www.bartleby.com/107/272.html - anatomy of the thyroid http://www.endocrineweb.com/tests.html - common tests to examine thyroid gland function PANCREAS http://www.howstuffworks.com/diabetes1.htm - general information concerning the pancreas and its main functions http://w3.uniroma1.it/step/chir/h.html - anatomical views of the pancreas http://members.aol.com/OhLarry922/home.html - information on pancreas transplant http://www.endocrineweb.com/pancreas.html - pancreas hormones ADRENAL GLANDS http://arbl.cvmbs.colostate.edu/hbooks/pathphys/endocrine/adrenal/ general information and illustrations on the adrenal glands GONADS http://training.seer.cancer.gov/module_anatomy/unit6_3_endo_glnds5_go nads.html - sex hormones DISEASES ASSOCIATED WITH THE ENDOCRINE SYSTEM BELLI MARIA The Endocrine system is very important for living, because its chemical messengers, hormones, influence the operations of all of the body´ s tissues and organ systems, controlling the body functions. Hormone levels vary and can be influenced by environmental or genetic factors. When the endocrine system doesn’t function properly hormone production is disturbed and a variety of disorders can arise. Controlling the production of or replacing specific hormones can treat many hormonal disorders in children and adolescents, some of which include: 1. Diabetes mellitus (Type 1) Two main forms of diabetes mellitus are recognized: Type 1 (or insulin-depended) and type 2 (or non-insulin depended). Type 1 diabetes mellitus appears at juvenile, when the pancreas fails to produce enough insulin and is the result of an autoimmune process. The disease has a high incidence (15.6 cases per 100000 of the under 21 year old population in the UK annually). Symptoms include hunger, polydipsia, polyuria and loss of weight. It can cause multiple long-term complications including kidney problems, pain from nerve damage, blindness and early coronary heart disease and stroke. Although diabetes mellitus has been recognized for thousands of years, little help could be offered until the discovery of insulin in 1921, because regular insulin injections help the patients to control their blood sugar levels and reduce the risk of developing diabetes complications. It is appreciated that diabetes mellitus is actually a group of disorders that are heterogeneous, probably comprising several entities with separate precipitating factors which result in the typical but not universal, picture of insulitis and beta cell destruction. Major developments in understanding the immunogenetics at a molecular level reveal a very complex interaction of loci both within the MHC (major histocompatibility complex) and outside it. There are genes that play a major role in determining susceptibility or conferring protection. However, there is a hierarchy, depending on haplotype, for these effects, which may relate to other loci that are in linkage disequilibrium, like those regulating TNF (tumor necrosis factor). Much less is known of the influence of non-MHC genes, although by analogy with experimental diabetes, these may be critical to the emergence of disease. This is underlined by relatively low concordance in HLA (human leucocyte antigen)-identical siblings, compared to monozygotic twins, but in turn, the occurrence of diabetes in only 40% of subjects with an affected identical twin indicates the importance of environmental factors. Viruses have some role, most clearly shown in the congenital rubella syndrome; much further work is required to identify how other viral infections may contribute to the initiation of disease. T cell cloning is beginning to elucidate the nature of beta cell-specific T cell autoimmune responses. Several beta cell auto antigens have been identified, although none has been fully characterized and, apart from insulin, these are not completely beta cell-specific. Auto antibodies to the 64 kd antigen seem the most promising marker for diabetes: their pathogenic importance is uncertain. The beta cell may contribute to its own destruction by hyper expression of MHC class 1 and 2 molecules and by synthesis of ICAM-1 (intercellular adhension molecule) and IL-6 (interleukin), all in response to cytokines. Autoantigen presentation by class 2-expressing beta cells has not been demonstrated and this hypothetical function is not supported by experiments with transgenic mice. Cytokines like IL-1 and TNF may be important in beta cell destruction, intra-islet specificity possibly being achieved because beta cells are already damaged or are particularly susceptible to this type of injury. Immunosuppressive treatment has on the whole been disappointing. The most promising agent, cyclosporin A, produces a modest increase in insulin-free remissions but these are only temporary and there are major side effects of prolonged therapy. One possible strategy to improve outcome would be commencement of immuno-modulatory treatment before presentation, when around 90% of the beta cells are already destroyed. This depends on the availability of reliable prediabetic markers and recent progress suggests that such screening may soon be feasible. 2. Hypothyroidism Primary hypothyroidism, the most common form, is probably an autoimmune disease, usually occurring as a result of Hashimoto's thyroiditis and is associated often with a firm goiter or, later in the disease process, with a shrunken fibrotic thyroid gland with little or no function. Iodine deficiency and rare inherited enzymatic defects can also cause hypothyroidism. Patients with hypothyroidism have a dull facial expression and their voice is hoarse and speech is slow. Other symptoms are facial puffiness and periorbital swelling. In addition to that cold intolerance may be prominent; eyelids droop; hair and the skin is coarse and dry. Weight gain is modest and is largely the result of decreased metabolism of food and fluid retention. Patients are forgetful and show other evidence of intellectual impairment, with a gradual change in personality. Some appear depressed. There may be frank psychosis (myxedema madness). A decrease in both thyroid hormone and adrenergic stimulation causes bradycardia. The heart may be enlarged, partly because of dilation but chiefly because of the accumulation of a serous effusion of high protein content in the pericardial sac. Pleural or abdominal effusions may be noted. The pericardial and pleural effusions develop slowly, and only rarely result in respiratory or hemodynamic distress. Patients generally note constipation. Women with hypothyroidism often develop menorrhagia, in contrast to the hypomenorrhea of hyperthyroidism. Hypothermia is commonly noted. Mild anemia is often present, usually normocytic-normochromic and of unknown etiology, but it may be hypochromic owing to menorrhagia, and sometimes macrocytic because of associated pernicious anemia or decreased absorption of folic acid. Myxedema coma is a life-threatening complication of hypothyroidism. Its characteristics include a background of long-standing hypothyroidism, coma with extreme hypothermia (temperatures 24 to 32.2° C [75.2 to 90° F]), areflexia, seizures, CO2 retention, and respiratory depression. Hypothroidism can be treated by oral thyroid hormone replacement. A variety of thyroid hormone preparations are available for replacement therapy, including synthetic preparations of T4 (L-thyroxine), triiodothyronine (liothyronine), combinations of the two synthetic hormones, and desiccated animal thyroid. Synthetic preparations of T4 (L-thyroxine) are preferred. T3 is generated from the T4 in peripheral tissues. T3 (liothyronine sodium) should not be used alone for long-term replacement because its rapid turnover requires that it be taken bid. Additionally, patients receiving T3 are chemically hyperthyroid for at least several hours a day and thus may be exposed to greater cardiac risks. Myxedema coma is treated with a large initial dose of T4 or T3. Corticosteroids are also given since the possibility of central hypothyroidism cannot be initially ruled out. The patient should not be re-warmed rapidly because of the threat of cardiac arrhythmias. Hypoxemia is common, so Pao2 should be measured at the outset of treatment. If alveolar ventilation is compromised, immediate mechanical ventilatory assistance is required. The precipitating illness should be rapidly and appropriately treated and fluid replacement given carefully, since hypothyroid patients do not excrete water appropriately. Finally, all drugs should be given cautiously since they will be metabolized more slowly than in normal people. 3. Acromegaly Acromegaly is a condition resulting from excess growth hormone production and it results in excessive growth. Symptoms of acromegaly vary depending on how long the patient has had the disease. The most common symptoms are: swelling of the hands and feet facial features become coarse as bones grow body hair becomes coarse as the skin thickens and/or darkens increased perspiration accompanied with body odor protruding jaw voice deepening enlarged lip, nose, and tongue thickened ribs (creating a barrel chest) joint pain degenerative arthritis enlarged heart enlargement of other organs strange sensations and weakness in arms and legs snoring fatigue and weakness headaches loss of vision irregular menstrual cycles in women breast milk production in women impotence in men Treatment of acromegaly depends on the cause of the disease. Ninety percent of acromegaly cases are caused by benign tumors on the pituitary gland. Because the tumor is compressing the pituitary gland, the hormone production can be altered. Some other acromegaly cases are caused by tumors of the pancreas, lungs, or adrenal glands. The goal of treatment is to restore the pituitary gland to normal function, producing normal levels of growth hormone. Treatment may include removal of the tumor, radiation therapy, and injection of a growth hormone blocking drug. Left untreated, acromegaly can lead to diabetes mellitus and hypertension. The disease also increases a patient's risk for cardiovascular disease and colon polyps that may lead to cancer. How can a healthy endocrine system be maintained? The glands in the endocrine system and the hormones they secrete influence practically every cell, organ and function of our bodies. The body´ s equilibrium, the reproductive system, the immune system, the emotional well-being, blood pressure, cholesterol, tissue function, sexual function, stress, metabolism, growth and development, all these are influenced by healthy endocrine glands. So, it is very important to maintain a healthy endocrine system. However, poor nutrition and stress puts a burden on the glands, often leading to a depleted state. For example, our adrenals release adrenalin which is produced during stress. When our adrenals become exhausted by repeated stress, it leads to reactive hypoglycemia. Our pancreas, in charge of sugar metabolism, can then also become exhausted which lead to diabetes. Like all organs, our glands need good nutrition. Vital nutrients include vitamins, minerals, and amino acids such as C, E, B-complex, zinc, chromium, selenium, alanine, glycine, and glutamic acid. These nutrients are necessary for proper glandular function and as building blocks by which the glands construct their corresponding hormones. Healthy endocrine glands help ensure our bodies get adequate amounts of necessary hormones such as adrenalin, insulin, testosterone, and estrogen. Without these important glands we cannot handle stress or sugars properly, nor can we reproduce healthy children. To sum up, a wellness plan for support of endocrine and glandular system includes: Regular exercise Healthy diet emphasizing fruits and vegetables Stress management Avoid prolonged exposure to pesticides and other man-made chemicals Pharmacists’ Supplement Recommandations: Vitamins and Minerals - betacarotene, vitamins A, C, D, E, B-complex, pantothenic acid, biotin, folic acid, zinc, selenium, chromium, manganese, copper, iodine, magnesium, calcium, potassium Herbs and Phytonutrients - licorice root, kelp, alfalfa, Siberian Ginseng, Irish moss, parsley, hops, capsicum, lycopene, bioflavonoids Essential Fatty Acids - omega-3 and omega-6 Antioxidants - grape seed extract, Vitamin E Amino Acids - glutamic acid, alanine, glycine, dimethylglycine (DMG) Glandular Extracts - especially adrenal, pituitary, thymus, pancreas. INTERNET LINKS Http://kidshealth.org/parent/general/body-nasics/endocrine.html http://www.merck.com/mrkshared/mmanual/section2/chapter3d http://www.umm.edu/endocrin/acromegaly.htm http://www.rxwellmescenter.com/Endocrine20%and20%glandular.asp-4ok http://www.longevityplus.net http://www.meditationcenter.com/lecture/storms.html BIBLIOGRAPHY (for parts 1 –2) Williams Textbook of Endocrinology – Wilson, Foster, Kronenberg, Larsen Saunders Principles and Practice of Endocrinology and Metabolism – Becker - Lippincott Testosterone – E.Nieschlag, H.M.Behre - Springer Endocrine Secrets – M. T. McDermott – Mosby Fundamentals of Clinical Endocrinology – R. Hall, M. Besser – Churchill Livingstone Diseases of the Thyroid – M.H. Wheeler, J.H. Lazzarus – Chapman and Hall Medical WORDS USED WITHIN THE ESSAY List of Medical words: ΤERM Example in Word class context information Primary hypothyroidism, the most common form, autoimmune is probably an adjective autoimmune disease… coma hormone injection insulin … Longstanding hypothyroidism, coma with extreme hypothermia… The glands in the endocrine system and the hormones they secrete influence practically every cell, organ and function of our bodies. regular insulin injections help the patients to control their blood sugar levels … The pancreas fails to produce enough insulin… noun noun noun noun Dictionary definition A condition that results from sensitization to products of one’s own organs Insensibility, stupor, sleep A substance produced in one organ, which excites functional activity at a distant site Introduction of material under pressure into tissues A poly-peptide hormone, secreted by the β-cells of the Langerhans in the pancreas Greek translation αυτοάνοσος κώμα ορμόνη ένεση, ενιεμένη ουσία ινσουλίνη metabolism polydipsia polyuria stroke symptoms body´ s equilibrium,…, metabolism, growth, are influenced by healthy endocrine glands Symptoms include hunger, polydipsia, polyuria Symptoms include hunger, polydipsia, polyuria It can cause multiple longterm complications including… and stroke Symptoms of acromegaly vary depending on…. noun Chemical process taking place in living cells which may be divided into constructive or building-up process (anabolism) and destructive or breaking-down process (catabolism) μεταβολισμός noun Abnormal thirst πολυδιψία noun Excessive production of urine Πολυουρία noun Cerebrovascular accident noun A noticeable change in the body and its functions, evidence of disease Αιφνίδια προσβολή, χτύπημα σύμπτωμα List of Academic words: TERM complication congenital Example in context It can cause multiple long-term complications including kidney problems… Viruses have some role, most clearly shown in the congenital rubella syndrome; Word class Dictionary Greek information definition translation noun disorder arising επιπλοκή from the circumstances produced by a disease adjective Existing at birth Συγγενής, εκ γενετής hormones,…, controlling the body functions heterogeneous …diabetes mellitus is actually a group of disorders that are heterogeneous,… treatment The goal of treatment is to restore the pituitary gland to normal function function noun adjective noun The normal special work of an organ Differing in kind or in nature λειτουργία ετερογενής A way of curing Αγωγή, a disease θεραπεία