Hematology Case Study 3 - Cal State LA
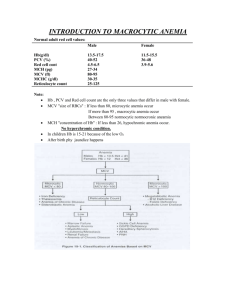
advertisement

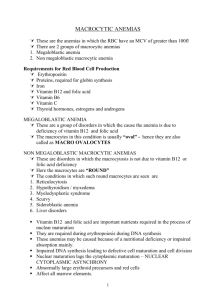
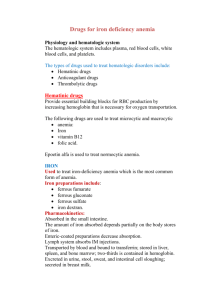
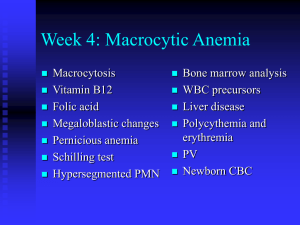
Hematology Case Study 3 Ms. Kate Allison, a 36-year-old female, experienced a recent 35-pound weight loss. Her tongue was red and fissured. She also complained of chronic fatigue and shortness of breath upon exertion. Physical examination suggested signs of jaundice and decreased fibratory sensation of fingers and toes. She was hospitalized with a general diagnosis of moderate anemia, jaundice, and neurological symptoms. Her admitting CBC demonstrated the following laboratory results: WBC: RBC: HGB: HCT: MCV: MCH: MCHC: RDW: PLT: 4.5 x109/L 2.50 x 1012/L 10.0g/dL 31 % 124.0 fL 40.5 pg/dL 32.7 gm/dL 21.2 155 x 109/L Differential: Lymphocyte % Monocytes % Neutrophils % Eosinophils % Basophils % 36.0 3.8 59.4 1.0 0.0 NRBCs/100 WBCs: 5 Moderate number of hypersegmented neutrophils The following abnormal erythrocyte morphology was reported (on a scale of 1-4): Macrocytes: 2+ Anisocytosis 3+ Poikilocytosis: 2+ Ovalocytes: 1+ Basophilic stippling: 1+ Occasional Howell-Jolly bodies 1. What is the morphological classification of the patient’s anemia? Macrocytic Based on the initial CBC results, further testing was ordered with the following results: B12: Folate: Total bilirubin *AST: *ALT: <50 pg/mL 10.3 ng/mL 2.5 mg/dL 35 U/mL 30 U/mL (Low) (Normal) (High) (Normal) (Normal) *These are liver enzymes that may increase with liver damage. Examination of a bone marrow aspirate revealed an erythroblastic hyperplasia with megaloblastic normoblasts. 2. Based on the information obtained so far, what is the most likely diagnosis? There is a vitamin B12 deficiency. The patient was admitted with signs of a moderate hemolytic anemia and neurological symptoms. Her CBC shows that she has a macrocytic anemia. Her leukocyte and platlet counts are the lower end of the normal range, indicating a developing pancytopenia. The blood smear revealed hypersegmented neutrophils, ovalocytes and Howell Jolly bodies. Her bilirubin values support a diagnosis of hemolysis. On a differential diagnosis, neurological symptoms typically accompany B12 deficiency rather than a folate deficiency. Based on her serum vitamin B12 and folate results, she can definitively be diagnosed as having a megaloblastic anemia due to a vitamin B12 deficiency. 3. What is the significance of the AST/ALT results? There is no liver disease. Since the liver enzymes are normal, liver disease is rules out as a source of jaundice or the macrocytic anemia. 4. What further testing can be done to obtain a definitive diagnosis? Testing for antibodies against intrinsic factor, Schilling test, gastric analysis. A common cause of vitamin B12 deficiency in a patient with no previous gastrointestinal history is pernicious anemia. The Schilling test can determine if the deficiency is due to absence of intrinsic factor, or some malabsorption disorder. A Schilling test and antibody test were done with the following results: Schilling Test: Part I, before intrinsic factor: 1% Part II, after intrinsic factor: 8% (Normal is >7.5%) Intrinsic factor blocking antibodies: Positive to a titer of 1:6400 5. What is the patient’s definitive diagnosis? Pernicious anemia. The Schilling test result in Part I showed less than 7% of the initially radioactively tagged radioactive dose of oral vitamin B12 in the urine 24 hours later. When the test was repeated with intrinsic factor, a greater amount of radioactive B12 was found in the urine 24 hours later. The diagnosis of PA is supported by the finding of intrinsic factor blocking antibodies in her blood. 6. How would the diagnosis change if the special testing results were as follows? Schilling Test: Part I, before intrinsic factor: 1% Part II, after intrinsic factor: 3% Intrinsic factor blocking antibodies: Negative The diagnosis is not PA. The vitamin B12 deficiency is due to some other malabsorption disorder. An abnormal Schilling test result following part II with oral intrinsic factor and the absence of autoantibodies suggest that the vitamin B12 deficiency was due to some sort of malabsorption disorder such as Crohn’s disease. 7. What would you predict the patient’s reticulocyte count to be? Normal to low. Megaloblastic anemia results from ineffective erythropoiesis with intramedullary hemolysis, which decreases the normal number of reticulocytes. In addition, reticulocytosis was not seen in the peripheral smear.