HISTOLOGY ENDOCRINE SYSTEM PROF.DR. HUDA AL
advertisement

HISTOLOGY
ENDOCRINE SYSTEM
PROF.DR. HUDA AL-KHATEEB
Lec.1
Endocrine system is the system that regulates the tissue activities
by a secretory product (hormone)
Tissue activities include:
1. Coordination of growth and development
2. Adaptation to external and internal environmental stresses
3. Processes of sexual reproduction
Hormones are chemicals that are released ( from an endocrine cell )
in a small amount , directly to the blood or tissue fluids. They usually
act on special cells that are called Target cells.
Target cell is a cell that possesses a specific receptors for a certain
hormone.
Receptors are special sites that are located extra- or intra-cellular
(depending on the type of hormone).
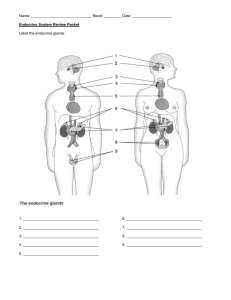
Classification of endocrine system
I. Typical endocrine glands – includes
1. Pituitary gland
2. Suprarenal gland ( adrenal gland)
3. Thyroid gland
4. Parathyroid gland
5. Pineal body
II. Scattered endocrine masses
1. Islets of Langerhans – in the pancreas
2. Corpus luteum – in the ovary
3. Interstitial cells of Leydig – in the testis
4. Placental lactogen secreting cells - in theplacenta
5. Chorionic gonadotropin secreting cells – in the placenta
6. Juxtaglomerular cells – in the Juxtaglomerular
apparatus of the kidney
III. Isolated endocrine cells ( also called Diffuse Neuroendocrine
System) (also called APUD cells – Amine Precursor Uptake and
Decarboxylation cells)
They are present principally within the lining epithelium of
the digestive and respiratory system.
Examples of APUD cells:
G-cell that secrets gastrin
I-cell that secrets cholicystokinin and pancreozymine
N-cell that secrets neuroscretin
S-cell that secrets secretin
A-cell that secrets glucagon
k-cell that secrets gastric inhibitory peptide
B-cell that secrets insulin
PP-cell that secrets pancreatic polypeptide
D-cell that secrets somatostatin
In a multicellular organism, cell communications are mediated by
chemical messengers via:
I- Autocrine activity – a cell secrets a chemical messenger that acts
on its own receptors. Example: epidermal growth factor cause
local control of cell growth, or influences the activity of the same
cell type. Example:prostaglandin
II- Paracrine activity – a cell influence a nearby cell. Example: D –
cell (somatostatin secreting cell) of islet of Langerhans acts on
the adjacent A – cell (glucagon secreting cell) . the end result is
somatostatin will inhibit glucagon secretion.
III- Endocrine activity – a cell acts on a distant (far) cells. Example: G
–cell (gastrin secreting cell) present in the pyloric region of
stomach and duodenum , secrets gastrin to blood. Gastrin acts
on stomach leads to increase in secretion of gastric gland and
increase motility of stomach.
IV- Synaptic secretion – present in the nerve ending. Example:
acetylcholine
Endocrine system varies in its embryonic origin, some are:
1. Ectodermal origin – example: pituitary gland
2. Mesodermal origin – example: gonads (ovary and testis)
3. Endodermal origin – example: thyroid, parathyroid glands and
pancreas
Histology of endocrine cells:
A. Light microscopical study: generally, endocrine cells (glands,
masses and scattered cells) are polyhedral and usually arranged
in cords and separated by fenestrated capillaries or sinusoids.
B. Electron microscopical study – the electron microscopical
features of endocrine cells depends on the type of hormone it
secret.
Hormones are classified according to their chemical structure into 3
classes, these are:
1. Steroid hormones – (example: testosterone, estrogen,
progesterone and adreno-cortico-tropic hormone – ACTH).
Ultrastructurally, steroid hormone secreting cells are
characterized by :
Abundant smooth endoplasmic reticulum
Numerous mitochondria (large number of mitochondria)
Large amount of lipid droplets
Steroid hormones usually leave their synthesizing cells by
diffusion through cell membrane. They inter their target cells by
diffusion through its cell membrane (some inter through intranuclear
membrane too), where they meet their specific intracytoplasmic or
intranuclear receptors.
2. Protein hormones – (example: prolactin, growth hormone,
insulin). Electron microscopical study of a protein hormone
secreting cell shows that they are:
Rich with rough endoplasmic reticulum
Large Golgi apparatus
Many secretory granules
Protein hormones are usually synthesized as a large
molecules called 'Prohormones' (inactive form of hormone), then
shortened to an active hormone either before storage in the secretory
granules or prior to exocytosis of the secretory granules.
Protein hormones leave their synthesizing cells by exocytosis.
Their specific receptors lie on the cell membrane of their target cells.
Hormone-receptor interaction will activate adenylate cyclase (cell
membrane enzyme). Activated adenylate cyclase will convert ATP to
cAMP (acts as a second messenger to produce the biological activity in
the target cell).
3. Peptide hormones – {example: thyroxin, epinephrine (adrenalin)
and norepinephrine (noradrenalin)}
By electron microscope exam, these cells reveal numerous tinny
storage granules and abundant mitochondria.
Peptide hormones leave their synthesizing cell by diffusion and
inter their target cell by diffusion through its cell membrane and
intranuclear membrane to meet their specific intranuclear
receptors.
HISTOLOGY
Prof.Dr. Huda Al-khateeb
Lec. 2
ENDOCRINE SYSTEM
Pituitary gland (Hypophysis)
Pituitary gland is a small bean-shape organ. Its
dimensions are (12x10x9 mm)
It weighs 0.5gm in male. It is slightly heavier in nonpregnant and much heavier in pregnant women.
It lies beneath the base of the brain (hypothalamus) to
which it is linked by stalk.
It is enclosed in the sella turcica of the sphenoid bone
(sella turcica is an important radiological land mark).
Pituitary gland has double embryological origin
1. From the oral ectoderm – the roof of the mouth
cavity will invaginate cranially forming a pouch
called "Rathke's pouch". Later this part detaches
from the oral cavity and forms the
adenohypophysis.
2. From the developing nervous system – the floor of
diencephalon will evaginate caudally. Later it will
form the neurohypophysis.
Therefore pituitary gland can be divided into:
A. Adenohypophysis – subdivided into:
Pars distalis (Anterior lobe)
Pars tuberalis ( Cranial part)
Pars intermedia (Intermediate lobe)
B.Neurohypophysis – subdivided into:
Pars nervosa (Posterior lobe)
Stalk (Infundibulum) – composed of median
eminence and stem
Pars distalis (Ant. Lobe): composed of two types of cells:
a) Chromophobes (50%)
b) Chromophils – subdivided into
i. Acidophils (40%)
ii. Basophils (10%)
Chromophobes:
Light microscopical study of Chromophobes shows:
Small polyhedral cells with pale cytoplasm and small
rounded central nucleus.
Their cytoplasm has no affinity to dyes and has no
granules
Cells are usually found in clusters
Their function is unknown, they are thought to be:
i. Either exhausted degranulated chromophils
ii. Or represent immature chromophils
Chromophils:
Light microscopical study of chromophils manifests:
Large polyhedral cells with large acidophilic (in
acidophils) or basophilic (in basophils) granules.
They have large central rounded nucleus.
Electron microscopic study of chromophils:
Acidophils and basophils are sub-grouped according to
the size of granules (in the cytoplasm) seen in the
electron microscope.
Acidophils – subgrouped into:
1. Somatotrophs – (secretory granules = 300 – 400 nm),
they are responsible for growth hormone (GH)
secretion. GH influences the general body growth and
bone elongation (by its effect on the epiphyseal
cartilage of long bones).
Note: the increase of GH in childhood and adolescent
leads to gigantism, while the increase of GH, in adults,
leads to acromegaly. The reduction in GH in childhood
leads to dwarfism.
2. Mammotrophs – (secretory granules = 200 nm)
They are responsible for prolactin secretion. This
hormone stimulates milk synthesis and secretion from
mammary gland during lactation in female. In male, its
role is not well understood.
Recently, it has been found that these cells secret
luteotrophic hormone (LTH), which stimulates corpus
luteum of the ovary to secret progesterone.
Basophils – are subdivided according to their electron
microscopical features into:
1) Gonadotrophs – (secretory granules = 250 – 400 nm).
The secret the following hormones:
Follicular – stimulating hormone (FSH) – stimulates
folliculogenesis in female and spermatogenesis in male.
Leuteinizing hormone (LH) – in female, it is
responsible for maturation of follicles in ovary,
ovulation and corpus luteum formation.
Interstitial cell – stimulating hormone (ICSH) – in
male, it maintains interstitial cells of Leydig in testis
and stimulates them to secret androgens, particularly,
testosterone which is essential for sperm maturation
and development of secondary sex organs.
2) Thyrotrophs – (secretory granules = 120 – 200 nm)
They are responsible for secretion of thyroid –
stimulating hormone (TSH) which stimulates thyroid
gland to secret tetraiodothyronin (Thyroxine) (T4) and
triiodothyronin (T3).
3) Corticotrophs – (secretory granules = 400 – 550)
They secret adreno-cortico-trophic hormone (ACTH).
This hormone acts on the adrenal gland cortex, leading
to secretion of corticosteroid hormones (aldosterone
and cortisol) and sex hormones (estrogen, progesterone
and androgen).
Recently, it has been found that these cells are
responsible for the secretion of β-lipotropin hormone
(β-LPH), α-melanocyte-stimulating hormone (α-MSH)
and β-endorphins.
Pars Intermedia:
In human, it is a rudimentary region made up of
cords and follicles of weakly basophilic cells that
contains secretory granules. It might be responsible
for the secretion of α-melanocyte-stimulating
hormone (α-MSH)
Pars Tuberalis:
It is a sleeve like that surround the infundibulum. Its cells
are arranged in cords alongside the blood vessels. Most of
them secret gonadotropins (FSH & LH).
Neurohypophysis: composed of:
Pars nervosa (posterior lobe)
Infundibulum: with its stalk attached to the
hypothalamus at the median eminence
All parts of neurohypophysis contain Pituicytes and axonal
processes of unmyelinated nerve fibers whose cell bodies are
located in the paraventricular and supraoptic nuclei of the
hypothalamus. The axonal processes converge at the median
eminence forming a bundle called "hypothalamohypophyseal tract" and pass through the infundibulum to
reach pars nervosa. These nerve fibers are unusual in that
they do not end on other neuron or effector cells, but end
blindly close to the fenestrated capillary plexus of pars
nervosa. The terminal portions of these axonal processes are
commonly expanded and contain secretory granules called
Herring bodies or called neurosecretory bodies. The
neurosecretory bodies contain numerous membrane-
enclosed granules with either oxytocin or vasopressin bound
to carrier proteins called neurophysin I and II respectively.
Oxytocin and vasopressin are believed to be synthesized in
the cell bodies and then transported through the axons to the
nerve terminals where they are released in response to
hypothalamic nerve impulses. Axons from the supraoptic
nuclei are mainly concerned with vasopressin/ADH
secretion, whereas most of the fibers from the
paraventricular nuclei are concerned with oxytocin
secretion.
Oxytocin stimulates the contraction of the uterine smooth
muscles during child birth. It also stimulates the contraction
of Myoepithelial cells of the acini of mammary gland leading
to milk ejection.
Vasopressin increases water permeability of renal collecting
ducts leading to more water reabsorption which cause
increase in blood volume. It stimulates the contraction of
smooth muscles of the small-size arteries and arterioles
leading to increase of blood pressure.
Pituicytes are
Star-shaped glial cells
Supporting
Have cytoplasmic processes that surround the axons.
Blood supply of pituitary gland:
Pituitary gland receives blood from:
i. Right and left superior hypophyseal arteries that
are derived from circle of Willis and supply
infundibulum then anterior lobe by hypophyseal
portal system
ii. Right and left inferior hypophyseal arteries that
are derived from the internal carotid arteries and
supply neurohypophysis.
Blood, from all pituitary lobes, drain into superior and
inferior hypophyseal veins.
Hypophyseal portal system:
Both superior hypophyseal arteries break up into primary
capillary plexus (located near neurosecretory neurons that
contain releasing and inhibiting hormones). Capillaries of
this plexus join to form hypophyseal portal vein that break
up into secondary capillary plexus within adenohypophysis.
Both capillary plexuses are fenestrated with diaphragms.
HISTOLOGY
Prof.Dr. Huda Al-khateeb
Lec. 3
ENDOCRINE SYSTEM
ADRENAL (SUPRARENAL) GLANDS
They are paired, flattened, triangular bodies that are located
superior to the superior pole of the kidney. Both glands are
weighing 8 gm. They are approximately 5x4x1 cm in
diameter.
Adrenal gland is enclosed by a dense connective tissue
capsule. Its stroma is composed of rich network of reticular
fibers that support the secretory cells.
Suprarenal gland has two parts that are of different
embryonic origin, these are:
1. Cortex (90%) – derived from the genital ridge of the
mesoderm.
2. Medulla (10%) – derived from neural crest cells.
Adrenal cortex:
It is subdivided into three concentric layers, which are not
sharply defined (because they are derived from the same
embryonic origin). These are:
a) Zona glomerulosa
b) Zona fasciculata
c) Zona reticularis
Note: all cells of the adrenal cortex reveal ultrastructurall
features of steroid-hormone secreting cells.
Zona glomerulosa: characterized by being:
Thin outer layer (15%) that is located just under the
capsule
Light microscopical exam shows that its cells are
pyramidal and arranged in rounded or arched groups
that are surrounded by capillaries.
Their nuclei are rounded and central while cytoplasm
is lightly basophilic
These cells are responsible for secretion of
mineralocorticoids mainly aldosterone (controls
electrolytes –Na+ & K+ - homeostasis and water
balance).
Zona fasciculata:
It is the thickest layer (65 – 80%) of the adrenal cortex
Cells are large polyhedral with rounded central
nucleus and pale foamy cytoplasm. These cells are
arranged in parallel columns of 1or 2 cells thickness.
Columns usually run in right angle to the capsule.
Cells' columns are separated by sinusoidal capillaries.
The cytoplasm of zona fasciculata cells contains
numerous lipid droplets that contain neutral fats, fatty
acids, cholesterol and phospholipids. These substances
represent precursors for steroid hormones.
During slid preparation (by typical histological
procedures) lipid is extracted, thus gives vacuolated or
spongy appearance to these cells and that's why they
are called Spongyocytes.
Zona fasciculata cells secret the following hormones:
i. Glucocorticoids (mainly cortisol and cortisone),
which influence the carbohydrate, lipid and
protein metabolism.
ii. Gonadocorticoids (sex hormones - small amount
of androgens).
Zona reticularis:
Thin layer (10%) that lies between zona fasciculata and
medulla. It consists of small rounded cells that are arranged
in branching and anatomizing cords. Cells have rounded
central nucleus and deeply basophilic cytoplasm (because
they contain fewer lipid droplets and more lipofuscin
pigment). This layer secrets the weak androgen
(dehydroepiandrosterone - DHEA) which is converted to
testosterone in several other tissues.
MEDICAL APPLICATION
Because of the feedback mechanism controlling the adrenal
cortex, patients who are treated with corticoids for long
periods should never stop taking these hormones suddenly:
because, secretion of ACTH in these patients is inhibited,
and thus the cortex will not be induced to produce
corticoids, causing severe drops in the levels of sodium and
potassium.
Fetal Adrenal Cortex
At birth in humans (but not most other mammals) the adrenal
gland is larger than that of the adult and produces up to 200
mg of corticosteroids per day, twice that of an adult. At this
age, a layer known as the fetal or provisional cortex,
comprising 80% of the total gland, is present between the thin
permanent cortex and an under-developed medulla. The fetal
cortex is thick and contains mostly cords of large, steroidsecreting cells under the control of the fetal pituitary. The
principal function of the cells is secretion of sulfated DHEA
which is converted in the placenta to active estrogens (and
androgens), which mostly enter the maternal circulation. The
fetal adrenal cortex is an important part of a fetoplacental unit
which affects both endocrine systems during pregnancy but
whose physiological significance remains largely unclear.
After birth, the provisional cortex undergoes involution while
the permanent cortex organizes the three layers (zones)
described above.
Adrenal Medulla
The adrenal medulla is composed of large, pale-staining
polyhedral cells arranged in cords or clumps and supported
by a reticular fiber network. A profuse supply of sinusoidal
capillaries intervenes between adjacent cords and a few
parasympathetic ganglion cells are present. When medullary
cells are exposed to an oxidizing agent such as potassium
bichromate (K2Cr2O2), caticholamines (adrenalin and
noradrenalin) will be oxidized giving a brown coloration to
their cytoplasm, therefore these cells are called chromaffin
cells and the reaction is called Chromaffin reaction.
Chromaffin cells can be considered modified sympathetic
postganglionic neurons, lacking axons and dendrites and
specialized as secretory cells.
Unlike cells of the cortex, medullary chromaffin cells
contain many electron-dense granules, 150–350 nm in
diameter, for hormone storage and secretion. These granules
contain one or the other of the catecholamines, epinephrine
or norepinephrine. Ultrastructurally the granules of
epinephrine-secreting cells are less electron-dense and
generally smaller than those of norepinephrine-secreting
cells.
Norepinephrine-secreting cells are also found in paraganglia
(collections of catecholamine-secreting cells adjacent to the
autonomic ganglia) and in various viscera. The conversion of
norepinephrine to epinephrine (adrenalin) occurs only in
chromaffin cells of the adrenal medulla. About 80% of the
catecholamine secreted from the adrenal is epinephrine.
Medullary chromaffin cells are innervated by cholinergic
endings of preganglionic sympathetic neurons, from which
impulses trigger hormone release by exocytosis. Epinephrine
and norepinephrine are released to the blood in large
quantities during intense emotional reactions, such as fright,
and produce vasoconstriction, increased blood pressure,
changes in heart rate, and metabolic effects such as elevated
blood glucose. These effects facilitate various defensive
reactions to the stressor (the fight-or-flight response).
During normal activity, the adrenal medulla continuously
secretes small quantities of the hormones.
MEDICAL APPLICATION
One disorder of the adrenal medulla is pheochromocytoma, a
tumor of its cells that causes hyperglycemia and transient
elevations of blood pressure.
Disorders of the adrenal cortex can be classified as
hyperfunctional or hypofunctional. Tumors of the adrenal
cortex can result in excessive production of glucocorticoids
(Cushing syndrome) or aldosterone (Conn syndrome).
Cushing syndrome is most often (90%) due to a pituitary
adenoma that results in excessive production of ACTH; it is
rarely caused by adrenal hyperplasia or an adrenal tumor.
Excessive production of adrenal androgens has little effect in
men, but precocious puberty (in boys) and hirsutism
(abnormal hair growth) and virilization (in girls) are
encountered in prepubertal children.
Adrenocortical insufficiency (Addison disease) is caused by
destruction of the adrenal cortex in some diseases. The signs
and symptoms suggest failure of secretion of both
glucocorticoids and mineralocorticoids by the adrenal cortex.
Blood supply
1. Superior suprarenal artery – from phrenic nerve
2. Middle suprarenal artery – from aorta
3. Inferior suprarenal artery – from renal artery
These arteries inter adrenals at various points of the capsule
to form subcapsular plexus, from which three groups of
arteries arise:
i. Arteries that supply the capsule
ii. Arteries of the cortex – branch repeatedly to form
capillaries that drain to medullary capillaries
iii. Arteries of the medulla – they pass through the cortex
to reach the medulla then give rise to medullary
capillaries
All capillaries later drain to suprarenal veins.
Thyroid gland
Embryologically, it is derived from the cephalic portion
of the alimentary canal (endoderm)
It is located in the cervical region, anterior to larynx
and trachea
It has two lobes that are connected to each others by
the isthmus
It is covered by connective tissue capsule
Thyroid gland section is composed of thyroid follicles
that are filled with gelatinous substance called colloid
Follicular wall is composed of cells called follicular
cells which range from squamous to low columnar
epithelium, according to their secretory activity.
Follicular
cells
secret
both
Thyroxine
(tetraiodothyronin) (T4) and triiodothyronin (T3)
Between follicles, there is loose connective tissue that
contains Parafollicular cells (also called C-cells) which
are large, pale, polyhedral cells that secret calcitonin
(suppress bone resorption by osteoclasts. Calcitonin
secretion is triggered by elevated blood Ca2+ levels).
MEDICAL APPLICATION
A diet low in iodide hinders the synthesis of thyroid
hormones, causing increased secretion of TSH and
compensatory growth of the thyroid gland, a condition
known as iodine deficiency goiter. Goiters are endemic in
some regions of the world, where dietary iodide is scarce
and addition of iodide to table salt is not required.
Hypothyroidism in the fetus may present at birth as
cretinism, characterized by arrested or retarded physical
and mental development
Parathyroid glands
they are four small glands, their total weight = 0.4 gm
(0.1 each)
they lie within the capsule of thyroid gland one at each
end of the upper and lower poles
Embryologically, they are derived from pharyngeal
pouches; the two superior parathyroid glands are
derived from the fourth pouch, while the two inferiors
from the third one. each parathyroid gland is covered
by connective tissue capsule
Two types of cells are present in parathyroid glands:
chief (or principal) cells and oxyphil cells. The chief
cells are small polygonal cells with round nuclei and
pale-staining,
slightly
acidophilic
cytoplasm.
Ultrastructurally the cytoplasm is seen to be filled with
irregularly shaped granules 200–400 nm in diameter.
These are secretory granules containing the
polypeptide parathyroid hormone (PTH), a major
regulator of blood calcium levels. Much less, often
clustered, populations of oxyphil cells are sometimes
present, more commonly in older individuals. These
are much larger than the principal cells and are
characterized by acidophilic cytoplasm filled with
abnormally shaped mitochondria. Some oxyphil cells
show low levels of PTH synthesis, suggesting these cells
are transitional derivatives from chief cells.
Parathyroid hormone targets osteoblasts, which
respond by producing an osteoclast-stimulating factor
to increase the number and activity of osteoclasts. This
promotes resorption of the calcified bone matrix and
the release of Ca2+, increasing the concentration of Ca2+
in the blood, which suppresses parathyroid hormone
production. Calcitonin from the thyroid gland inhibits
osteoclast activity, lowering the blood Ca2+
concentration and promoting osteogenesis. Parathyroid
hormone and calcitonin thus have opposing effects and
constitute a dual mechanism to regulate blood levels of
Ca2+, an important factor in homeostasis. Parathyroid
hormone also indirectly increases the absorption of
Ca2+ from the gastrointestinal tract by stimulating the
synthesis of vitamin D, which is necessary for this
absorption.
Pineal body (gland) (Epiphysis cerebri)
It regulates the daily rhythms of bodily activities.
It is a very small, pine cone-shaped organ in the brain
measuring approximately 5–8 mm in length and 3–5
mm at its greatest width and weighing about 150 mg.
The pineal develops with the brain from
neuroectoderm in the roof of the diencephalon and is
found in the posterior of the third ventricle, attached to
the brain by a short stalk.
The pineal gland is covered by connective tissue of the
pia mater, from which emerge septa containing small
blood vessels and subdividing various sized groups of
secretory cells as lobules.
The prominent and abundant secretory cells are the
pinealocytes, which have slightly basophilic cytoplasm
and large, lobulated nuclei and prominent nucleoli.
Ultrastructurally pinealocytes are seen to have
secretory vesicles, many mitochondria, and long
cytoplasmic processes extending to the vascularized
septa, where they end in dilatations near capillaries,
indicating an endocrine function. These cells produce
melatonin, a low molecular-weight tryptophan
derivative. Unmyelinated sympathetic nerve fibers
enter the pineal gland and end among pinealocytes,
with some forming synapses.
Interstitial glial cells resemble astrocytes. They have
elongated nuclei more heavily stained than those of
pinealocytes, long cytoplasmic processes, and are
usually found in perivascular areas and between the
groups of pinealocytes. Pineal astrocytes represent only
about 5% of the cells in the gland.
A characteristic feature of the pineal gland is the
presence of variously sized concretions of calcium and
magnesium salts called brain sand, which form by
precipitation around extracellular protein deposits.
Accumulations of brain sand are opaque to x-rays and
allow the pineal to serve as a good midline marker in
radiological and computer-assisted tomography studies
of the brain.
Melatonin release from pinealocytes is promoted by
darkness and inhibited by daylight and the resulting
diurnal fluctuation in blood melatonin levels induces
rhythmic changes in the activity of the hypothalamus,
pituitary gland, and other endocrine tissues that
characterize the circadian (24 hours, day/night)
rhythm of physiological functions and behaviors.