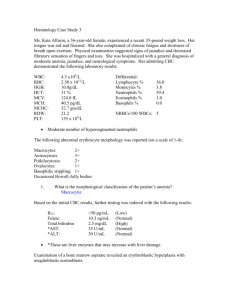
Macrocytic Anemias: Causes, Diagnosis & Findings
advertisement

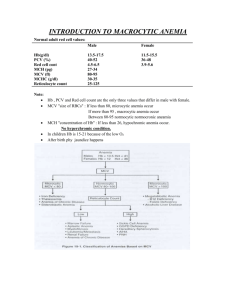
MACROCYTIC ANEMIAS 1. 2. These are the anemias in which the RBC have an MCV of greater than 100fl There are 2 groups of macrocytic anemias Megaloblastic anemia Non megaloblastic macrocytic anemia Requirements for Red Blood Cell Production Erythropoeitin Proteins, required for globin synthesis Iron Vitamin B12 and folic acid Vitamin B6 Vitamin C Thyroid hormones, estrogens and androgens MEGALOBLASTIC ANEMIA These are a group of disorders in which the cause the anemia is due to deficiency of vitamin B12 and folic acid The macrocytes in this condition is usually “oval” - hence they are also called as MACRO OVALOCYTES NON MEGALOBLASTIC MACROCYTIC ANEMIAS These are disorders in which the macrocytosis is not due to vitamin B12 or folic acid deficiency Here the macrocytes are “ROUND” The conditions in which such round macrocytes are seen are 1. Reticulocytosis 2. Hypothyroidism / myxedema 3. Myelodysplastic syndrome 4. Scurvy 5. Sideroblastic anemia 6. Liver disorders Vitamin B12 and folic acid are important nutrients required in the process of nuclear maturation They are required during erythropoiesis during DNA synthesis These anemias may be caused because of a nutritional deficiency or impaired absorption mainly. Impaired DNA synthesis leading to defective cell maturation and cell division Nuclear maturation lags the cytoplasmic maturation – NUCLEAR CYTOPLASMIC ASYNCHRONY Abnormally large erythroid precursors and red cells Affect all marrow elements. 1 Neurologic symptoms (dorsal columns) Ineffective erythropoiesis: High indirect bilirubin Very high LDH Folic Acid: – It is a vitamin which yellow in colour, water soluble, necessary for the production of the RBC, WBC and platelets. – It is not synthesized in the body. – It is found in large number of green fresh vegetables, fruits. Daily requirement: The human body needs about 100-150 µg daily. Absorption: It is absorbed in the Duodenum and Jejunum. Transportation: Weakly bound to albumin. METABOLIC FUNCTION 1. Purine synthesis 2. Conversion of homocysteine to methionine ( which also requires B12 ) 3. Deoxythymidilate synthesis. FOLIC ACID DEFICIENCY 1. INCREASED DEMAND 2. DECREASED INTAKE 3. DECREASED ABSORPTION 4. METABOLIC INHIBITION INCREASED DEMAND Pregnancy Lactation Infancy Puberty and growth period Patients with chronic hemolytic anemias Disseminated cancer DECREASED INTAKE Elderly Lower socio economic status Chronic alcoholics DECREASED ABSORPTION Acidic food substances in foods like legumes, beans Drugs like phenytoin, oral contraceptives 2 Celiac disease which affect the gut absorption Heat sensitive – more loss during cooking METABOLIC INHIBITION VITAMIN B12 This vitamin is synthesized in nature by micro-organism in the intestine of man and animals, but we can not obtain it from the bacteria in our bodies, because it is synthesizing in the large colon after the site of absorption and it is wasted in the faeces in about 5µg/day. So we obtain it from animal food such as liver, kidney, meat and dairy products as milk and cheese. Abundant in animal foods Microorganisms are the ultimate origin of cobalamin It is stored in liver for many years It is efficiently reabsorbed from bile It is resistant to cooking and boiling Diary requirements: The human body needs about 1-2 µg daily. Absorption: B12 is combined with glycoprotein called the intrinsic factor (IF), which is synthesized in the gastric cells. The absorption occurs in the distal ileum. Transportation: Transport by a protein synthesized in the liver called Transcobalamine II, which carry vitamin B12 to liver, nerves and bone marrow. VITAMIN B12 DEFICIENCY 1. INCREASED REQUIREMENT 2. DECREASED INTAKE 3. IMPAIRED ABSORPTION INCREASED DEMAND a. Pregnancy b. Lactation c. Puberty d. Growth period e. Hyperthyroidism f. Disseminated cancer DECREASED INTAKE a. Inadequate intake b. Vegetarian diet IMPAIRED ABSORPTION 3 INTRINSIC FACTOR DEFICIENCY due to chronic gastritis or antibodies against stomach cells. - PERNICIOUS ANEMIA - GASTRECTOMY Malabsorption states Diffuse intestinal diseases. Eg., lymphoma, systemic sclerosis Competitive parasitic uptake – fish tapeworm Bacterial overgrowth CLINICAL FEATURES 1. Patients develop all general symptoms and signs of the anaemia. 2. Knuckle pigmentation 3. Angular stomatitis 4. Atrophic glossitis- “beefy” tongue 5. Neurological disorders: sever deficiency of the folic acid causes neuropathies diseases. 6. Deficiency during pregnancy causes neural tube defect. PERIPHERAL BLOOD FINDINGS 1. Hemoglobin – decreased 2. Hematocrit – decreased 3. RBC count – decreased/normal 4. MCV - >100fl ( normal 82-98fl) 5. MCH –increased 6. MCHC – NORMAL 7. Reticulocytopenia. 8. Total WBC count – normal / low 9. Platelet count – normal/ low 10.Pancytopenia, especially if anaemia is sever. PERIPHERAL SMEAR OR STAINED BLOOD FILM RBC: -Poikilocytosis - tear drops and schistocytes Anisocytosis - oval macrocytes - Macro ovalocytes (macrocytic normochromic) - Well hemogloibised, thicker than normal - Inclusions like HOWELL JOLLY BODIES, basophilic stippling, Cabot rings WBC: Normal count or reduced count Hypersegmented neutrophils (>5 lobes) MACRO POLYMORPHO NUCLEAR CELLS (Macropolys) 4 PLATELETS: Normal or decreased BONE MARROW Markedly hypercellular Myeloid : erythroid ratio decreased or reversed. (Normally, there are three myeloid precursors for each erythroid precursor resulting in a 3:1 ratio, known as the M:E (myeloid to erythroid) ratio) Erythropoiesis : MEGALOBLASTIC MEGALOBLAST 1. Abnormally large precursor 2. Deeply basophilic royal blue cytoplasm 3. Fine chromatin with prominent nucleoli 4. Nuclear cytoplasmic asynchrony 5. Abnormal mitoses 6. Maturation arrest BIOCHEMICAL FINDINGS Increase in serum unconjugated bilirubin- because of ineffective erythropoiesis Increase is LDH Normal serum iron and ferritin TESTS FOR FOLATE AND B12 DEFICIENCY Serum folate assay Red cell folate assay Serum B12 assay PERNICIOUS ANEMIA Scandinavian countries more prevalent Disease of elderly – 5th to 8th decades Genetic predisposition Tendency to form antibodies against multiple self antigens PATHOGENESIS Immunologically mediated, autoimmune destruction of gastric mucosa CHRONIC ATROPHIC GASTRITIS – marked loss of parietal cells Three types of antibodies a) Type I antibody- 75% - blocks vitamin B12 and IF binding b) Type II antibody – prevents binding of IF-B12 complex with ileal receptors c) Type III antibody – 85-90% patients – against specific structures in the parietal cell Associated with other autoimmune diseases like autoimmune thyroiditis 5 DIAGNOSTIC FEATURES 1. Moderate to severe megaloblastic anemia 2. Leucopenia with hypersegmented neutrophils 3. Mild to moderate thrombocytopenia 4. Mild jaundice due to ineffective erythropoiesis and peripheral hemolysis 5. Neurologic changes 6. Low levels of serum B12 7. Elevated levels of homocysteine 8. Striking reticulocytosis after parenteral administration of vitamin B12 9. Serum antibodies to intrinsic factor 6