Ability Based Outcomes Workbook
advertisement
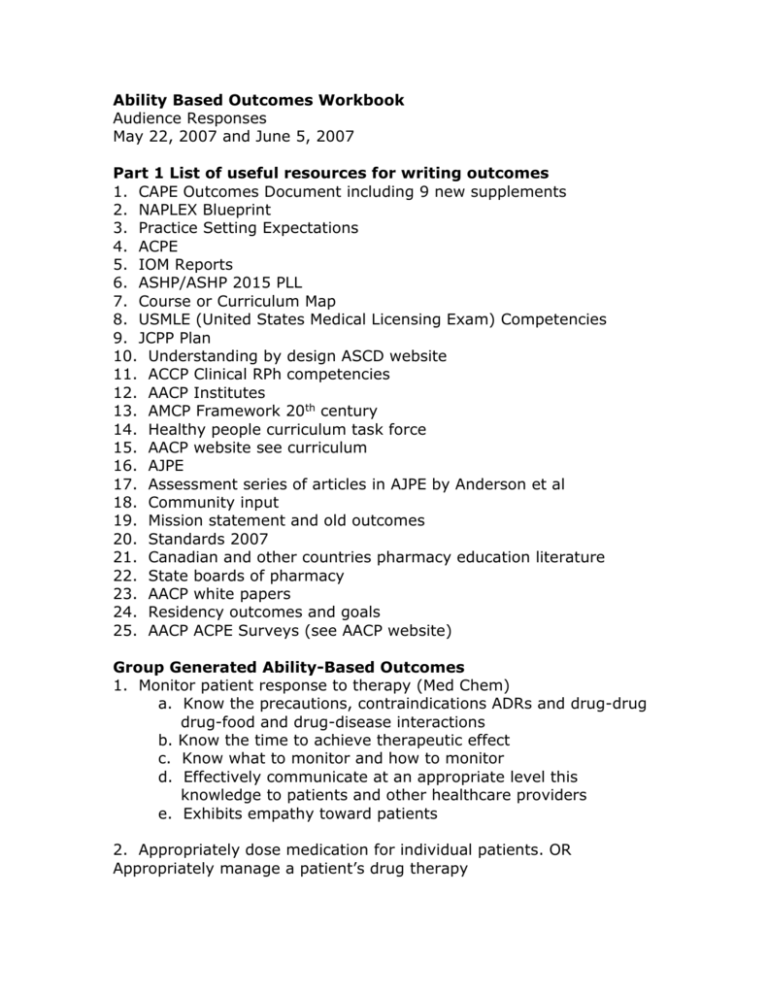
Ability Based Outcomes Workbook Audience Responses May 22, 2007 and June 5, 2007 Part 1 List of useful resources for writing outcomes 1. CAPE Outcomes Document including 9 new supplements 2. NAPLEX Blueprint 3. Practice Setting Expectations 4. ACPE 5. IOM Reports 6. ASHP/ASHP 2015 PLL 7. Course or Curriculum Map 8. USMLE (United States Medical Licensing Exam) Competencies 9. JCPP Plan 10. Understanding by design ASCD website 11. ACCP Clinical RPh competencies 12. AACP Institutes 13. AMCP Framework 20th century 14. Healthy people curriculum task force 15. AACP website see curriculum 16. AJPE 17. Assessment series of articles in AJPE by Anderson et al 18. Community input 19. Mission statement and old outcomes 20. Standards 2007 21. Canadian and other countries pharmacy education literature 22. State boards of pharmacy 23. AACP white papers 24. Residency outcomes and goals 25. AACP ACPE Surveys (see AACP website) Group Generated Ability-Based Outcomes 1. Monitor patient response to therapy (Med Chem) a. Know the precautions, contraindications ADRs and drug-drug drug-food and drug-disease interactions b. Know the time to achieve therapeutic effect c. Know what to monitor and how to monitor d. Effectively communicate at an appropriate level this knowledge to patients and other healthcare providers e. Exhibits empathy toward patients 2. Appropriately dose medication for individual patients. OR Appropriately manage a patient’s drug therapy 3. Identify components of a profit/loss statement for two pharmacy locations/Analyze the data and determine which location performed better/professionally 4. Explain the pathophysiology as it relation to pharmacotherapy of a chronic disease/integrate objective/subjective data in formulating a management plan/demonstrate empathy towards the patient regarding fear (e.g. social stigma mortality guilt) 5. Monitor patient drug regimens for drug interactions Identify potential drug interactions Assess clinical significance of potential interactions Take action in responding to identified drug interactions 6. Recommend drug dosage formulations based on patient therapy needs and characteristics 7. Initiate and adjust drug dosing based on patient and population specific pharmacokinetic parameters 8. Students become life-long learners List appropriate resources for obtaining information Critique information resources Perform literature search Value importance of life-long learning 9. Design/modify drug therapy regimens based on patient specific physiologic conditions 10. Utilize pharmaceutics and biopharmaceutics in the optimal design of pharmacy care Understand the physical-chemical and biological principles of various dosage forms Interpretation of principles in the design of optimal dosage forms Valuing patient specific variables in design and selection of dosage forms 11. Develop a patient-specific plan for the self-monitoring for the prevention of or disease-state management. Know the available self-monitoring devices for screening diagnosis and monitoring Acquire from a patient appropriate information/ select the most appropriate device/ teach the patient how to use the selected device Be sensitive to patient’s needs 12. Intervene with a prescriber on behalf of a patient when an Rx is contraindicated Recognize medications that are contraindicated based on patientspecific data Assertively explain contraindication to a prescriber to effect a constructive change Exhibit compassion and advocacy on behalf of patient 13. Explain the MOA of various drugs to practitioners and patients as it pertains to managing disease states State the MOA and the resulting pharmacologic effects in drugs typically used to treat asthma Select appropriate asthma tx based on the MOA anticipating the adverse effects based on those mechanisms Value the importance of educating patients and providers about the role for the MOA for their asthma (acute v preventive) 14. Recognize and manage drug-interactions based on disease concurrent drug therapy and dietary intake Basic pharmacokinetic principles of ADME Identify drug-drug, drug-disease and drug food interactions. Exhibits a willingness to communicate with health care professionals and patients 15. Make appropriate decisions regarding drug selection process after assessing pathophysiology/organ function. 16. Evaluate drug therapy decisions Understand pharmacologic and therapeutic principles Justify drug selection based on physiochemical properties Exhibit confidence in decision making process 17. Individualize dosing based on patient and medication specific characteristics Knows Pk/Pd parameters of medications Identifies correct formuals and accurately calculates dosing regimen Recognizes value/importance of patient specific dosing 18. Apply principles of drug action in pharmacist-patient care decisions 19. Implement a quality assurance program 20. Recommend drug therapy 21. Evaluate the appropriateness of drug therapy 22. Monitor patients for adverse effects of drugs 23. Resolve a drug-related problem for a specific patient utilizing evidence based medicine 24. Evaluate function and workflow to ensure appropriate allocation of staff time and responsibilities 25. Formulate monitor and adjust a dosage regimen specific to an individual patient Barriers or Key Elements for Success Lack of resources Committee approach Attitude “Why do we need this?” Language Where do we (Pharmacy) fit in to the HC environment overall? Strategic Plan Global view vs course level view Faculty buy-in Limited resources – time, attention, expertise, competing forces Attitude “What is in it for me?” Backwards design Disconnect between faculty in different specialties Shared understanding Preconceived notions A committee must have more than one member Details versus generalities Refining process Attitude “it is not broken” Faculty learning curve Content and time management Turf wars Credit hours = worth of a course Idea that outcomes are a living document Turnover of faculty verbs are important Where are the appropriate levels of Bloom’s taxonomy Depth and breadth of content over time Culture and rewards