189, Tests for intestinal malabsorption
advertisement
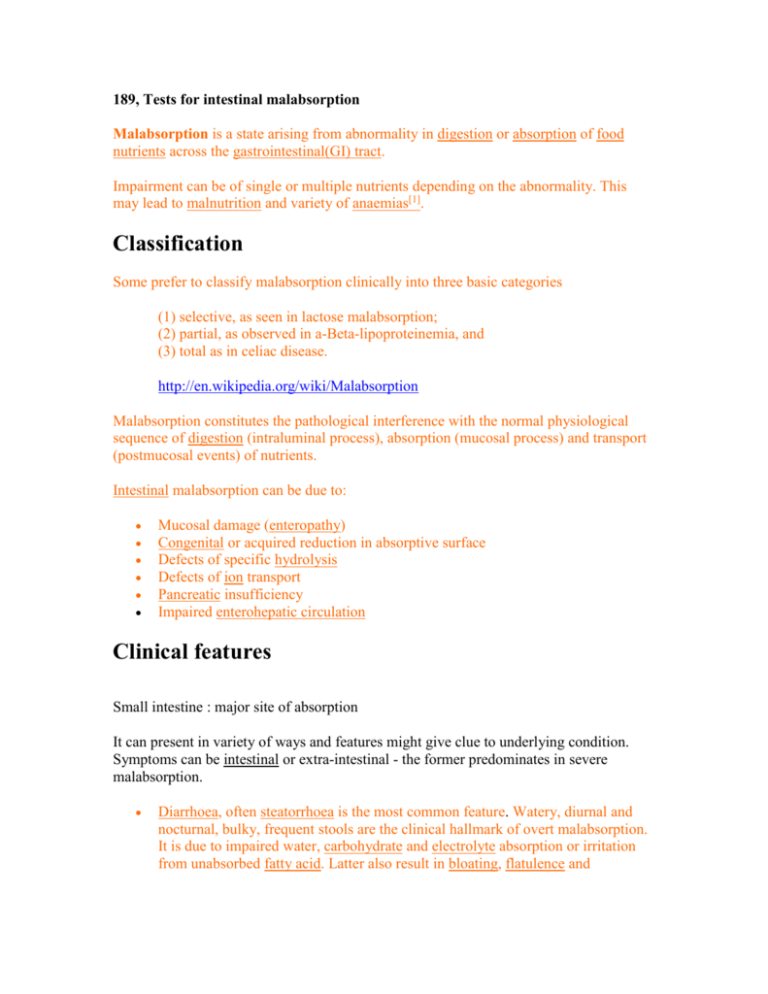
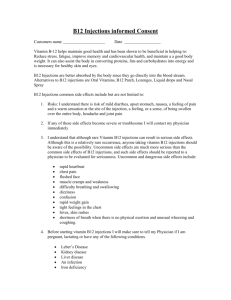
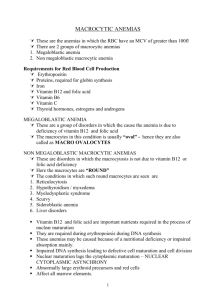
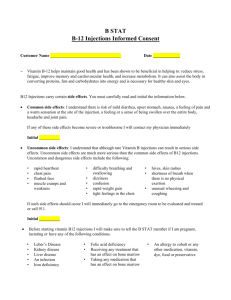
189, Tests for intestinal malabsorption Malabsorption is a state arising from abnormality in digestion or absorption of food nutrients across the gastrointestinal(GI) tract. Impairment can be of single or multiple nutrients depending on the abnormality. This may lead to malnutrition and variety of anaemias[1]. Classification Some prefer to classify malabsorption clinically into three basic categories (1) selective, as seen in lactose malabsorption; (2) partial, as observed in a-Beta-lipoproteinemia, and (3) total as in celiac disease. http://en.wikipedia.org/wiki/Malabsorption Malabsorption constitutes the pathological interference with the normal physiological sequence of digestion (intraluminal process), absorption (mucosal process) and transport (postmucosal events) of nutrients. Intestinal malabsorption can be due to: Mucosal damage (enteropathy) Congenital or acquired reduction in absorptive surface Defects of specific hydrolysis Defects of ion transport Pancreatic insufficiency Impaired enterohepatic circulation Clinical features Small intestine : major site of absorption It can present in variety of ways and features might give clue to underlying condition. Symptoms can be intestinal or extra-intestinal - the former predominates in severe malabsorption. Diarrhoea, often steatorrhoea is the most common feature. Watery, diurnal and nocturnal, bulky, frequent stools are the clinical hallmark of overt malabsorption. It is due to impaired water, carbohydrate and electrolyte absorption or irritation from unabsorbed fatty acid. Latter also result in bloating, flatulence and abdominal discomfort. Cramping pain usually suggest obstructive intestinal segment e.g. in Crohn's disease, especially if persists after defecation. Weight loss can be significant despite increased oral intake of nutrients. Growth retardation, failure to thrive, delayed puberty in children Swelling or oedema from loss of protein Anaemias, commonly from vitamin B12, folic acid and iron deficiency presenting as fatigue and weakness. Muscle cramp from decreased vitamin D, calcium absorption. Also lead to osteomalacia and osteoporosis Bleeding tendencies from vitamin K and other coagulation factor deficiencies. Low serum tryptophan and clinical depression, as can happen with fructose malabsorption Diagnosis/Tests There is no specific test for Malabsorption. As for most medical conditions, investigation is guided by symptoms and signs. Moreover, tests for pancreatic function are complex and varies widely between centres. Blood Tests Routine blood tests may reveal anaemia, high ESR or low albumin; which has high sensitivity for presence of organic disease. In this setting, microcytic anaemia usually implies iron deficiency and macrocytosis can be from impaired folic acid or B12 absorption or both. Low cholesterol or triglyceride may give clue toward fat malabsorption as low calcium and phosphate toward osteomalacia from low vitamin D. Specific vitamins like vitamin D or micro nutrient like zinc levels can be checked. Fat soluble vitamins (A, D, E & K) are affected in fat malabsorption. Prolonged prothrombin time can be from vitamin K deficiency. Serological studies Specific tests are carried out to determine underlying cause. IgA tissue trans glutamate or IgA antiendomysium assay for gluten sensitive enteropathy. Stool studies Microscopy is particularly useful in diarrhoea, may show protozoa like giardia, ova, cyst and other infective agents. Fecal fat study to diagnose steatorrhoea is less frequently performed nowadays. Low elastase is indicative of pancreatic insufficiency. Chymotrypsin and pancreolauryl can be assessed as well Radiological studies Barium follow through is useful in delineating small intestinal anatomy. Barium enema may be undertaken to see colonic or ileal lesions. CT abdomen is useful in ruling out structural abnormality, done in pancreatic protocol when visualising pancreas. Magnetic resonance cholangiopancreatography (MRCP) to complement or as an alternative to ERCP Interventional studies Biopsy of small bowel showing coeliac disease manifested by blunting of villi, crypt hyperplasia, and lymphocyte infiltration of crypts. Endoscopy is frequently undertaken, but to visualise small intestine, which can be up to 7m long, is indeed a daunting task. OGD to reveal duodenal lesion also for D2 biopsy (for celiac disease, tropical sprue, Whipple's disease, A-b-lipoproteinemia etc.) Enteroscopy for enteropathy and jejunal aspirate and culture for bacterial overgrowth Colonoscopy is helpful in colonic or ileal lesion. ERCP Other investigations Radio isotope tests e.g. 75SeHCAT, 95mTc to exclude terminal ileal disease. Sugar probes or sub 51Cr-EDTA to determine intestinal permeability. Glucose hydrogen breath test for bacterial overgrowth D-xylose absorption test. http://en.wikipedia.org/wiki/Malabsorption In animal medicine, xylose is used to test for malabsorption by administering to the patient in water after fasting. If xylose is detected in blood and/or urine within the next few hours, it has been absorbed by the intestines. After Xylose has been catalytically hydrogenated, it turns into a natural sugar substitute called Xylitol. This new sugar, along with Xylose itself, is a reducing sugar. http://www.answers.com/topic/xylose-1 Lower level in urine after ingestion indicates bacterial overgrowth or reduced absorptive surface. normal in pancreatic insufficiency. Bile salt breath test to determine bile salt malabsorption. Schilling test http://en.wikipedia.org/wiki/Malabsorption The Schilling's test is a medical investigation used in patients with vitamin B12 deficiency. The purpose of the test is to determine if the patient has pernicious anemia. Process There are a few variations on the exact procedure used. In the first part of the test, the patient is given radiolabeled vitamin B12 to drink. The most commonly used radiolabels are 57Co and 58Co. An intramuscular injection of unlabeled vitamin B12 is given at around the same time. The purpose of this injection is to saturate tissue stores with normal vitamin B12 to prevent radioactive vitamin B12 binding in body tissues, so that if absorbed, it will pass into the urine. The patient's urine is then collected over the next 24 hours to assess the absorption. Normally, the ingested radiolabeled vitamin B12 will be absorbed into the body. Since the body already has liver receptors for transcobalamin/vitamin B12 saturated by the injection, much of the ingested vitamin B12 will be excreted in the urine. A normal result shows at least 5% of the radiolabelled vitamin B12 in the urine over the first 24 hours. In patients with pernicious anemia or with deficiency due to impaired absorption, less than 5% of the radiolabeled vitamin B12 is detected. If an abnormality is found, the test is repeated, this time with additional oral intrinsic factor. If this second urine collection is normal, this shows a lack of intrinsic factor production, or pernicious anemia. A low result on the second test implies abnormal intestinal absorption (malabsorption), which could be caused by coeliac disease, biliary disease, Whipple's disease, fish tapeworm infestation (Diphyllobothrium latum), or liver disease. Malabsorption of B12 can be caused by intestinal dysfunction from a low vitamin level in-and-of-itself (see below), causing test result confusion if repletion has not been done for some days previously. In some versions of the Schilling's test, B12 can be given both with and without intrinsic factor at the same time, using different cobalt radioisotopes 57Co and 58Co, which have different radiation signatures, in order to differentiate the two forms of B12. This allows for only a single radioactive urine collection. Note that the B12 shot which begins the Schilling's test is enough to go a considerable way toward treating B12 deficiency, so the test is also a partial treatment for B12 deficiency. Also, the classic Schilling test can be performed at any time, even after full B12 repletion and correction of the anemia, and it will still show if the cause of the B12 deficiency was intrinsic-factor related. In fact, some clinicians have suggested that full folate and B12 replacement be normally performed before a Schilling's test is done, since folate and B12 deficiencies are both known to interfere with intestinal cell function, and thus cause malabsorption of B12 on their own, even if intrinsic factor is being made. This state would then tend to cause a false-positive test for intrinsic factor-related B12 malabsorption. Many labs have stopped performing the Schilling's test, due to lack of production of the cobalt radioisotopes and labeled-B12 test substances. Diagnoses Part 1 test result Part 2 test result Diagnosis Normal - Normal Low Normal Pernicious anemia Low Low Malabsorption http://en.wikipedia.org/wiki/Schilling_test Lactose H2 breath test for lactose intolerance Hydrogen breath test In a hydrogen breath test, after an overnight fast, 50 grams of lactose (in a solution with water) are swallowed. If the lactose cannot be digested, enteric bacteria metabolize it and produce hydrogen. This, along with methane, can be detected in the patient's breath by a clinical gas chromatograph or a compact solid state detector. The test takes about 2 to 3 hours. A medical condition with similar symptoms is fructose malabsorption. In conjunction, measuring the blood glucose level every 10 - 15 minutes after ingestion will show a "flat curve" in individuals with lactose malabsorption, while the lactase persistent will have a significant "top", with an elevation of typically 50 to 100% within 1 - 2 hours. However, given the need for frequent blood drawns, this approach has been largely supplanted by breath testing. http://en.wikipedia.org/wiki/Lactose_intolerance References http://en.wikipedia.org/wiki/ Plagiarism sources: 64.6% (je to celý opsaný z en.wiki)