Functional Nutrition Protocol, IBS Revised
advertisement

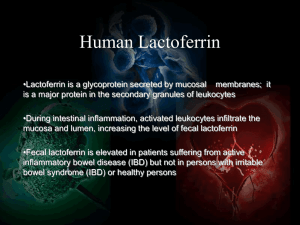
Functional Nutrition Intervention Protocols IRRITABLE BOWEL SYNDROME SSESSMENT Anthropometrics Biomarkers/Labs Conventional Height, weight, BMI Waist circumference, hip circumference, waist-to-hip ratio % body fat, % lean body mass R/O gastrointestinal tract cancer R/O celiac disease Iron status, folate/B12 status, protein status, vitamin D Functional Comprehensive stool analysis, intestinal permeability RBC essential fatty acids Food sensitivity testing (IgG or Mediator Release Testing) Nutrigenetic As appropriate, such as inflammation profile, Phase I/Phase II detoxification profile Clinical Indicators Nutrition-focused physical exam Diet/Lifestyle Histories Comprehensive intake form Include Medical Symptom Questionnaire IAGNOSIS NTERVENTION Irritable bowel syndrome IFM 5R Program for Gastrointestinal Dysfunction Core Food Plan Balanced core food plan Food Plan Modifications 21-day Comprehensive Elimination Diet + anti-inflammatory foods + elimination of any foods promoting GI reactions Functional Foods/Medical Foods Soluble fiber foods, such as oatmeal/oat bran, cooked or canned fruits and vegetables Anti-inflammatory medical food Dietary Supplements Vitamins High quality daily multivitamin with chelated minerals If using antacid or proton pump inhibitor, replenish vitamin B12, folate Minerals Replace if patient using antacids or protein pump inhibitors or labs indicate need: Ca, Cr, Fe, I, Mg, Mn, Se, Zn 75 mg Zn short-term may help with intestinal permeability Nutritionals L-glutamine, 10-40 g/day, taken between meals, increase gradually, caution with individuals with bipolar disorder Irritable Bowel Syndrome Page 1 of 2 Functional Nutrition Intervention Protocols Dairy-free probiotics, 30-100 billion colony-forming units of Lactobacillus and Bifidobacter bacteria in divided doses daily; increase gradually; accompany with soluble fiber Omega-3 fatty acids, 2-4 g/day Bovine colostrum may be helpful, from herds certified to be free of bovine spongiform encephalopathy (BSE) Botanicals Anti-inflammatory herbs: boswellia, 400 mg tid; ginger (root), 1-4 g/d; turmeric (root), 500 mg/d standardized to 95% curcuminoids, willow (bark), 60-240 mg salicin/d Carminative herbs: peppermint tea; enteric-coated peppermint oil, 180-200 mg tid between meals Promote healing: Aloe vera juice (aloes-free), 50 ml (~6 oz) tid; DGL (deglycyrrhizinated licorice), 200 mg standardized extract (1-2% glycyrrhizin) tid Food/Medication/Dietary Supplement Interactions Lifestyle Recommendations Physical Activity Aloe vera may cause hypoglycemia Daily activity, as tolerated, preferably outdoors (sunshine) Yoga and other mindfulness activities Sleep Full complement, as determined for individual patient Psycho-social Stress assessment, management program Encourage social connections, activities that are meaningful and pleasurable for the individual ONITORING and Follow-up Plan VALUATING Periodic contact by functional nutrition practitioner Return to clinic in 3 weeks to begin food reintroduction Primary source of dietary supplement information: Natural Standard Database Drisko J, Bischoff B, Hall M, McCallum R. Treating irritable bowel syndrome with a food elimination diet followed by food challenge and probiotics. J Am Coll Nutr. 2006;25:514-22. Irritable Bowel Syndrome Page 2 of 2