Anemia

Anemias in children
Anemia…
… abnormal low hemoglobin, hematocrit or
RBC count, lower than the age-adjusted reference range for healthy children.
Anemia…
… abnormal low hemoglobin, hematocrit or
RBC count, lower than the age-adjusted reference range for healthy children.
Etiologic classification
I Impaired red cell formation
A/ Deficiency
Decreased dietary intake
Increased demand
Decreased absorption
Increased loss
B/ Bone marrow failure
Failure of a single or all cell lines
Infiltration
C/Dyshematopoietic anemia
II Blood loss
III Hemolytic anemia
Corpuscular (membrane, enzymatic or hemoglobine defects)
Extracorpuscular (immune, idiopathic)
Diagnosis of Anemia
detailed history careful physical examination peripheral blood smear
red cell morphology
MCV
RDW (red cell distribution width)
WBC and platelet morphology
Additionally:
-bone marrow evaluation
-additional testing
History
-
Diet ( iron , folate, vitB12 intake, onset of hemolysis after certain foods –e.g.,fava beans)
- family history ( transfusion requirements of relatives, splenectomy, gallblader disease )
- environmental exposures (lead poissoning)
-
- symptoms (headache, exertion dyspnea, fatigue, dizziness, weakness, mood or sleep disturbances, tinnitis) melena, hematemesis, abdominal painchronic blood loss
Physical Examination
Pallor
(skin, oral mucosa, nail beds)
Jaundice -hemolysis tachycardia tachypnea orthostatic hypotension venous hum systolic ejection murmur
peripheral edema?
Splenomegaly?
Hepatomegaly?
Glossitis?
gingival pigmentation?
Adenopathy?
Facial, extremity examination
Peripheral Blood Components important! Different values dependent on age!
RBC
Hgb
HCT
MCV – 80 – 100 fl/L (a calculated value)
MCH
RDW
Reticulocyte Count
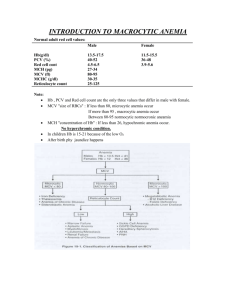
MCV for Characterize Anemia
-
(>85fl)
Low(<70 fl)
* Macrocytic
* Hypochromic/Microcytic
Normal newborn
Iron deficiency anemia
Increased erythropoesis
-Thalassemia
-Sideroblastic anemia
-Chronic infection
-Lead poisoning
-Inborn errors of Fe metabolism
Post splenectomy
Liver disease
Aplastic anemia
Megaloblastic anemia
Down S.
Obstructive jaundice
-Severe malnutrition
-Copper deficiency
Normocytic
Acute blood loss
Infection
Renal failure
Connective tissue disorders
Liver disease
Disseminated malignancy
Early iron deficiency
Aplastic anemia
Bone marrow infiltration
Dyserythropoietic anemia
Megaloblastic anemia
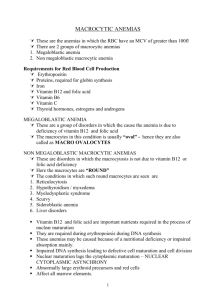
Presence the megaloblasts in the bone marrow and macrocytes in the blood
In > 95% occurs as a result of folate and vitamin B12 deficiency
Deficiencies of ascorbic acid, tocopherol, thiamine may be related to megaloblastic anemia
Dietary vitamin B12 (cobalamine) is required from animal sources (meat and milk)
Causes of vitamin B12 deficiency
I Inadequate dietary intake (<2mg/day) –malnutrition, veganism, maternal deficiency
II Defective vitamin B12 absorption
Failure to secrete intrinsic factor
Failure to absorption in small intestine
III Defective vitamin B12 transport
IV Disorders of vitamin B12 metabolism (congenital, acquired)
Folic acid deficiency
One of the most common micronutrient deficiences in the word (next to iron deficiency)
Component of malnutrition and starvation
Women are more frequently affected than men
Folate sufficiency prevents neural tube defects
Low mean daily folate intake is associated with twofold increased risk for preterm delivery and low infant birth weight
Causes of folic acid deficiency
Inadequate intake (method of cooking, special diet, goat’ milk)
Defective absorption (congenital or acquired)
Increased requirements (rapid growth, chronic hemolytic anemia, dyserythropoietic anemias, malignant disease, hypermetabolic state, cirrosis, post –BMT)
Disorders in folic acid metabolism (congenital, acquired)
Increased excretion
Clinical features of cobalamine and folate deficiency
Insidious onset: pallor, lethargy, fatigability, anorexia, sore red tongue and glossitis, diarrhea
History: similarly affected sibling, maternal vitamin B12 deficiency or poor maternal diet
Vitamin B12 deficiency: signs of neurodevelopmental delay, apathy, weakness, irrability, athetoid movements, hypotonia, peripheral neuropathy, spastic paresis
Megaloblastic Anemias:
Clinical Findings
• Anemia is slow to develop
• Fatigue
• Weakness
• Yellow color
• Weight loss
• Glossitis
Megaloblastic Anemia:
Lab Features: Hematology
Macrocytic, normochromic anemia
Increased MCH: due to large cell volume
Normal MCHC
RBC, HGB, Hct decreased
Granulocytes and Thrombocytes are affected as well.
Granulocytes are hypersegmented
Megakaryoctyes are abnormal resulting in thrombocytopenia
Megaloblastic Anemia:
Lab Features: Peripheral blood
Triad of oval macrocytes,
Howell-Jolly bodies and hypersegmented neutrophils
Anisocytosis, Poikilocytosis
RBC’s are fragile, lifespan is shortened and many die in the bone marrow which causes ↑ LDH
Megaloblastic Anemia:
Lab Features: Misc
Bone marrow
Hypercellular with megaloblastic erythroid precursors
M:E ratio decreased
Chemistries
Vitamin B12
Folate
Methylmalonic acid
(MMA)
Homocysteine
Lactic dehydrogenase(LDH)
Diagnosis
Red cell changes: Hgb usually reduced,
MCV increased to levels 110 – 140fl., MCHC normal, in blood smear many macrocytes and macro-ovalocytes, anisocytosis, poikilocytosis, presence of Cabot rings, Howell-Jolly bodies, punctate basophilia
White blood cell count reduced to 1500 – 4000/mm 3 , neutrophils show hypersegmentation (>5 lobes)
Platelets count moderately reduced (50,000 – 180,000/mm 3 )
Bone marrow: megaloblastic appearance
Serum vitamin B12 values lowered (normal 200 – 800 pg/ml)
Serum and red cell folate levels – wide variation in normal range; less than 3 ng/ml -very low, 3-5 ng/ml –low, >5-6 ng/ml normal, in red cell:74-640 ng/ml
Schilling urinary excretion test – measurement of intrinsic factor availability and absorption of vitamin B12
Treatment
Vitamin B12 deficiency
Prevention in cases of risk of vitamin B12 deficiency
Treatment 25 – 100µg vitamin B12
Folic acid deficiency
Correction of the foliate deficiency (100-200 µg/day)
Treatment of the underlying causative disorder
Improvement of the diet to increase folate intake
Megaloblastic Anemia: Causes of
Vitamin B
12
deficiency
Folate deficiency
Drugs
Myelodysplastic syndromes
Acute leukemia
Megaloblastic Anemias:
Deficiency of Vitamin B
12
Vitamin B
12
(cyanocobalamin) deficiency
1.
Inadequate dietary intake a.
B
12 is found in food of animal origin: red meat, fish, poultry, eggs, dairy products
Megaloblastic Anemias:
Deficiency of Vitamin B
12
2.
a.
Malabsorption
Pernicious anemia
Caused by gastric parietal cell atrophy which causes decreased secretion of intrinsic factor (IF). IF is necessary for B
12 absorption.
Atrophy due to immune destruction of the acid-secreting portion of the gastric mucosa
Onset is usually after age 40, primarily women
Affects people of Northern European backgrounds
Neurologic problems
Schilling test used for diagnosis
Schilling test
Establishes the cause of vitamin B
12 deficiency
Test performed in two parts
If parts one & two abnormal: Pernicious anemia
If part one only abnormal: malabsorption
B
12
Malabsorption causes (con’t)
c.
Gastrectomy d.
d.
Blind loop syndrome
bacteria use up the B
12
Fish tapeworm= Diphyllobothrium latum
completes for B
12
Other Causes for B
12
Deficiency
3.
a.
b.
c.
Drugs
Alcohol
Nitrous oxide
Antitubercular drug
Megaloblastic Anemia:
Folic Acid (Folate) deficiency
1.
a.
b.
c.
Inadequate dietary intake
Poverty
Old age
Alcoholism
Megaloblastic Anemia:
Folic Acid (Folate) deficiency
2.
a.
Malabsorption
Ileitis/Crohn’s disease b.
Tropical sprue c.
Blind loop syndrome d.
a.
b.
Nontropical sprue
Gluten-sensitive enteropathy
Childhood celiac disease
Megaloblastic Anemia:
Folic Acid (Folate) deficiency
3.
a.
Increased requirement a.
Pregnancy
There is increased demand during pregnancy and should be supplemented prior to and during pregnancy. Deficiency during pregnancy can cause neural tube defects in utero.
b.
c.
Infancy
Hematologic diseases that involve rapid cellular proliferation such as sickle cell anemia
Hemoglobin values vary with age
Newborn
Infancy
Child
Adolescence
Age
(cord blood)
2-3 months
3-6 months
6-12 months
12-24 months
> 24 months
> 13 years
Hb (gm/dL)
13.8-20.0
MCV= 96 -116
Reticulocytes 3-
7%
9.0 (term)
8.5 (low birth wt.)
9.5
10.0
10.5
11.5
12.0 (female)
13.5 (male)
Differential Diagnosis of Anemia
•Divide into groups by size of cell
Microcytic
(MCV)
Normocytic Macrocytic
Fe-def
Thalassemia
Sideroblastic
Lead toxicity
Hgb
Inborn errors
Copper def.
Acute blood loss
Liver disease
Renal disease
Infiltrated marrow
E TEC
Connective tissue
Aplastic Anemia
Anemia/MDS
Newborn
Liver disease
Hypothyroidism
Splenectomy
Trisomy 21
Reticulocytosis
Aplastic
Atransferrinemia Vit B12/Folat
Differential Diagnosis of Anemia
• Consider increased destruction versus decreased production based on reticulocyte count
Production
Dietary(Fe,B12,Folate)
Aplastic Anemia
Diamond-Blackfan TEC
Bone Marrow infiltrate
Destruction
Hemoglobin
Enzyme defects
Membrane defects
Immune-mediated
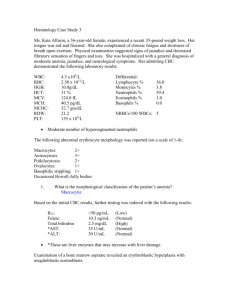
19 mo old male noted by his grandmother to be pale and fussy.
Described as very picky, his diet is mainly string cheese, mac & cheese and milk. The child appears in no distress.
He is slightly tachycardic with normal heart rhythm, no gallop, +systolic murmur, normal BP and good peripheral perfusion. CBC shows Hb=5.0 gm/dl,
MCV 52fL, retic 1.6%.
What is the most appropriate clinical management?
1) Refer immediately to the closest hospital for 10cc/kg PRBC transfusion.
2) Schedule a slow transfusion with 5cc/kg of PRBC then start supplementation with oral iron.
3) Start the patient on a daily children ’s chewable vitamin with Fe.
4) Obtain nutrition consult and start oral Fe at 3-6 mg/kg elemental Fe daily.
Which of the following sets of labs are consistent with iron deficiency anemia?
1) ↑ RDW, ↓ RBC#, ↑ MCV
2) Normal RDW, ↑ RBC#, ↓ MCV
3) ↑ RDW, ↓ RBC#, ↓ MCV
Thal trait vs. Fe-deficiency
•
Remember, in thalassemia trait, all red cells are very small ( ↓ ↓
MCV), but they ’re all the same size (nl RDW), and there is no production problem (nl to ↑ RBC). There is marked discrepancy
between Hgb value and MCV, whereas in Fe-def, these two values tend to go down at a similar rate.