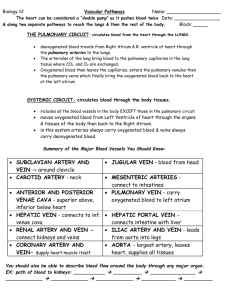
cardiovascular function
advertisement

LAB VIII Cardiovascular & Pulmonary Health & Review of Blood Pressure Regulation Cardiovascular and pulmonary diseases including coronary heart disease, hypertension, cerebrovascular disease, COPD, Asthma, and others make up some of the most common causes of death and disability in the United States and in much of the industrialized world. According to the Centers for Disease Control (a great deal of health statistics can be found for free at www.cdc.gov and www.americanheart.org ), in 2006 the leading causes of death in the U.S. included: 1) Heart Disease (26% of all deaths), 2) Cancer (23.1%), 3) Cerebrovascular Disease (Strokes, 5.7%), and 4) Chronic Lower Respiratory Diseases (including bronchitis, emphysema, asthma, and others, 5.1%). Additionally, diabetes mellitus was number 6 on that list and hypertension was number 13. While the mortality rate for some of the above conditions (e.g. heart disease) are declining due to better prevention and treatment, the incidence of these diseases are staggering and are (mostly) increasing. That is, the decrease in mortality rate does not reflect a healthier population, but rather an improved health care response to these conditions. 33.6% of U.S. adults have hypertension – that is 74,500,000 Americans with hypertension (nearly 30% of all U.S. adults!). For adults who reach the age of 50, the lifetime residual risk of developing hypertension is 90%. In 2000 10 million American adults had a diagnosis of chronic obstructive pulmonary disease (COPD) with an estimate of an additional 14 million undiagnosed cases. Over 16 million U.S. adults and over 7 million U.S. children have asthma. In 2006, heart disease was the number one cause of death in men and women resulting in over 630,000 deaths. Coronary heart disease accounted for a majority of these deaths. Every year nearly 800,000 Americans experience a first heart attack. Nearly 500,000 have already had one or more. In 2010 it is estimated that heart disease will result in more than $316 billion in lost productivity, medications, and health care services. Cardiovascular and pulmonary diseases share some risk factors; especially smoking and tobacco use. Estimates suggest that around 443,000 Americans die prematurely per year as a result of smoking and an additional nearly 9 million illnesses/year. Second hand smoke is also a killer, accounting for an estimated 3,000 deaths/year from lung cancer, 46,000 deaths/year from heart disease, and several hundred thousand respiratory complications in children. This is a major preventable cause of death and disease. In 2005-2006, 39.5% of U.S. adults were considered inactive and only 30% are meeting current physical activity guidelines. Nearly 60% of U.S. adults report no vigorous physical activity in the previous year. Inactivity is one of the major coronary heart disease risk factors. 12.2% of heart attacks are attributed to physical inactivity, even after accounting for other CAD risk factors. Furthermore, physical activity is known to improve several other risk factors including weight control (34% of U.S. adults are obese), hypertension (over 30% of U.S. adults), high cholesterol (almost 16% of U.S. adults), and diabetes (over 10% of U.S. adults). However, exercise does present a health risk for some. The incidence of sudden death is greater in adults than children due to the lower incidence of cardiovascular disease in younger individuals. However, it is recommended that all high school and college athletes undergo routine pre-participation screening prior to competition. A majority of sudden deaths during exercise are caused by heart diseases and conditions. It is of great importance for all individuals who work in health care settings and with athletes to understand some of the risks, signs and symptoms that may put one at risk during exercise. Lab VIII - 1 Lung Volumes and Capacities By this time we have already discussed several important concepts related to the respiratory system including: ventilation (VE), alveolar ventilation (VA), tidal volume (TV), respiratory rate (RR), dead space (DS), and the respiratory control centers in the medulla and pons. Furthermore each of these, and the lung volumes and capacities below are review from your human physiology courses. Additionally students are reminded that we have already discussed the fact that lung volumes and capacities are always reported in BTPS conditions (see lab I, II). Tidal volume averages about 500 ml in adults. If we inspire as much air as we can, the lung is expanded much more than it is in normal respiration. The extra volume taken in above tidal volume following a maximal inspiration is called the inspiratory reserve volume. The sum of the tidal volume and the inspiratory reserve volume is called the inspiratory capacity. The volume of air that can be expired beyond the resting expiratory level is known as the expiratory reserve volume. The air expired from maximal inspiration to maximal expiration is a called the vital capacity. The vital capacity is the greatest volume of air that can be exhaled from the lungs after a maximum inspiration. At the end of a maximal expiration, some air still remains in the lungs. This volume remains because the mechanical limits of expiration have been reached and no further reduction in the thoracic cavity can occur. This remaining volume is called the residual volume. The sum of the residual volume and the expiratory reserve volume is called the functional residual capacity. When the vital capacity and the residual volume are added together, one obtains the total lung capacity (see Fig.1). All the pulmonary volumes and capacities are about 20-25% lower in women than in men, and tend to be greater in elite athletes and in large persons than in small or inactive individuals. Inspiratory Capacity Inspiratory Reserve Volume Total Lung Capacity Tidal Volume Vital Capacity Expiratory Reserve Volume Functional Residual Capacity Residual Volume FIGURE 1 Pulmonary ventilation, or the movement of air in and out of the lungs and air passages is based on changes in thoracic pressure created by respiratory movements. Air movement is therefore dependent on muscle contraction, primarily the diaphragm. However, air movement is limited by airway resistance and lung compliance. Spirometry is a simple method for measuring pulmonary ventilation and determining volume (restrictive) and flow (obstructive) limitations. It allows us to measure all lung volumes except residual volume and to determine the maximal flow rate at which these volumes may be moved in and out of the lungs. You have already learned all of the major lung volumes and Lab VIII - 2 capacities in your human physiology course, please review them before coming to class. Review appendix pages 33 to 45 as your read this lab and complete your experiments. Spirometry and Pulmonary Function testing Restrictive pulmonary diseases are characterized by a reduced ability of the lungs or chest wall to expand. Thus, individuals with restrictive pulmonary diseases tend to have lower vital capacities compared to individuals with normal, healthy lungs(see appendix). Restrictive pulmonary diseases can be defined clinically by a vital capacity that is <80% of predicted. The predicted vital capacity can easily be estimated based on the subject’s gender, height, and age. There are many types of restrictive pulmonary diseases. The largest category of restrictive pulmonary diseases are interstitial lung diseases; which includes pulmonary fibrosis. These conditions mostly result in a loss of elasticity of the lungs and subsequently, a reduced ability to expand and collapse the lungs. Obese individuals may also have reduced volumes & capacities, indicative of a restrictive pulmonary disease; usually due to an inability to lower the diaphragm as far as normal. Individuals with restrictive pulmonary diseases tend to have a greater amount of anatomical and physiological dead space. Thus, during exercise they must increase minute ventilation even more than healthy individuals. It is also harder for patients with restrictive diseases to inflate their lungs. This means that even at rest their respiratory muscles must perform more work to sufficiently oxygenate the blood and clear carbon dioxide from the body. Thus, when these patients exercise, they must move more air than a normal person due to the dead space, and they also need to work harder to move a given amount of air. Another consideration is that due to the reduced ability to expand the lungs, these individuals tend to increase ventilation more by increasing respiratory rate than by increasing tidal volume. (What affect do you think this has on alveolar ventilation?). As you can imagine these individuals are more susceptible to respiratory muscle fatigue than those who have healthy lungs. Obstructive pulmonary diseases on the other hand are characterized by a greater resistance to movement of air into and/or out of the lungs. Remember that Ohms law states that Flow = Pressure / resistance and that Poicelle's law states that the resistance is inversely proportional to the radius to the fourth power. So, if the airway radius is reduced, the resistance to airflow will be greater. As a result of the greater resistance, assuming the pressure gradient is not changed, then the flow (rate of air movement) will be reduced. This is why obstructive pulmonary diseases are usually assessed during spirometry by looking at flow rates. When talking about the pulmonary system, flow (volume/time) is usually reported in liters/second. On a typical spirogram (see appendix) the slope of the tracing indicates the flow. The liters of air moved is indicated by the displacement along the y-axis, and the time it takes to move that air is indicated by displacement along the x-axis. So y-axis displacement in liters divided by x-axis displacement in seconds = liters/second. Determining the slope of the line at any given time can be a time consuming process. Thus, we usually use the FEV1 as an indirect indicator of flow (it is really a volume, but it is a volume that was moved in a given amount of time, 1 second). A healthy individual can expire 80% or more of their FVC out in one second. That is, the ratio of the FEV1 to the FVC should be greater than 80%. This ratio is appropriately named the FEV1/FVC ratio, and it is typically below 80% in individuals with obstructive pulmonary diseases. Examples of obstructive pulmonary disease include asthma, emphysema, and bronchitis. Chronic bronchitis, asthma, and emphysema are frequently referred to collectively as chronic obstructive pulmonary diseases (COPD) because many of the symptoms and problems associated with these different obstructive lung diseases are very similar. The respiratory muscles of subjects with obstructive pulmonary diseases also have to work harder to adequately ventilate the lungs due to the greater resistance to airflow. During exercise large volumes of air must be moved into and Lab VIII - 3 out of the lungs. Because of the great resistance to airflow in the lungs, these patients are often unable to adequately ventilate the lungs, leading to excessive anaerobic metabolism and causing rapid fatigue. Clinically it is very useful to assess pulmonary function by having the volume (in liters) plotted out on a graph against the flow (in liters/second). The resulting graph is called a flowvolume loop (see appendix). The volume is on the x- axis and the flow is on the y-axis. Air movement during expiration is recorded above the x-axis, and inspiration is recorded below the xaxis. It is an appropriate time to begin thinking about what this curve would look like for an individual with an obstructive or a restrictive pulmonary disease. The coronary circulation in health and disease The coronary arteries are the arteries that provide oxygen rich blood to the myocardium. Epicardial coronary arteries can be seen on gross inspection of the heart; the major epicardial coronary arteries are listed below. Epicardial coronary arteries give rise to intramyocardial coronary arteries that dive below the surface of the myocardium, and the subendocardial coronary arteries that run along the inside of the heart chambers. The left main coronary artery (LCA) angles down and laterally to the left on the anterior aspect of the heart. It branches downward into the left anterior descending (LAD), and laterally into the circumflex artery (CxA). The LAD supplies arterial blood to the anterior walls of both ventricles, as well as the interventricular septum. The circumflex artery provides the blood flow to the lateral and dorsal walls of the left atrium and ventricle. Thus, complete blockage of the left main coronary artery would essentially deprive the entire left ventricular myocardium of oxygen rich blood flow. Unfortunately, the point of bifurcation of the LAD and CxA from the LCA is a prime site for the development of an atherosclerotic plaque. The Right coronary artery (RCA) supplies blood to the right side of the heart, and it gives rise to the posterior descending artery (PDA) to much of the posterior aspects of the myocardium. Coronary venous blood will eventually be emptied into the coronary sinus on the posterior aspect of the heart, which in turn empties this oxygen-depleted blood into the right atrium. The delivery of adequate amounts of oxygen rich blood to the myocardium is of extreme importance because the myocardium has a very limited ability to produce ATP via anaerobic metabolism. Thus, the heart is essentially an aerobic machine with a very high demand for ATP, and thus a very high demand for oxygen. The extreme aerobic capacity of the cardiac muscle cells is reflected in its large number of mitochondria and capillaries. Additionally, the myocardium usually takes up most of the available oxygen from the arterial blood, resulting in an arterio-venous oxygen difference of > 15 vols% at rest. Thus, any increase in the heart’s oxygen demands (myocardial oxygen demand, MVO2) must usually be met by increasing coronary blood flow. This coupling of metabolic needs of the heart with coronary blood flow is primarily a result of metabolically induced vasodilation (autoregulation) of the coronary arteries. Myocardial oxygen demand (MVO2) is often estimated by the Rate Pressure Product (RPP, sometimes called the double product). The RPP is calculated by multiplying the systolic blood pressure times the heart rate. It makes sense that the RPP can be used as an estimate of MVO2 because if the heart is beating more often (higher HR), or is beating harder (resulting in higher SBP), then one would expect that there is a greater oxygen demand. At rest the heart receives approximately ~250ml/min (5% of cardiac output). Blood flow to the ventricular myocardium occurs primarily during ventricular diastole (see Appendix 8-2). The great amount of pressure developed during ventricular systole compresses the subendocardial coronary arteries and thus results in great amount of resistance to coronary blood flow (resulting in reduced coronary blood flow, Flow = Pressure/resistance). Lab VIII - 4 During exercise the heart requires more oxygen. For example, at rest HR is ~70 beats per minute, and SBP ~120mmHg, resulting in a RPP of 8,400. During maximal exercise HR may be ~200 bpm, and SBP may normally increase to ~200mmHg, resulting in a rate pressure product of ~40,000, this represent an approximately five-fold increase in myocardial oxygen demand (MVO2). However, during exercise the duration of diastole is decreased in absolute time, and it is also decreased as a percentage of the cardiac cycle. In order to provide enough oxygen to meet the heart’s oxygen demands (MVO2), the coronary blood flow must increase dramatically. In fact coronary blood flow is three to five times greater at maximal exercise (~1000ml/min) than it is at rest. However, this presents a problem. How can the myocardium obtain adequate amounts of oxygen when there is less time to provide blood to the myocardium (less time in diastole), and it is already taking up almost all of the oxygen available to it? The answer is the coronary arteries must dilate during exercise in order to accommodate an increase in coronary blood flow (and thus increase delivery of oxygen to the myocardium). Most people associate CAD with old age and the elderly. However, evidence of the development of atherosclerotic plaques has been found even in babies who have died of accidental causes. By the time an individual reaches the age of 20-25 years of age, the diameter of their coronary arteries may already be reduced by 20-25%. However, because of the great ability of the coronary arteries to dilate, coronary blood flow is not significantly reduced until the coronary arteries are ~70-75% occluded (see Appendix 8-2). Thus, we associate CAD with old age because for most individuals it takes time (aging) before a significant reduction in coronary blood flow occurs. Coronary arteries that have developed substantial atherosclerotic lesions also do not dilate properly, and thus during exercise when MVO2 increases, the coronary arteries may not be able to provide enough blood (and thus oxygen) to the myocardium. A temporary lack of adequate blood flow is called ischemia, when one is discussing the temporary lack of adequate blood flow to the myocardium the term myocardial ischemia is usually used. It should be noted that ischemia is a lack of adequate blood flow relative to the oxygen demand; it is temporary and reversible. Myocardial ischemia can thus be reversed either by inducing vasodilation (often done pharmacologically, for example with nitroglycerine tablets) to increase oxygen delivery, or by reducing MVO2 (stop exercising, use a beta blocker, etc.) Myocardial ischemia often results in the stimulation of chemically sensitive afferent nerve endings around the heart. Many of these nerve endings join with other ascending nerve fibers from nocireceptors (pain receptors) in the skin around the chest, arms, neck, and/or back. Thus, a person often perceives pain in the chest, neck, arm, or back when the myocardium is not receiving enough oxygen. This type of referred pain is called angina pectoris (often just called angina). Stable angina is predictable; it usually has an onset during increased physical activity or exertion, and is thought to be representative of coronary flow limitations due to atherosclerosis. Unstable angina, on the other hand is not as predictable, and may be due to vasospasms or a transient blood clot (thrombosis) blocking one of (or some of) the coronary arteries. Vasospasms occur when the smooth muscle lining the coronary arteries “clamp down”. This often occurs with strong epinephrine-mediated stimulation of alpha-adrenergic receptors in the smooth muscles. If myocardial ischemia is not reversed it may result in damage to the myocardium (myocardial injury), and eventually necrosis (death) of cardiac muscle cells, and possibly causing a myocardial infarction (MI). Ischemia can also occur in peripheral blood vessels. Individuals with peripheral vascular disease (PVD) have atherosclerosis in their peripheral circulation. These individuals also tend to feel pain during exercise, but in their limbs, instead of their chest. This intermittent pain is called claudication and is due to ischemia in the periphery. Most PVD subjects complain of claudication in their lower legs and buttocks. Intermittent claudication is one of the major signs or symptoms suggestive of coronary artery disease (see Appendix). It stands to reason that if someone has Lab VIII - 5 atherosclerosis in their peripheral vasculature that they are likely to also have a significant atherosclerotic buildup in their coronary arteries. The Cardiac Cycle, Heart Rate, and Blood Pressure (see appendix page 6) At the beginning of left ventricular contraction (systole), the ejected blood flows faster going into the aorta than it does leaving the arterioles. As a result, the blood ejected by the ventricle faces the opposition of the blood remaining in the aorta from the previous ventricular ejection. The tension in the aortic wall increases as the vessel distends to accommodate more blood and as aortic and arterial pressures goes up. Following ventricular systole, the ventricle begins to relax (diastole), and the aortic valve closes. After the aortic valve closes there is an elastic recoil of the aortic walls, creating a notch in the aortic pressure curve. As blood is ejected and the pressure in the aorta increases, the pressure is transmitted to the arteries. When the aorta has its elastic recoil causing a second small surge in pressure, this also is transmitted to the arteries. When the ventricle is in diastole and the aortic pressure drops, so does the pressure in the arteries. Thus, the pressure changes in the heart and aorta dictate the pressures in the arteries. The pulses felt in arteries in the periphery (e.g. radial and carotid pulses) are caused by these pressure changes. Every time the heart beats and ejects blood, a pulse can be felt. Thus, the pulse can be used to determine how frequently one's heart is beating. One can easily feel (palpate) the pulse and determine its rate at body sites where large arteries lie near the skin or overlie bone. There are a number of sites where the arterial pulse can be easily palpated. The radial artery at the wrist is a commonly used site. One must be careful to separate heart rate from pulse rate because the two are not always identical. In some types of arrhythmias (abnormal electrical rhythm in the heart), some beats may be very weak and a pulse will not register at the wrist. The radial pulse rate would then be slower than the actual heart rate. In some cases (e.g. aortic aneurysm) the left and right radial pulses may even vary. Blood pressure is the driving pressure that causes blood to flow from high pressure to low pressure through our circulatory system (i.e. Left Ventricle Aorta Arteries Arterioles Capillaries Venules Veins Vena Cava Right Atria). In our laboratory experiments today, we will be talking about arterial blood pressure. Both blood pressure and blood flow in the aorta and other large arteries is pulsatile in nature. During left ventricular systole, arterial pressure increases and during ventricular diastole, it decreases. Systolic blood pressure (SBP) is defined as the peak pressure reached during ventricular systole. Diastolic blood pressure (DBP) is the lowest pressure reached during diastole of the ventricle. A normal value for systolic pressure for a 20year-old man is 120 mm Hg and for diastolic pressure, it is 80 mm Hg. The arterial pressure is conventionally written as systolic pressure over diastolic pressure (e.g. 120/80). These numbers tend to be lower in smaller individuals and in women. If systolic blood pressure is chronically elevated above 140 mmHg, and/or if the diastolic blood pressure is chronically elevated above 90 mmHg, the individual is said to have hypertention. Two other pressures used in cardiovascular physiology are pulse pressure (PP) and mean arterial pressure (MAP). Pulse pressure is defined as the difference between the systolic and diastolic pressures. It is normally between 40 and 50 mm Hg. Mean arterial pressure is the average pressure throughout the cardiac cycle and is calculated as diastolic pressure plus one third of the pulse pressure. Mean arterial pressure is normally between 90-100 mmHg. MAP = DBP + 1/3(PP) The mean blood pressure is a function of two factors: cardiac output and total peripheral resistance. Cardiac output (Q) is the amount of blood pumped out of the heart per minute, and it is usually about 5L/min at rest. During maximal exercise cardiac output may get as high as 20Lab VIII - 6 30L/min in an average individual, and may reach as high 50L/min in highly trained endurance athletes. Students should remember from their previous physiology courses that according to Poicelle’s law, resistance depends primarily upon the caliber (diameter/radius) of the blood vessels (i.e. vasoconstriction or vasodilation) and to some extent, perhaps, the viscosity of the blood. Total peripheral resistance (TPR) is the total resistance to blood flow provided by all of the blood vessels in the body. The relationship between MAP, Q, and TPR can be written mathematically as: MAP = Q x TPR The above equation is related to "Ohm's Law" which you have learned about in your human physiology course (and probably also your physics courses). Knowledge of this relationship between pressure, cardiac output (blood flow), and resistance (total peripheral resistance) is of great utility to clinicians and exercise physiologists. For example, hypertension is associated with high mean arterial pressure, but their cardiac outputs are usually normal (or sometimes lower), thus, hypertension is associated with higher than normal TPR. Cardiac output is determined by both the heart rate and the volume of blood ejected by the ventricle per beat, which is called the stroke volume. Thus cardiac output can be determined as: Q (L/min) = heart rate (beats/min) x stroke volume (L/beat) Stroke volume, as previously stated is the amount of blood pumped out of the ventricle per beat. However, it should be noted that not all blood that enters the ventricle will be pumped out. The stroke volume (SV) can be calculated as: SV (ml/beat) = EDV (ml) – ESV (ml) The end diastolic volume (EDV) is the amount of blood that fills the ventricle prior to systole (or at the end of diastole). Thus, the EDV is dependent mostly on venous return (amount of blood returning to the heart from the venous circulation) and the size of the ventricle. The end systolic volume , and on the other hand is the amount of blood left in the ventricle after systole, and determined, in part, by the strength of the ventricular contraction (i.e. if the ventricle contracts hard there will be less blood left in the ventricle after systole). The fraction of blood that enters the ventricle that is actually pumped out is called the ejection fraction. In healthy individuals, the ejection fraction should be greater than 50-55% at rest. In patient’s with heart failure, ventricular function may so compromised that ejection fraction can get as low as 15-20%. In healthy hearts the ejection fraction increases during exercise. The ejection fraction can be calculated as: EF% = SV / EDV Ischemia occurs when a tissue’s oxygen demand is greater than it’s oxygen supply. Myocardial ischemia occurs when the heart’s oxygen demand is greater than the oxygen supplied via coronary arteries. Atherosclerosis has the potential to decrease the lumen of the coronary arteries, and thus cause myocardial ischemia. Patients with a significant reduction in coronary artery blood flow as a result of atherosclerosis have coronary artery disease (CAD). The classic symptom of myocardial ischemia in such patients is chest pain or angina pectoris. In these individuals, myocardial ischemia most commonly occurs when the heart’s oxygen demand is increased above rest (such as during exercise). During exercise, blood flow in the coronary arteries increases, but in individuals with CAD, the increase in blood flow fails to meet the oxygen demand, and ischemia ensues. Clinically, it is useful, then, to have a way of estimating the myocardial (heart) oxygen demand (MVO2). MVO2 can be easily estimated if heart rate and blood pressures are known by calculating what is called the rate pressure product (RPP, also sometimes called the double product): RPP = HR x SBP Lab VIII - 7 The measurement of blood pressure provides valuable information regarding the pumping efficiency of the heart and the overall condition of the systemic blood vessels. It is generally stated that the systolic blood pressure indicates the force of contraction of the heart and that the diastolic pressure indicates the condition of the systemic blood vessels. Thus, the systolic blood pressure is often said to be more related to stroke volume and cardiac output, while the diastolic blood pressure is more related to the resistance provided by the blood vessels (TPR). It is possible to measure systolic and diastolic blood pressures directly by inserting a catheter into a blood vessel and attaching a pressure gauge. However, this direct method of measurement is not very practical or convenient. Indirect methods have been developed that are of acceptable accuracy. Indirect methods tend to underestimate direct methods. One indirect method of estimating systemic arterial blood pressure utilizes a stethoscope and a sphygmomanometer (blood pressure cuff). The sphygmomanometer is an inflatable rubber cuff with a pressure gauge attached to it. It is attached around a limb (usually arm) and as it is inflated, it collapses the artery underneath. A stethoscope bell is placed over the (brachial) artery distal to the cuff. When the pressure of the cuff exceeds the pressure in the artery, the artery is collapsed and blood flow through it ceases. As pressure in the cuff is reduced, blood flow through the artery begins at a cuff pressure just below systolic blood pressure. At this time, a sharp, tapping sound may be heard with the stethoscope over the artery. At this sound, cuff pressure is taken as an approximation of systolic blood pressure. The sounds that are heard are associated with turbulent blood flow in the blood vessel, due to the fact that the vessel is partially occluded. When a blood vessel is not occluded at all blood flow is very orderly, called laminar flow, which is usually completely silent. As pressure in the cuff is further reduced, the sounds made are more intense and then become suddenly muffled. This occurs at the level of diastolic blood pressure, where the artery remains open throughout the entire pulse cycle. Cuff pressure at the point of sound muffling is used as an approximation of diastolic blood pressure. As cuff pressure continues to be reduced, the sounds disappear completely and normal laminar flow through the vessel is reestablished. Since the disappearance of sound is easier to establish than muffling (especially if your subject is exercising), and since there is only a few millimeters of mercury pressure change between the two, the disappearance of sound is commonly used in determining diastolic pressure. The disappearance of sound is technically the end diastolic blood pressure. The sounds heard over the artery during blood pressure determination by the auscultatory method are known as Korotkoff sounds, named after Nikolai Korotkoff, a Russian physician, who first reported five phases of sound change in 1905. The phases of the Krotkoff sounds include: Phase 1. Appearance of a fairly sharp thudding sound that increases in intensity during the next 10 mm Hg decrease in pressure. The pressure when the sound first appears is the systolic blood pressure. Phase 2. The sounds become a softer murmur during the next 10 to 15 mm Hg of drop in pressure. Phase 3. The sounds become louder again and have a sharp thudding quality during the next 10 to 15 mm Hg of decreased pressure. Phase 4. The sounds suddenly become muffled and reduced in intensity. The pressure at this point is termed the diastolic blood pressure. If the subject is at rest, this muffled sound continues for another 5 mm Hg decrease in pressure. It is not uncommon to hear the Korotkoff sounds all the way down to 0 mmHg in healthy subjects during exercise, thus the initial point when the sound becomes muffled should be recorded as the DBP. However, it is often difficult to hear this change in sound quality when the subject is exercising, thus the fifth Korotkoff sound may be a more reliable indicator of diastolic blood pressure during exercise. Lab VIII - 8 Phase 5. The point at which the sound ceases completely (associated with laminar blood flow) is called the end diastolic blood pressure. It is sometimes recorded along with the systolic and diastolic pressures (e.g. 120/80/75) because the true diastolic blood pressure lies between the fourth and fifth sounds. Sometimes, if you are taking the blood pressure of a young, healthy subject during exercise, the sounds may be heard all the way down to 0 mmHg. The subject's diastolic blood pressure is not really 0 in this case. It should be remembered that sphygmomanometry is an indirect way of assessing blood pressure, and may not always be a hundred percent accurate. If the muffled sound (4th Korotkoff sound) is heard, it is probably a more accurate reflection of the diastolic blood pressure. But, because the 4th sound is sometimes difficult to hear, and may not be heard equally well by all clinicians, it is usually less reliable (different people would get different numbers). Thus, the 5th Korotkoff sound is commonly recorded as the diastolic blood pressure during exercise even though it is technically the end diastolic blood pressure. Note: The Korotkoff sounds should not be confused with heart sounds, they are completely different concepts. Krotkoff sounds are heard in arteries depending upon the presence or absence of turbulent blood flow, which depends upon whether or not the blood vessel is partially occluded or not. Heart sounds are heard around the heart, and are associated with opening or closing of heart valves (first and second heart sounds) , or with filling of the ventricles (third and fourth heart sounds). There are several different types of sphygmomanometers used for the indirect determination of blood pressure. The two most common types are aneroid and mercurial sphygmomanometers. The aneroid type is light and portable, and works by means of a spring-operated gauge. Internal parts that are susceptible to wear and tear and a relatively small indicator gauge making it sometimes difficult to read, are disadvantages for this type of sphygmomanometer. The mercurial blood pressure cuff uses a column of mercury to measure cuff pressure. This type of sphygmomanometer is more accurate, easier to use and contains no moving parts (except the column of mercury). Disadvantages for the mercurial sphygmomanometer include heaviness, size (larger than aneroid type), more easily broken, and when broken can spill the toxic mercury. Typically, when using the aneroid type of sphygmomanometer, as we will be using in lab, the blood pressures are recorded only in even numbers. Remember that MAP = 1/3PP + DBP, MAP = Q x TPR and Q = HR x SV, and there are a number of things that can affect HR, SV and TPR. If any of these variables change it will affect blood pressure. Because the SBP is the peak arterial pressure during ventricular systole it is more dependent upon stroke volume and cardiac output (Q) than it is on resistance (TPR), because systole is contraction of the ventricle and the SV is the result of this contraction. During diastole blood is not being pumped out of the left ventricle into the arterial circulation. Thus, the DBP is less dependent upon SV on Q than it is on resistance (i.e. the resistance is what keeps the arterial pressure from falling to 0 mmHg when blood is not being ejected into the arterial circulation). Cardiovascular Regulation We have already discussed the relationships between some of the many variables related to cardiovascular function (SV, HR, Q, MAP, TPR). In order to maintain homeostasis the body must maintain an adequate pressure gradient to pump freshly oxygenated blood (as well as other nutrients, hormones, etc.) to the body’s tissues and to remove metabolic by-products, such as CO2. If arterial pressure drops too low it will not be possible to move blood against the forces of gravity up to the brain or to perfuse the body’s tissues. The brain can not function without oxygen because it can not create ATP anaerobically. A number of complications can also arise from having chronically elevated high blood pressure (see hypertension below). In order to survive, blood Lab VIII - 9 pressure must be maintained within an appropriate range (homeostasis). In general the body responds to changes in pressure by changing cardiac output and/or by changing blood vessel radius (MAP = Q x TPR, and TPR is inversely related to the radius). Thus, if blood pressure gets too low, the body can respond with an increase in cardiac output and/or by constricting the blood vessel (decreasing the radius). A number of mechanisms regulate arterial pressure (only a few will be discussed). Some of these control mechanisms react very rapidly to pressure changes, while others provide long term regulation of arterial pressure. By far, the most rapid controls are the nervous pressure control mechanisms. Both branches of the autonomic nervous system affect blood pressure. A sympathetic nervous system activity is usually associated with increasing blood pressure by increasing cardiac output and/or by causing vasoconstriction of blood vessels. On the other hand if blood pressure is too high, and needs to be lowered, a decrease in sympathetic nervous system activity occurs, along with a concomitant activation of the parasympathetic nervous system, which tends to decrease heart rate. The integrating center for these neurally mediated cardiovascular reflexes is the cardiovascular regulatory centers in the medulla oblongata. One of the neural pressure control mechanisms, the baroreceptor feedback mechanism (see appendix page 13) involves pressure receptors (called pressoreceptors or baroreceptors) in the internal carotid arteries and aorta. Information from these receptors is integrated by the vasomotor center of the medulla. When body position changes (e.g. supine to standing), the baroreceptors send information to the medulla, which, in turn, sends signals to the heart and blood vessels in an attempt to maintain a relatively constant arterial pressure. As the body assumes a more vertical position, gravity pools blood in the lower extremities due to the effects of gravity on fluids, and there is a decrease in blood pressure in the carotid baroreceptor area. This elicits a baroreceptor reflex as neural activity leaving the baroreceptors decreases. This information is sent to the medulla, which responds by increasing sympathetic nervous system activity. This increased sympathetic activity produces vasoconstriction and an increased heart rate, thereby causing an increase in blood pressure. This minimizes the decrease in arterial pressure in the head and upper body. When there is an increased stimulation of the baroreceptors caused by an increased arterial pressure in the baroreceptor area, it results in an inhibition of vasoconstriction by the vasomotor center, as well as a decreased heart rate. During exercise the “set point” for the baroreceptors increases to a higher pressure, such that the higher pressures during exercise result in about the same discharege as rest. The chemoreceptor mechanism is another nervous pressure control mechanism which involves chemosensitive receptors located in the two carotid bodies and several aortic bodies that are stimulated by decreases in oxygen or increases in hydrogen ions and carbon dioxide in the arterial blood. These receptors are not very sensitive to oxygen, in fact, they do not respond unless the partial pressure of oxygen in the arterial blood drops to 60% of its normal value. Thus, increases in carbon dioxide and hydrogen ions in the blood are chemical causes of an increase in blood pressure. There are several other mechanisms related to blood pressure control, for example free nerve endings in skeletal muscles can respond to changes in carbon dioxide and hydrogen ions, and are thus able to affect blood pressure by sending signals to the medulla. The long term regulation of blood pressure is controlled by the kidneys, by altering blood volume. Not all regulation of blood pressure is controlled by the medulla, for example individual tissues have some ability to affect their own blood flow (autoregulation). Thus, if there is a local decrease in partial pressure of oxygen, decrease in pH, increase in temperature, increase in partial pressure of carbon dioxide, increase in potassium, or increase in the amount of ADP, vasodilation will occur. All of these factors are associated with metabolically active skeletal muscle, which requires an increased blood flow. Thus, when skeletal muscles start contracting, their blood flow increases in part due to local changes in these various chemicals, which results in vasodilation and the resulting decrease in resistance. Lab VIII - 10 Determining the Carotid & Radial Pulse When taking the carotid pulse, the examiner should use the three middle fingers to palpate the pulse and not the thumb since a clear, steady pulse is present in this digit. The pulse may be taken on either side of the subject's neck just under the back of the lower jaw beside the larynx. Using the three middle fingers, apply slight pressure by pressing inwardly and toward the back gradually until the carotid pulse is picked up. It should be pointed out that heavy pressure should be avoided not only because it is uncomfortable for the subject, but because there is a chance of erasing the carotid pulse with unnecessary pressure, and perhaps stimulating baroreceptors, which would tend to slow the heart rate via baroreflex. Count the carotid pulse for 15 seconds. When two consecutive counts are within one beat of each other, multiply the last 15-second count by four and record this as the pulse rate per minute. Other procedures may be used for pulse rate determinations in which frequency is counted for a specified number of seconds and is converted to a one minute value, e.g., pulse frequency for 10 seconds X 6 or 20 seconds X 3. Practice may be required before any accuracy can be achieved in counting pulse rate. When taking the radial pulse, examiner should use the three middle fingers to palpate the pulse and not the thumb since a clear, steady pulse is present in this digit. The pulse may be taken on either arm. Instruct the subject to hold their forearm with the hand palm up. The pulse can be felt over the radial artery that passes over the radius bone at the base of the thumb. The radial artery is found between a large tendon and the bony prominence which is located on the lateral side of the wrist. Too much pressure may eliminate the pulse. Count the radial pulse for 15 seconds. When two consecutive counts are within one beat of each other, multiply the last 15-second count by four and record this as the pulse rate per minute. Other adjusted pulse rate determinations may be used in which frequency is counted for a specified number of seconds and is converted to a one-minute value, e.g., pulse frequency for 10 seconds X 6 or 20 seconds X 3. Determine Arterial Blood Pressure Via Auscultation (see appendix page 7) When taking the arterial blood pressure, either arm may be used. Instruct the subject to keep the upper arm at approximately the level of the heart. The same arm should be used if more than one measure is to be taken. Body position should remain the same from measure to measure. Fasten the arm band snugly around the arm of the subject just above the elbow. Be sure that there are no unnecessary folds in the arm band. It should be mentioned that some cuffs have markings for both right and left arm and some have no such markings. At any rate, employ the center of the inflatable area of the cuff on the inside of the upper arm and roll the long end of the cuff about the limb. Place the gauge or mercury column where it can be easily seen. Locate the brachial artery in the forearm just above the elbow and place the stethoscope bell over the artery in or above the anticubital fossa of the elbow. Inflate the sphygmomanometer until the pressure is about 85-90 mm Hg (just above the diastolic pressure and below the systolic pressure). At this pressure there should be partial restriction of blood flow and flow sounds should be audible through the stethoscope. When measuring blood pressure the cuff pressure should be increased to about 130140mmHg. At this pressure no sounds should be audible. If you still hear blood flow sounds the pressure is not high enough and you need to increase the cuff pressure by another 20mmHg. This procedure will need to be repeated until no flow sounds are audible. This procedure will keep you from using pressures higher than are needed that are uncomfortable for your subject. Once the pressure is high enough to remove the flow sounds the artery will be occluded, the cuff should not be kept at this pressure for more than 2 minutes. Lab VIII - 11 To take the measurement, slightly open the valve and allow the pressure to fall slowly (2mm Hg/beat, Note: during exercise it may be necessary to take the blood pressure a bit faster so as not do disrupt the subject's movement pattern for very long). Listen carefully for the sound of the blood passing through the partially occluded artery and notice the pressure at which the first sound is detected. (It should sound like the beating of the heart.) This is the systolic blood pressure. If the first sound (systolic) is not heard the first time, the pressure should be increased and another reading taken. As the pressure decreases it will assume a muffled quality, this represents diastolic blood pressure. (If the examiner is unable to notice the change to muffled sound, the diastolic pressure may be recorded as the point at which all pressure sound disappears. However, it should be pointed out that the examiner must consistently use one signal or the other.) Practice may be required before any accuracy can be achieved in taking arterial blood pressure. It is necessary that near total quietness be demanded of the laboratory class and complete concentration of the examiner's part. Lab VIII - 12 LABORATORY PROCEDURES I. Demonstration: Normal, Restrictive, and Pulmonary conditions 1. Enter your subject’s information into the computer program. Subject characteristics such as gender, age, height, race, and smoking history will be used to calculate predicted values for the subject. Record the predicted values in the data sheet. 2. Place a nose clip on your subject and instruct the subject to wrap their lips around the mouthpiece in order to make a good seal over the mouthpiece. Then, have your subject perform a forced vital capacity maneuver. Instruct them to take 3-4 normal breaths followed by a maximal inspiration and then exhaling as forcefully and completely as possible followed by a maximal inspiration. This completes the procedure. If both the tester and the subject feel that it was a good test and a max effort was given, press yes to save the test results. A. Record the data in the data sheet. B. Draw an example of the spirograph, making sure to label each of the following: xaxis, y-axis, tidal volume, inspiratory reserve volume, expiratory reserve volume, inspiratory capacity, and vital capacity. Also, label an estimate of the FEV1 on the recording. C. Draw the flow-volume loop, making sure to label each of the following: x-axis, yaxis, tidal volume, inspiratory reserve volume, expiratory reserve volume, vital capacity, peak expiratory flow rate. 3. Restrictive pulmonary disease simulation. For this experiment we will have the subject exhale all of the air possible from their lungs and then wrap large straps around the subject’s chest. If the subject feels uncomfortable, remove the straps and estimate the data. Repeat the forced vital capcity maneuver as above, record the data, and draw sample spirograph and flow-volume loop. Remove the chest straps as soon as possible. 4. Obstructive pulmonary disease simulation. For this experiment we will have the subject breathe through a very small tube between the mouthpiece and the recording device. Repeat the forced vital capcity maneuver as above, record the data, and draw sample spirograph and flow-volume loop. II. Maximal Voluntary Ventilation (MVV) and the potential for pulmonary limitations to maximal exercise. 1. Have the subject perform a maximal voluntary ventilation procedure. This procedure requires the subject to breathe as deep and frequently as possible for 12 seconds. The resulting MVV will provide an estimate of the maximal amount of air that can be moved by the subject’s lungs in one minute. 2. Compare the subject’s MVV to their maximal VE from their VO2max test. Then answer the questions in the manual. III. Blood Pressures & Cardiovascular Disease Risk Factors, signs and symptoms (work in pairs) 1. Using a blood pressure cuff, sphygmomanometer, and stethoscope, determine your subject’s seated resting blood pressure as described previously in the lab manual. If you can hear the 4th Korotkoff sound, record the 1st, 4th, and 5th sounds. If the 4th sound is not noted simply record the 1st and 5th sounds as reflecting the SBP and DBP. Unless otherwise noted, we will use the DBP as determine using the 5th Korotkoff sound in our Lab VIII - 13 calculations for PP, MAP, etc. Take your subject’s pulse and determine their heart rate. Perform your calculations 2. With your partner, determine what major CVD risk factors are present? Where answers are unknown, estimate. In young, healthy, college students it is tempting to record blood lipids and others as normal if they are unknown. However, in clinical settings, when critical pieces of information are unknown, the worst should be assumed (risk is present). For this lab, blood glucose can be taken. However, it should be noted that it is not a fasting blood glucose, and if the subject has eaten recently (a meal or snack within past few hours), it is normal for blood glucose to be elevated. 3. With your partner, determine what major signs/symptoms suggestive of cardiovascular, pulmonary, or metabolic disease are present. This should be done by asking questions and/or physical examination. 4. Determine what risk stratification category your subject is in. IV. Blood Pressure Regulation 1. Effects of Posture on Blood Pressure. Determine your subject’s seated, standing, and supine blood pressures using the auscultory method. Allow your subject at least 2-3 minutes in each new position Perform calculations (work in pairs) (For all remaining experiments, work in groups of 4-5 students.) 2. Perform a modified “tilt test”. A tilt test can be used to determine if s subject has lost significant amounts of blood or if they are dehydrated. The modified tilt test is performed by taking the subject’s seated blood pressure (ideally in a real seated position with a normal chair) and then having them stand up. Start the stop watch or note the time when they stand up. Then, take their heart rate and blood pressure 1 minute after standing up. Unique cutoff points indicating that the subject is “tilt positive” (they have lost significant amounts of blood and/or are dehydrated) if heart rate increases by 20 bpm or if SBP decreases by more than 20 mmHg. However, these cutoffs are considered by some to be too conservative, and it is fairly common for army medics and military medical personnel to use cutoffs of a 10 bpm increase in HR and/or a 10mmhg decrease in SBP as cutoffs for a “tilt positive” test. If HR increases less than 10 mmHg and/or if SBP decreases by less than 10 mmHg we will consider the subject “tilt negative” (normal, not dehydrated, no/insignificant blood loss). This test also demonstrates the function of the baroreceptors and the baroreflex. Record your data and perform necessary calculations. 3. Cold Pressor Test. First take your subject’s seated heart rate and blood pressure. If your subject is hypertensive at rest use a different subject. Have the subject sit comfortably. Record the blood pressure and heart rate following 5 minutes of rest. Have the subject immerse the free (non-cuffed) hand in ice water (5 degrees Celsius) to a depth well above the wrist. 10-15 seconds after the immersion obtain (rapid) blood pressures and heart rates back to back for 1-2 minutes and record your readings. Try to get at least 3-4 readings during the test. What initially happens to heart rate and blood pressure? Does the blood pressure (and heart rate) eventually become normal after the immersion in ice water? If so, how long does it take? Explain the physiological mechanism involved in this process. Extreme cold can stimulate temperature sensitive nociceptors and therefore cause pain. In general, painful stimuli initiate fight or flight responses. The normal reflex response to a cold stimulus (or painful stimulus) is an increase in blood pressure (both systolic and diastolic). This occurs because the painful stimulus produces an Lab VIII - 14 overall systemic vasoconstriction, which elevates blood pressure. In normal subjects, the increase in blood pressure is detected by the baroreceptors, which reflexively bring about a lowering of blood pressure to compensate for the rise. If the baroreceptor reflex is working normally, the rise in blood pressure with cold will be held to 10 mm Hg. A hypertensive individual may experience a rise in blood pressure as high as 30 to 40 mm Hg. 4. Face Immersion and Diving (Bradycardia) Reflex. First take your subject’s seated heart rate and blood pressure. Bradycardia, induced by the diving reflex, can be used to demonstrate the effects of the parasympathetic nervous system. This reflex results from combined stimulation of cold temperature receptors and other sensory recpetors (on the face) associated with the trigeminal nerve. The response is greater when combined with apnea (cessation of breathing). To perform this experiment record heart rate and blood pressure after 2-3 minutes of rest and then have your subject submerge their face in a basin of room temperature water. The subject may breathe as needed; however some degree of breath holding is necessary for good results. Take your blood pressure and heart rate measurements after 2 minutes of face immersion (start pumping up cuff after a minute and 40 seconds or so). Make sure you do not take a measurement within the first 5-10 seconds following a breath. Try and get 3 measurements within 3 minutes. This response is believed to be due to face immersion and/or to breath holding. This reflex has been observed in all vertebrates that have so far been tested for this response. The general response is a slowing of the heart rate with an increase in blood pressure (How can MAP increase if HR and Q decrease?). This response is believed to be protective in nature. That is, since the body does not know when it will get its next breath of fresh air, the body tries to decrease blood flow to all organs except the heart and brain (which are both almost exclusively aerobic). This decrease in blood flow and oxygen uptake by all of our other organs means that oxygen supply to our most important organs (heart and brain) can be maintained longer, and the organism can survive longer under water. 5. Have your subject perform a valsalva maneuver while seated. A valsalva maneuver is performed by trying to exhale against a closed glottis. The subject should be trying to forcefully exhale without actually expiring. This maneuver can usually only be maintained for approximately 20-30 seconds. Pump the cuff up to around 200mmHg just prior to the beginning of the Valsalva maneuver. Once the subject has started the Valsalva, the pressure in the cuff can be released and the blood pressure should be obtained fairly quickly (within the first 10 seconds). Determine heart rate using the pulse oximeter or a heart rate monitor. If the subject can hold the valsalva longer than that, try and get a second blood pressure. In taking the blood pressures very rapidly you will need to sacrifice accuracy for speed of measurement. 6. Determine your subject’s heart rate and blood pressure during a steady state, moderate intensity exercise bout. Complete your calculations and questions. Lab VIII - 15 DATA SHEETS I. Demonstration: Normal, Restrictive, and Pulmonary conditions A. Data 1 predicted 2 Normal 3 Restrictive 4 Obstructive FVC FEV1 FEV1/FVC FEF25-75% B. Draw examples of the spirograph for each condition below C. Draw in each flow-volume loops below Normal Restrictive Lab VIII - 16 Obstructive PEFR i. How did the subject’s normal values compare to the predicted values? Was there any evidence of obstructive or restrictive pulmonary disease from the normal recording? ii. Of what value are the “predicted” values? Why are they needed? What do you think would be major determinants of the predicted vital capacity? iii. Which values are different (indicate if higher or lower) between normal and obstructive? iv. Which values are different (indicate if higher or lower) between normal and restrictive? v. How did the spirographs compare between the different conditions? vi. How did the flow-volume loops compare between conditions? II. MVV and the potential pulmonary limitations to maximal exercise. A. What was the highest VE recorded during your subject’s VO2max test? __________ B. What was your subject’s MVV? ______________ C. How did these numbers compare? If the subject needed to ventilate more during the VO2max test, could they have increased ventilation? D. Does the subject appear to have a pulmonary limitation to maximal exercise? If so, what evidence is there? E. What other variables might be assessed to evaluate possible pulmonary limitations to maximal exercise? F. What type of individual might you expect to have a pulmonary limit to maximal exercise performance? Lab VIII - 17 III. Blood Pressures & Cardiovascular Disease Risk Factors, signs and symptoms (work in pairs) 1. Blood pressures: A. Seated blood pressure #1: _______ / _________ / _________ Seated heart rate #1: _______ PP: MAP: RPP B. Seated blood pressure #2: _______ / _________ / _________ Seated heart rate #2: ______ PP: MAP: RPP C. Does the subject have normal blood pressure, prehypertension, or hypertension? 2. CVD risk factors indicate subject’s values (and clinically relevant cutoffs) Positive Risk Factors A. Age B. Family History (Hx) C. Cigarette smoking D. Sedentary lifestyle E. Obesity (see BMI and waist data from earlier labs) F. Hypertension (see data above) G. Dyslipidemia H. Prediabetes Subject’s blood glucose: _______ Time since subject last ate: ________ Negative Risk Factors I. High HDL Cholesterol What is the difference between positive and negative risk factors? If your subject had a family history, smoked, a blood pressure of 142/82 and an HDL of 64 mg/dL (all others are normal), how many risk factors would they have? . Lab VIII - 18 3. Major signs/symptoms suggestive of cardiovascular, pulmonary, or metabolic disease Determine if subject has the sign/symptom and write a brief description of what it is and what it may indicate. When asking your subject/partner about each practice putting into laypersons’s terms. A. Angina Pectoris (describe clinically relevant features) B. Shortness of Breath (SOB) C. Dizziness/Syncope D. Orthopnea/Paroxysmal Nocturnal Dyspnea E. Ankle Edema F. Palpitations/Tachycardia G. Intermittent Claudication H. Known heart murmur I. Fatigue/SOB 4. Risk stratification category: A. Is your subject low, moderate, or high risk? Explain your answer. B. How will this subject’s risk category influence your clinical decision making? (e.g. could you/would you do a maximal exercise test with them? If so, should a physician be present? Would you recommend they begin an intense exercise regimen? Lab VIII - 19 IV. Blood Pressure Regulation Experiments 1. Effects of Posture A. Supine blood pressure: _______ / _________ / _________ heart rate: _______ PP: MAP: RPP B. Seated blood pressure: _______ / _________ / _________ heart rate: _______ PP: MAP: RPP C. Standing blood pressure: _______ / _________ / _________ heart rate: _______ PP: MAP: RPP D. How did blood pressure compare between the different postures? How do you think posture/body position might influence the cardiovascular response to exercise? 2. Modified Tilt Test A. Seated blood pressure: _______ / _________ / _________ heart rate: _______ B. 1 min after standing up blood pressure: _______ / _________ / _________ heart rate: _______ C. Was the subject tilt positive? If so, what is a possible reason why? Lab VIII - 20 D. Describe the events that lead to these changes in blood pressure and heart rate. Make sure to use the following terms (some may/should be used more than once): gravity, blood pooling, venous return, end diastolic volume, stroke volume, cardiac output, MAP, medulla oblongata, sympathetic nervous system, parasympathetic nervous system, vasoconstriction and/or vasodilation, TPR, heart rate, and homeostasis. Flow charts are helpful (and fun!). 3. Cold Pressor Test. A. Normal seated - HR - ____________ BP - _______/________ MAP _________ B. Cold pressor test measurements (try to get 3-4 of them back-back within 2 minutes) time _________- HR - ____________ BP - _______/________ MAP ________ time _________- HR - ____________ BP - _______/________ MAP ________ time _________- HR - ____________ BP - _______/________ MAP ________ time _________- HR - ____________ BP - _______/________ MAP ________ C. . What happened to Heart Rate and MAP initially during the cold pressor test? explain the observed changes in HR and MAP. E. Name/draw the parts of the reflex arc (receptor, integrating center, type of efferent neurons, effector organs) involved in the initial portion of this reflex. F. Did the HR and MAP eventually return, or begin to return, to normal? If so, Name/draw the parts of the reflex arc (receptor, integrating center, type of efferent neurons, effector organs) involved in this second phase of this reflex. G. Would you consider your subject’s response a hypertensive response? Lab VIII - 21 H. In what way(s) is the cardiovascular response during this reflex similar and different from the cardiovascular response to exercise? What does this suggest about the cardiovascular response to exercise? 4. Diving Reflex. A. Normal seated - HR - ____________ BP - _______/________ MAP _________ B. Diving reflex (try to get 3-4 of them back-back within 2 minutes) time _________- HR - ____________ BP - _______/________ MAP ________ time _________- HR - ____________ BP - _______/________ MAP ________ time _________- HR - ____________ BP - _______/________ MAP ________ time _________- HR - ____________ BP - _______/________ MAP ________ C. What happened to Heart Rate and MAP initially during the face immersion? Explain the observed changes in HR and MAP. D. How might this reflex effect exercise in water? E. What branch of the autonomic nervous system is responsible for this change in HR? F. What branch of the autonomic nervous system is responsible for this change in MAP? G. How might these cardiovascular adjustments improve our ability to survive while submerged? H. How do we estimate the heart’s oxygen demand? What happened to the myocardial oxygen demand during the diving reflex? How might this benefit the organism when submerged? Lab VIII - 22 5. Valsalva. A. Normal seated - HR - ____________ BP - _______/________ MAP _________ B. Valsalva (try to get 2 of them back-back within 30 seconds) time _________- HR - ____________ BP - _______/________ MAP ________ time _________- HR - ____________ BP - _______/________ MAP ________ C. What happened to MAP in the first phase of the valsalva? What likely caused this response? What happened to RPP during this first phase? D. What happened to pulse pressures in the second phase of the valsalva? What likely caused this response? E. What does this suggest about working with people, some of whom might be hypertensive, when performing resistance exercise? 6. Moderate exericse. A. Normal seated blood pressure: _______ / _________ / _________ heart rate: _______ PP: MAP: RPP B. exercise blood pressure: _______ / _________ / _________ heart rate: _______ PP: MAP: RPP C. What happened to each of the following and what does each represent? SBP DBP PP MAP RPP Lab VIII - 23 Study questions 1. List the major cardiovascular disease risk factors, indicating relevant cutoff numbers for each. Indicate which factors are modifiable, and which ones are likely to be influenced by physical activity? 2. List six major signs/symptoms suggestive of cardiovascular, pulmonary, and/or metabolic disease. What problem, condition do each of these suggest may be present? 3. Which is worse? Having a major sign/symptom suggestive of cardiovascular disease or having a risk factor for cardiovascular disease? 4. What is the difference between morbidity and mortality? 5. What steps can you take to reduce your likelihood of, or at least delay the onset of, developing coronary artery disease? 6. Although heart rate is not directly proportional to blood pressure, the relationship between heart rate and blood pressure is demonstrated by what two formulas? What formulas define the relationship between Heart Rate and VO2? 7. Why/how does respiration (the mechanics of moving air in and out of the lungs) directly affect the cardiovascular system? Lab VIII - 24 8. What role does posture (e.g. supine vs standing) play in determining heart rate and blood pressure? What adjustments are made to accomplish these changes and what causes these adjustments to occur? How do you think posture would affect HR and BP response to exercise? 9. What are normal resting values for HR, Q, SV, EF%, SBP, and DBP? Are there different values between trained and untrained subjects? 10. What evidence can be used to determine if a subject has a pulmonary limitation to maximal exercise performance? 11. Explain why we use the BTPS correction factor? 12. How can one diagnose obstructive and restrictive pulmonary diseases during pulmonary function testing? What data should one look at? How are spirographs and flow-volume loops different in these conditions? 13. Name several types of obstructive and restrictive pulmonary diseases. 14. Briefly explain, in your own words, how we simulated obstructive and restrictive pulmonary diseases in class. 15. Knowing what you know about the relationship between pressure, flow and resistance and between resistance and radius of the conducting tube (bronchiole or blood vessel), use mathematical formulas to describe why flow rates are reduced during an asthma attack. Lab VIII - 25 16. Large elite endurance athletes typically have a much larger vital capacity (VC) than untrained subjects. However, training studies have generally found no change in VC with exercise training. What does this suggest about elite endurance athletes, the importance of VC for performance, and training adaptations? 17. If your subject has a TLC of 6.0 L, an FRC of 2.5 L, an RV of 1.5L, and a perfectly average TV, calculate IC, IRV, ERV, VC? 18. Considering that TV increases during exercise, what happens to IRV and ERV during exercise? Considering the lung volumes and capacities, what is the largest volume of air that a person could move in one breath at rest or during exercise? 19. Considering your career goals, how might information from this lab influence your decision making when working with your patients, athletes, colleagues, and/or family members? 20. In normal subjects, if Q increases at least 4-5 fold between rest and maximal exercise when performing running or cycling, why doesn’t MAP increase 4-5 fold? 21. If your subject’s heart is beating once every minute and their heart is pumping out six liters of blood every minute and sixty five percent of the blood in their ventricle at the end of diastole is pumped out every beat and the highest arterial pressure recorded during systole is one hundred and thirty four and the lowest arterial pressure recorded during ventricular diastole is seventy six millimeters of mercury, what are the subject’s: HR, SV, Q, MAP, EDV, ESV, RPP, and TPR? Lab VIII - 26